Abstract
Choledochal cysts of the cystic duct are extremely unusual and only single case reports are documented in the literature. The widely used Todani classification does not include such type of lesions. We present a case of a young girl with a cystic duct choledochal cyst diagnosed preoperatively and confirmed intraoperatively. Due to the site and mass effect of the cyst, excision of the lesion included a part of bile duct. Reconstruction was achieved by Roux-en-Y hepaticojejunostomy. While such lesions are extremely rare, they do occur and need to be recognized as a separate entity in the Todani classification.
Keywords: Choledochal cyst, Todani’s classification, Type 6 choledochal cyst
Introduction
Choledochal cyst defined as a cystic dilatation of the common bile duct is a rare abnormality, with a reported incidence of 1:100,000 to 150,000 live births [1]. Traditionally, choledochal cysts have been classified into five main types as described by Todani et al.—a modification of the earlier Alonso-Lej classification [2]. Isolated cystic duct cysts are extremely rare lesions with only single case reports in the literature. Here, we describe such a type of isolated dilatation of the cystic duct in a young woman diagnosed on surgical exploration.
Case Report
A 10-year-old female patient presenting with 1 year history of recurrent, upper abdominal pain was admitted in our department. There was no history of fever, jaundice, or weight loss. Physical examination revealed no abnormality except for deep tenderness in the right hypochondrium. Hemogram and blood chemistry were normal. Abdominal ultrasonography (USG) demonstrated a hypoechoic cystic dilatation ( 30 × 25 mm) in the middle of the common bile duct (CBD), without any apparent obstructing lesion and was thus suggestive of a type I choledochal cyst. Coronal magnetic resonance cholangiopancreatogram (MRCP) revealed a fusiform dilatation (30 × 25 mm) in the cystic duct with its low insertion into the CBD (Fig. 1). The right and left hepatic ducts, intrahepatic biliary ducts, and the main pancreatic duct were normal and no abnormal pancreaticobiliary ductal junction union was detected. A preoperative diagnosis of an isolated cyst duct cyst was thus made and the patient was planned for surgery.
Fig. 1.
Coronal image of magnetic resonance cholangiopancreatography (MRCP) revealing isolated cystic duct dilatation (CD) with its low insertion into the common bile duct (CBD). GB, gall bladder; CHD, common hepatic duct
On surgical exploration, a spherical cystic lesion (30 × 25 mm) was detected at the junction of cystic duct with the CBD (Fig. 2). The CBD was 7 mm in diameter and was displaced medially due to the mass effect of cystic lesion. Further dissection separated the cyst from the common hepatic duct. However, due to presence of a wide opening of the cystic lesion into the CBD, excision of the lesion by simple transection of cystic duct at its junction with CBD was not considered feasible. Therefore, cholecystectomy with a total excision of the cystic lesion along with part of common hepatic duct and common bile duct was performed. Reconstruction was achieved by Roux-en-Y hepaticojejunostomy. Histopathological examination of the gallbladder and the cyst revealed chronic cholecystitis and cystic duct cyst, respectively, with evidence of acute inflammation.
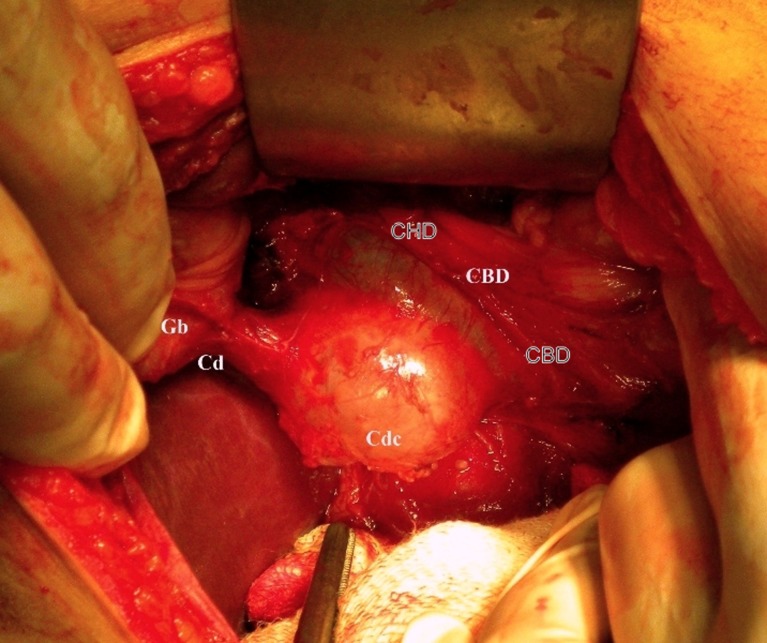
Fig. 2.
Operative photograph demonstrating a cystic duct cyst (Cdc) causing mass effect on the common bile duct (CBD). Gb, gall bladder, Cd, cystic duct, CHD common hepatic duct
Discussion
Choledochal cyst is defined as a cystic dilatation of the biliary ductal system. Although these cysts are rare, cystic lesions of the cystic duct are even rarer. Traditionally, the widely accepted and used classification of Alonso-Lej et al., as modified by Todani et al. [2], does not include the cystic lesions of the cystic duct as a separate entity. It was Serena Serradel et al. [3] who proposed for inclusion of such type of cysts as type 6 lesions in the Todani’s classification. A search in the medical literature reveals that less than 15 such cases have been reported till date [3–12]. As reported from the previous cases (Table 1), the common symptoms of the cystic duct lesions includes epigastric and/or right upper quadrant pain which is usually exaggerated by a fatty meal [11]. In our patient, the main feature was pain in the upper abdomen which got aggravated by intake of fatty food. However, an obstruction of the common bile duct may develop because of mass effect by the cyst [5] or due to inflammation resulting from cholangitis [8]. A precise recognition of the extent of the choledochal cyst is crucial before surgery. Abdominal ultrasonography is a good initial screening method; endoscopic retrograde cholangiopancreatography defines the biliary anatomy in detail including the abnormal pancreatobiliary junction. Nevertheless, it is an invasive technique. MRCP is highly effective and noninvasive method for evaluating the biliary tree.
Table 1.
Clinical profile of reported cases of cystic duct cysts
| References | Presentation | Investigation | Preoperative diagnosis | Operative treatment | Outcome |
|---|---|---|---|---|---|
| Chan et al. [11] | Incidental | CT scan, MRCP | Type II choledochal cyst | Cyst excision with cholecystectomy | Good |
| Serena Serradel et al. [3] | Pain in the epigastrium | USG, ERCP | Type II choledochal cyst | Cyst excision with cholecystectomy | Good |
| Bode et al. [5] | Obstruction | USG, HIDA scan, PTC | Type II choledochal cyst | Cyst excision with cholecystectomy with choledochoduodenostomy | Good |
| Conway et al. [12] | Pain right upper abdomen | CT scan, USG, HIDA scan | Choledochal cyst | Cyst excision with cholecystectomy | Good |
| Loke et al. [8] | Jaundice with acute cholangitis | USG, ERCP | Mirizzi’s syndrome | Cyst excision with cholecystectomy and Roux-en-Y choledochojejunostomy | Good |
| Baj et al. [9] | Pain in the right upper abdomen | USG, CT oral cholangiography | Cystic duct cyst (choledochocele) | Patient refused surgical treatment | Not known |
| Bresciani et al. [4] | Pain in the right upper abdomen | USG | Chronic cholecystitis | Video laparoscopic excision of the cyst with cholecystectomy | Good |
| Manickam et al. [10] | Pain in the upper abdomen | USG, HIDA scan, CT scan, MRCP | Cystic duct cyst with APBDJU | Excision of the cyst with cholecystectomy | Good |
| Shah et al. (present case) | Pain in the upper abdomen | USG, MRCP | Cystic duct cyst | Cyst excision, cholecystectomy and Roux-en-Y hepaticojejunostomy | Good |
The anatomical similarity between type 2 choledochal cyst and cystic duct cyst has been reported on before; both Serena Serradel et al. [3] and Bode and Aust [5] initially misdiagnosed their cases as type 2 choledochal cysts and Loke et al. [8] also mentioned that their case resembled a type 2 choledochal cyst. In such circumstances, one has to depend purely on operative findings and high index of suspicion for the possibility of existence of such a lesion. Bresciani et al. [4] stressed on performing the intraoperative cholangiogram for localizing the lesion.
The recommended surgical treatment for cystic duct cysts is cholecystectomy with excision of the cyst and transection of the cystic duct [3, 5]. However in some cases [8], as was in our case, the cystic duct junction with the common bile is quite wide and as such necessitates excision of part of common bile duct and thus a Roux-en-Y hepaticojejunostomy may be performed. Use of an isolated conduit of proximal jejunum interposed between common hepatic duct and the remaining part of distal CBD for bridging the gap between the common hepatic duct and duodenum after cyst excision is a reasonably good alternative. Recently, Bresciani et al. [4] and Chan et al. [11] have reported the laparoscopic management of the cystic duct cysts. With better understanding of this type of pathology and the advancements made at diagnostic level, more and more such cases may be reported in future. In conclusion, we report an unusual case of a cystic duct cyst. The preoperative diagnostic challenge may need the change in the angle of acquisition which performing an MRCP and we also suggests for inclusion of this type of a cyst as separate entity in the various classifications of choledochal cysts.
References
- 1.Yamaguchi M. Congenital choledochal cyst. Analysis of 1, 433 patients in the Japanese literature. Am J Surg. 1980;140(5):653–657. doi: 10.1016/0002-9610(80)90051-3. [DOI] [PubMed] [Google Scholar]
- 2.Todani T, Watanabe Y, Narusue M. Congenital bile duct cysts. Classification, operative procedures and review of 37 cases including cancer arising from choledochal cyst. Am J Surg. 1977;134(2):263–260. doi: 10.1016/0002-9610(77)90359-2. [DOI] [PubMed] [Google Scholar]
- 3.Serena Serradel AF, Santamaria LE, Herrera GR (1991) Cystic dilatation of the cystic duct: a new type of biliary cyst. Surgery 109(3Pt 1):320–322 [PubMed]
- 4.Bresciaini C, Gama-Rodrigues J, Santos VR. Video-laparoscopic treatment of a sizeable cyst of the cystic duct. Surg Lap and Endosc. 1998;8(5):376–379. doi: 10.1097/00019509-199810000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Bode WE, Aust JB. Isolated cystic dilation of the cystic duct. Am J Surg. 1983;145(6):828–829. doi: 10.1016/0002-9610(83)90152-6. [DOI] [PubMed] [Google Scholar]
- 6.Kise Y, Uetsiji S, Takada H, Yamamura M, Yamamoto M. Dilatation of the cystic duct with its congenital low entry into the common hepatic duct. Am J Gastroenter. 1990;85(6):769–770. [PubMed] [Google Scholar]
- 7.Benhidjeb T. Cystic duct cyst. Surgery. 1994;116(3):597–598. [PubMed] [Google Scholar]
- 8.Loke TKL, Lam SH, Chan CS. Choledochal cyst an unusual type of cystic dilatation of the cystic duct. Am J Roentgen. 1999;173(3):619–620. doi: 10.2214/ajr.173.3.10470889. [DOI] [PubMed] [Google Scholar]
- 9.Baj M, Sengupta S, O’ Donnell LJD. Choledochocele of the cystic duct; a case report. Internet J Gastroenterol. 2001;1(2):1. [Google Scholar]
- 10.Manickam S, Ramadan K, Adams BK. A rare choledochal cyst of the cystic duct with an anomalous pancreaticobiliary union in an adult patient. Clin Rad Extra. 2004;59:68–71. doi: 10.1016/j.cradex.2004.04.001. [DOI] [Google Scholar]
- 11.Chan ES, Auyang ED, Hungners ES. Laparoscopic management of a cystic duct cyst. JSLS. 2009;13(3):436–440. [PMC free article] [PubMed] [Google Scholar]
- 12.Conway WC, Telian SH, Wasif N, Gangandeep S. Type VI biliary cyst: report of a case. Surgery Today. 2009;39(1):77–79. doi: 10.1007/s00595-008-3789-4. [DOI] [PubMed] [Google Scholar]