Abstract
Background
Prior data suggest that opportunities in family planning training may be limited during obstetrics and gynecology (Ob-Gyn) residency training, particularly at faith-based institutions with moral and ethical constraints, although this aspect of the Ob-Gyn curriculum has not been formally studied to date.
Objectives
We compared Ob-Gyn residents' self-rated competency and intentions to provide family planning procedures at faith-based versus those of residents at non-faith-based programs.
Methods
We surveyed residents at all 20 Ob-Gyn programs in Illinois, Indiana, Iowa, and Wisconsin from 2008 to 2009. Residents were queried about current skills and future plans to perform family planning procedures. We examined associations based on program and residents' personal characteristics and performed multivariable logistic regression analysis.
Results
A total of 232 of 340 residents (68%) from 17 programs (85%) returned surveys. Seven programs were faith-based. Residents from non-faith-based programs were more likely to be completely satisfied with family planning training (odds ratio [OR] = 3.4, 95% confidence limit [CI], 1.9–6.2) and to report they “understand and can perform on own” most procedures. Most residents, regardless of program type, planned to provide all surveyed family planning services.
Conclusions
Despite similar intentions to provide family planning procedures after graduation, residents at faith-based training programs were less satisfied with their family planning training and rate their ability to perform family planning services lower than residents at non-faith-based training programs.
What was known
Obstetrics and gynecology residents' perceptions of their family planning training based on institutional constraints and whether this affects their intentions to provide these services has not been studied to date.
What is new
Residents at faith-based training programs were less satisfied with their family planning training and rated their ability to perform family planning services lower than residents at non-faith-based training programs.
Limitations
Regional survey, with limited ability to generalize, self-reported data, and potential selection effects.
Bottom line
Institutional constraints may affect Ob-Gyn residents' training experience and their subsequent provision of women's healthcare services.
Introduction
Obstetrics and gynecology (Ob-Gyn) residency education must prepare trainees to become experts in all aspects of women's healthcare, including the prevention and treatment of unplanned pregnancies. The American Congress of Obstetricians and Gynecologists (ACOG) and the Council of Residency Education for Obstetrics and Gynecology (CREOG) support family planning education and abortion residency training.1,2 Since 1996, the Accreditation Council for Graduate Medical Education (ACGME) specifies “If an [obstetrics and gynecology] residency program has a religious, moral, or legal restriction that prohibits the residents from providing abortions within the institution, the program must ensure that the residents receive satisfactory education and experience in managing the complications of abortion.”3 In an effort to improve Ob-Gyn residency family planning and abortion training, a privately funded national initiative called the Ryan Program4 was started in 1999 to provide funding and technical expertise to Ob-Gyn departments in the United States, Puerto Rico, and Canada. The Ryan Program has successfully integrated formal family planning training at 67 of 243 Ob-Gyn residency training programs in the United States and Puerto Rico (personal communication with the Ryan Program National Office, March 13, 2013).
Survey data, however, demonstrate limited Ob-Gyn residency training opportunities in family planning, particularly at faith-based institutions with moral and ethical constraints.5–8 A qualitative study that explored Ob-Gyn residency abortion training opportunities cited antiabortion values, including religious associations, as one barrier to training.9 We found no reports in the literature of residents' perception of family planning training, particularly at faith-based programs and whether this affects their future intentions to provide such care. We hypothesized that midwestern Ob-Gyn residents at faith-based and non-faith-based training programs will differ in their perceived ability to perform family planning procedures and their plans to provide family planning procedures after graduation.
Methods
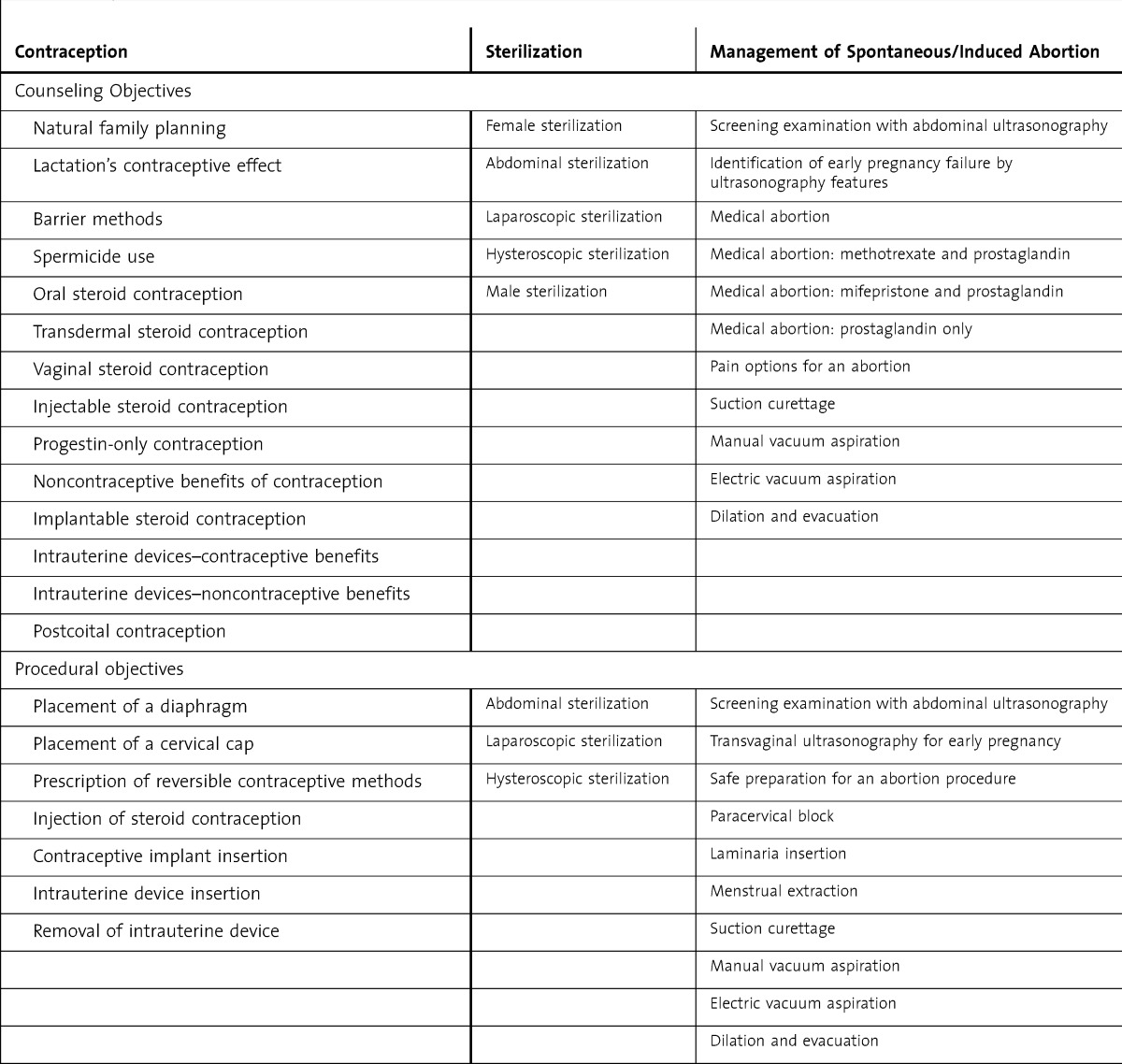
We developed a comprehensive list of family planning patient care activities (table 1) consisting of 30 counseling and 21 procedural objectives based on CREOG educational objectives,2 the Ryan Program's publicly available curriculum,4 and a comprehensive family planning residency curricula from a university Ob-Gyn training program.10 We then developed an anonymous survey to assess residents' self-reported competency and intentions to counsel and perform these procedures.
Table 1.
List of Survey Items
The survey queried residents about personal characteristics and level of satisfaction with their family planning training (satisfied; would not make any changes; somewhat satisfied; would like more elements included; unsatisfied). For each of the counseling objectives, residents were asked if they were able to discuss with their patients the advantages, disadvantages, and failure rates, using a 4-point Likert scale (1 = strongly disagree; 2 = disagree; 3 = agree; 4 = strongly agree). For the procedural objectives, residents assessed their ability to perform the listed procedures by using a 4-point Likert scale (1 = do not understand and cannot perform; 2 = understand but cannot perform; 3 = understand and can perform with help; 4 = understand and can perform on own). We also queried participants about their intentions to counsel or perform the procedures/services following graduation, using a 3-point Likert scale (1 = will not counsel/provide; 2 = may counsel/provide; 3 = will counsel/provide). We initially piloted the survey with 4 medical students and then revised it to enhance clarity.
We distributed this cross-sectional survey during the 2008–2009 academic year to all current 20 midwestern Ob-Gyn programs in Illinois, Indiana, Iowa, and Wisconsin. At each program, a single individual distributed and collected the surveys; that individual was either a residency coordinator or a current resident, fellow, or attending. Based on a review of the program's online website, we collected program characteristics, including faith-based affiliation, number of residents, affiliation with a university program, and presence of a dedicated family planning rotation and/or Ryan program. The program coordinator confirmed and supplemented missing information. Institutional review board approval was received at Loyola University Medical Center.
We analyzed data using SPSS version 18.0 software (SPSS, Chicago, IL). We dichotomized resident satisfaction with their family planning training into satisfied versus somewhat satisfied/unsatisfied. We dichotomized the ability to counsel as strongly agree/agree versus strongly disagree/disagree and the ability to perform as “understand and can perform on own” versus all other responses. We dichotomized plans to counsel or perform following graduation as will or may counsel/provide versus will not counsel/provide. We imputed missing outcome data for ability to perform by using mean program substitution. We reviewed descriptive statistics and examined associations based on personal and program characteristics using a Fisher exact test and Pearson χ2 test. We performed multivariable logistic regression and included program type and any personal variables associated with the outcome in univariable analyses at a P value of < .2.
Results
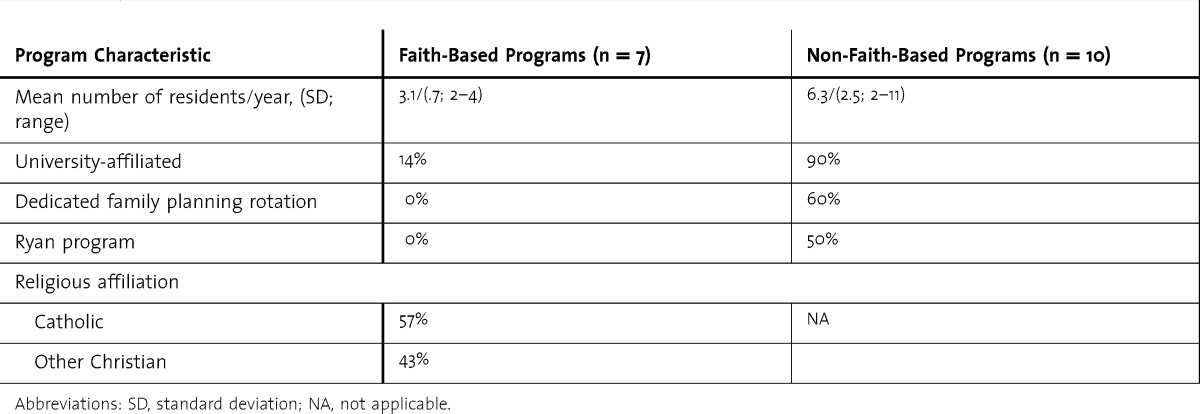
We received surveys from 17 Ob-Gyn residency training programs (85% program response rate) representing all of the states we surveyed. Seven of these programs had a faith-based affiliation (figure). Table 2 describes program characteristics: Non-faith-based programs trained more residents, were more often affiliated with a university program, and were more likely to have a dedicated family planning rotation and/or Ryan program.
FIGURE 1.
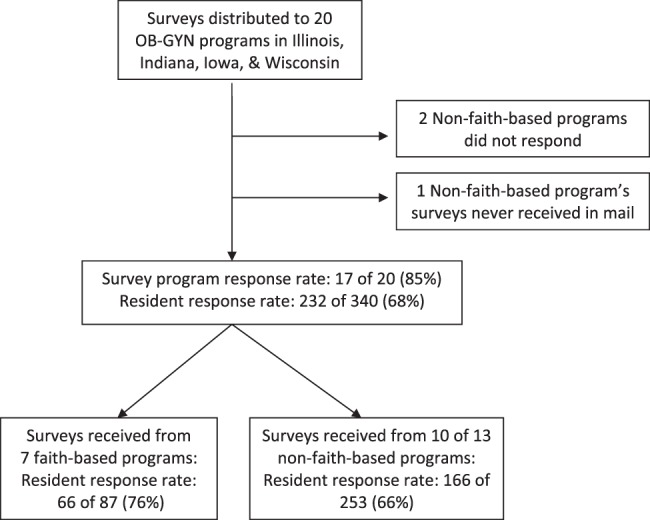
Study Flow Diagram
Table 2.
Program Characteristics by Program Type
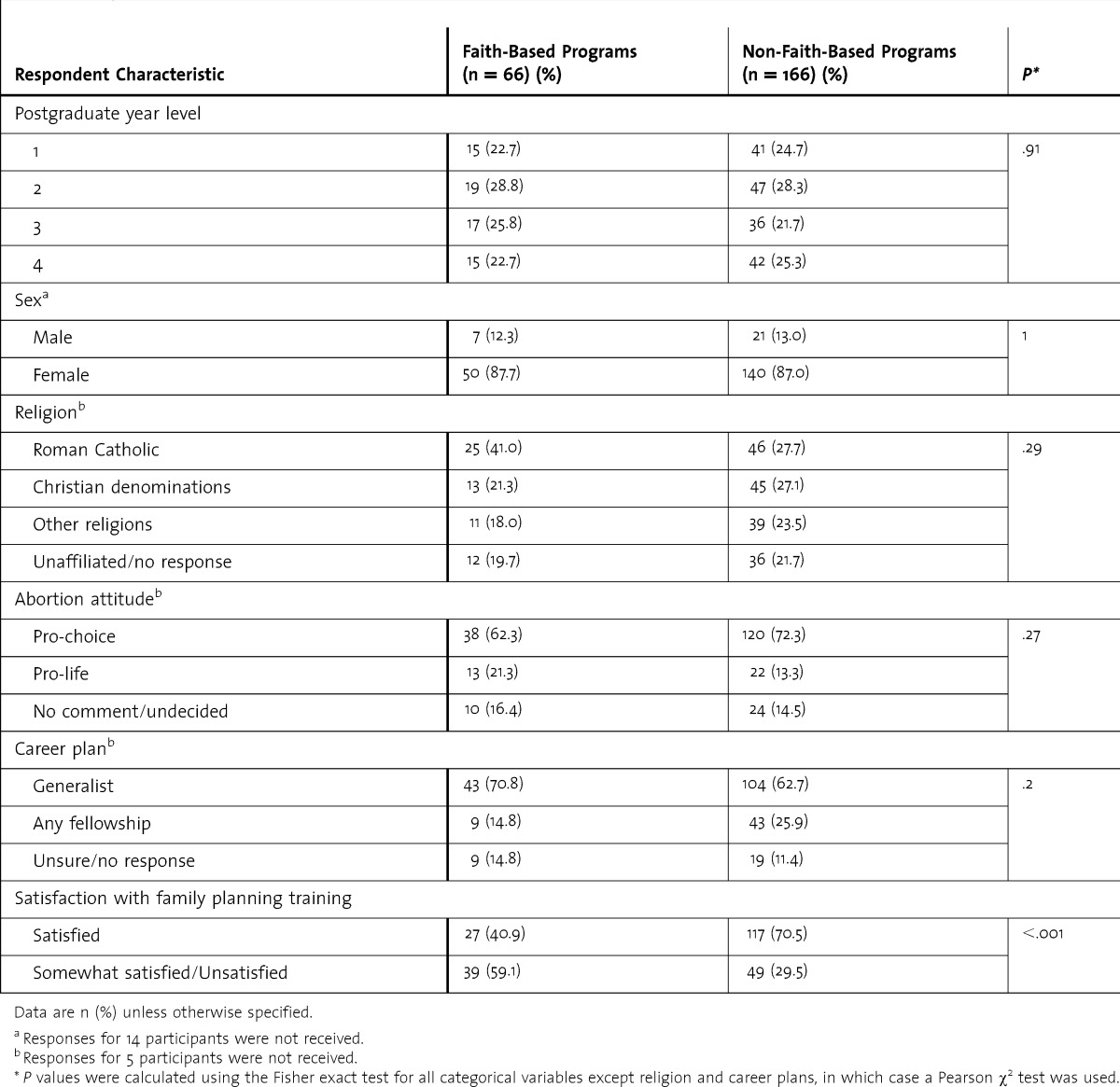
We received 232 resident surveys from the 17 programs that participated, accounting for a 68% resident response rate. There were no differences based on program type (P = .08). Table 3 demonstrates respondents' personal characteristics. Most respondents, regardless of program type, reported they were female, Roman Catholic, pro-choice, and planned on practicing general Ob-Gyn. The only difference we found in respondent characteristics based on program type was in relation to satisfaction with family planning training; residents at non-faith-based programs were 3.4 times more likely (95% confidence interval, 1.9–6.2) to report feeling completely satisfied than residents at faith-based programs.
Table 3.
Summary of Respondents' Personal Characteristics by Program Type
Survey responses about the listed counseling objectives were overall high: the average response rate for ability to counsel was 88% and 95% for plans to counsel. No further analysis was performed for the counseling objectives given high response rates. For procedural objectives, we focused analysis on self-reported performance competency and intentions to provide 10 family planning procedures, grouped into the 4 following categories: (1) long-acting reversible contraception (insertion of intrauterine device [IUD], placement of implantable contraception); (2) interval sterilization (laparoscopic sterilization, hysteroscopic sterilization); (3) first-trimester uterine evacuation techniques (suction curettage, manual vacuum aspiration [MVA], electric vacuum aspiration [EVA] and paracervical block); and (4) second-trimester uterine evacuation techniques (laminaria placement, dilation and evacuation [D&E]). We eliminated the remainder of the procedural objectives for reasons such as not commonly performed, little technical skill needed, or outdated procedure.
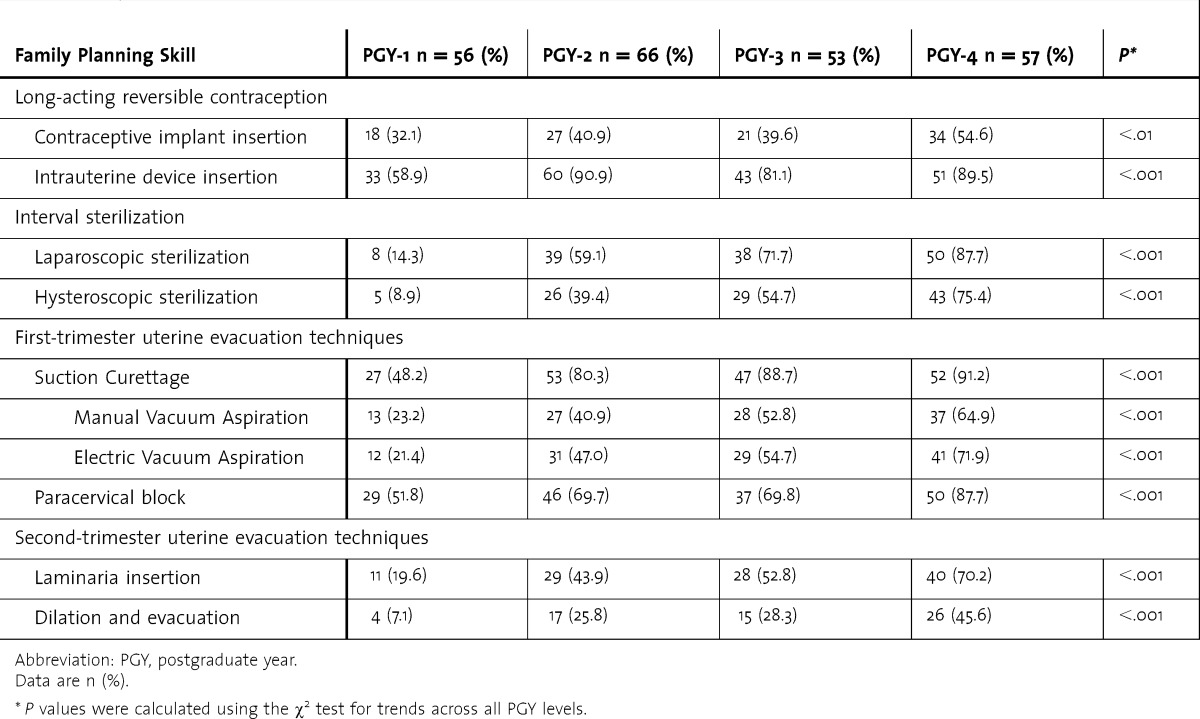
Table 4 demonstrates overall response rates for ability to perform and according to 3 program characteristics (non-faith-based affiliation, dedicated family planning rotation, and Ryan training program). Overall, more residents felt that they could insert an IUD or perform laparoscopic sterilization “on their own” as compared to implantable contraception insertion or hysteroscopic sterilization performance. The majority of residents felt competent performing suction curettage (77%), while a much smaller percentage (27%) reported they felt they could perform D&E. Residents at non-faith-based programs reported higher rates of competency for the most of the surveyed procedures. Findings were similar for residents at programs with a dedicated rotation or Ryan training program. As residents progressed through their training, they reported increasing levels of competency (table 5).
Table 4.
Residents Reporting They “Understand and Can Perform on Their Own” by Program Type
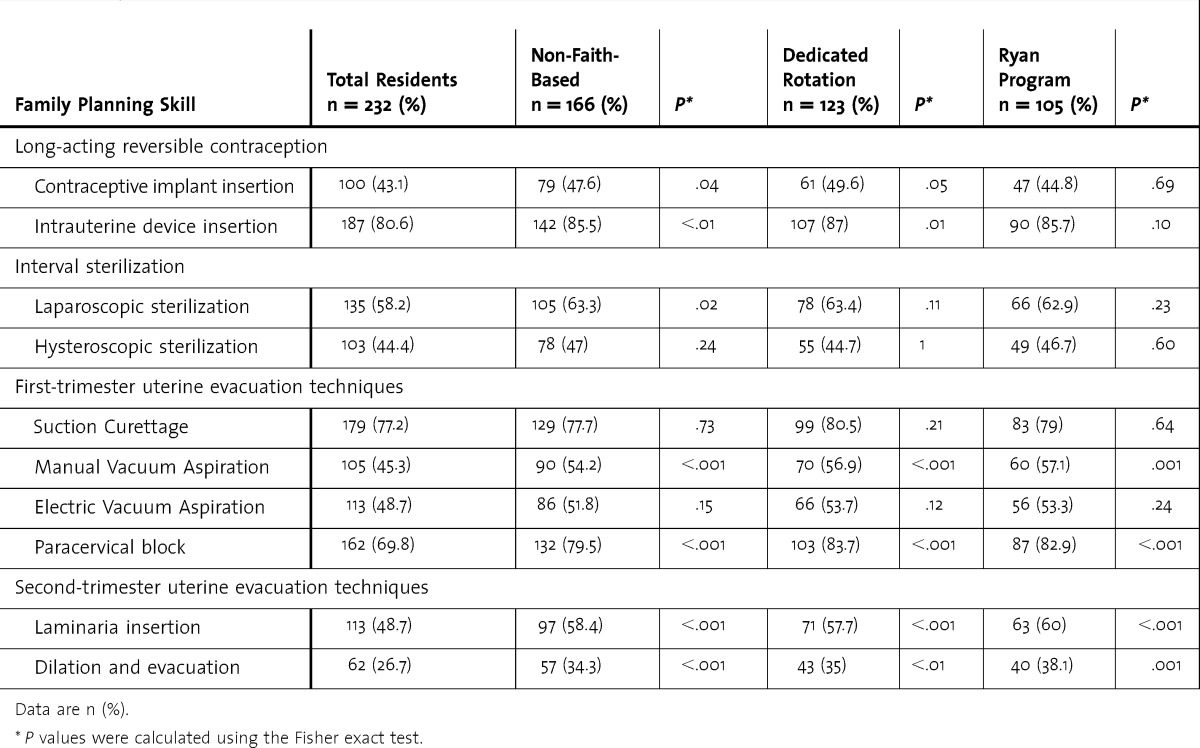
Table 5.
Residents Reporting They “Understand and Can Perform on Their Own” by PGY Level*
To examine our primary hypothesis, we performed multivariable regression analysis to control for any potential confounders. We included faith-based association as the only program characteristics given the overlap with other characteristics, such as rotation or Ryan program. For all multivariable models, we entered year of training and then entered abortion attitude and/or personal religion if it was found to be significant in bivariate analysis (P < .2). Gender and career plans were not significantly correlated with any of the procedures and were not entered into any of the models. For all examined procedures, differences between faith-based and non-faith-based program respondents persisted.
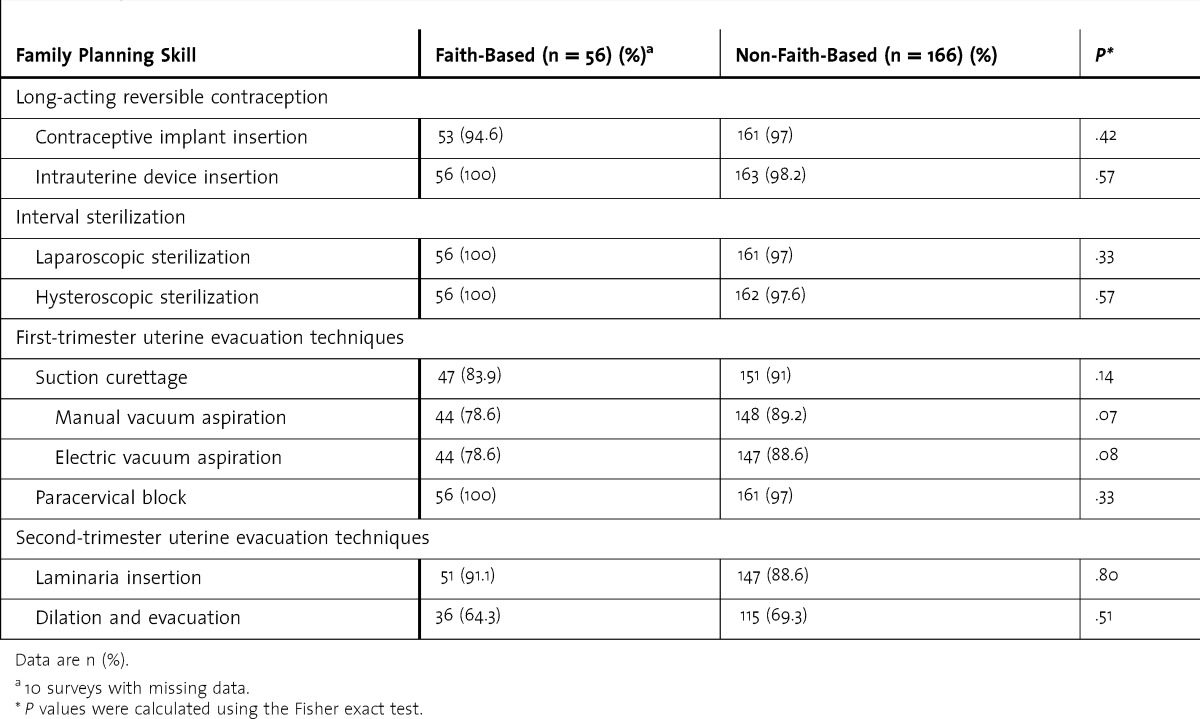
The majority of residents planned to perform all of the listed family planning procedures, including D&E (68%). Table 6 demonstrates responses for residents' plans to perform specific procedures; there were no differences based on program type.
Table 6.
Residents Reporting They “Will Provide” or “May Provide” by Program Type
Discussion
Our survey highlights the fact that satisfaction with family planning training and self-rated ability to perform family planning procedures appear to be lower for residents at faith-based training programs. Despite program type differences in reported competency, residents who match at faith-based programs do not appear to differ in the type of care they plan to provide to their patients. Although residents at faith-based institutions were 5 times less likely to feel competent at performing D&E, over 68% of all residents planned to provide D&E regardless of where they received their training.
Differences in training are likely to impact the provision of care that residents provide following graduation. Physicians who provide abortion care in practice are more likely to have received abortion training during their residency.11–13 Experience with abortion during training also impacts the provision of other aspects of gynecologic care following graduation. For instance, in a survey of 308 practicing Ob-Gyns, Dalton and colleagues13 found that induced abortion residency training was associated with the subsequent use of office-based uterine evacuation for early pregnancy failures. This is consistent with our findings that residents from non-faith-based programs reported higher rates of competency with MVA and paracervical block, first-trimester uterine evacuation techniques that are more commonly performed in the outpatient setting. These training differences may also impact healthcare costs; when effective contraception is offered and uterine evacuation is performed in the outpatient setting, they are more cost-effective than in the inpatient setting.14–16
There are limitations to this regional survey. The results may not be generalizable to residents training outside of the Midwest. Applicants for Ob-Gyn residency interested in abortion training may have preferentially applied to and ranked non-faith-based programs that provide training. We did not provide an explanation for the surveyed procedures, so some residents, particularly those without training, may not have been familiar with them. For example, more residents were familiar with suction curettage than specific types such as manual or electric vacuum aspiration. We also did not specify indications for procedures; certain residents may be willing to provide evacuation services for certain indications. We used a self-reported measure of procedural skills, which may be inaccurate, although prior investigators reported that Ob-Gyn residents if anything, rated themselves lower than faculty observers.17 A more valid description of procedural competence would need external assessments such as case logs or external evaluations blinded to program type. We found lower reported competence rates within the entire cohort for newer methods, such as implant insertion and hysteroscopic sterilization, and greater reported competence among the upper-year residents, suggesting that our measure of exposure to the procedures has some validity.
Finally, it is possible that there are explanations other than faith-based affiliation to explain the disparities we noted. We did not assess whether residents felt less satisfied or competent about other aspects of Ob-Gyn care. For example, the faith-based programs in our study tended to be smaller community programs and, thus, may have lacked resources and/or exposure to adequate patient volumes. The presence of a dedicated rotation and/or Ryan training program was assessed and appeared to reflect some of the differences we found. While these may be considered underlying factors for training differences, it is important to note that none of the faith-based programs had a dedicated rotation or Ryan program, likely secondary to institutional considerations.
There are consistent guidelines from ACOG and CREOG that recognize that all Ob-Gyn programs should expose their residents to comprehensive family planning training. We recognize that given institutional constraints, faith-based programs are often unable to provide family planning services and train their residents on-site. Such programs may consider dedicated family planning educational sessions18 and/or collaboration with off-site providers to train their residents. Electronic-learning (E-learning) family planning courses may also help complement training curricula. We anticipate that improving reproductive health care education, particularly at faith-based programs, will have lasting impacts on patient care. Improving residency training may impact how confident graduating residents, regardless of their personal moral values, feel about providing family planning services.
Conclusion
Our findings reflect the impact of institutional constraints on Ob-Gyn residents' training experience and their provision of women's healthcare services. Despite similar intentions to provide family planning procedures after graduation, residents at faith-based training programs were less satisfied with their family planning training and rated their ability to perform family planning procedures lower than residents at non-faith-based training programs.
Footnotes
Maryam Guiahi, MD, MSc, is Assistant Professor in the Department of Obstetrics and Gynecology, University of Colorado Anschutz Medical Campus; Carolyn L. Westhoff, MD, MSc, is Professor in the Division of Family Planning and Preventive Services, Department of Obstetrics and Gynecology, Columbia University; Sondra Summers, MD, is Associate Professor in the Department of Obstetrics and Gynecology, Stritch School of Medicine, Loyola University; and Kimberly Kenton, MD, MS, is Professor in Obstetrics & Gynecology and Urology, Northwestern University Feinberg School of Medicine.
Funding: The authors report no external funding source for this study.
This work was presented orally at the Council on Resident Education in Obstetrics and Gynecology and Association of Professors in Gynecology and Obstetrics Annual Meeting, Orlando, FL, March 9, 2012, and was awarded second place for oral presentations.
References
- 1.ACOG Committee Opinion No. 424: abortion access and training. Obstet Gynecol. 2009;113(1):247–250. doi: 10.1097/AOG.0b013e318196426c. [DOI] [PubMed] [Google Scholar]
- 2.Council on Resident Education in Obstetrics and Gynecology. Educational Objectives: Core Curriculum in Obstetrics and Gynecology. 8th ed. Washington DC: CREOG; 2005. [Google Scholar]
- 3.Accreditation Council for Graduate Medical Education. Obstetrics/gynecology program requirements. http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/220obstetricsandgynecology01012008.pdf. Accessed April 8, 2013. [Google Scholar]
- 4.Kenneth J. Ryan Residency Training Program in Abortion and Family Planning. http://www.ryanprogram.org. Accessed March 23, 2011. [DOI] [PubMed] [Google Scholar]
- 5.Westhoff C, Marks F, Rosenfield A. Residency training in contraception, sterilization, and abortion. Obstet Gynecol. 1993;81(2):311–314. [PubMed] [Google Scholar]
- 6.Almeling R, Tews L, Dudley S. Abortion training in US obstetrics and gynecology residency programs, 1998. Fam Plann Perspect. 2000;32(6):268–271. [PubMed] [Google Scholar]
- 7.Eastwood KL, Kacmar JE, Steinauer J, Weitzen S, Boardman LA. Abortion training in United States obstetrics and gynecology residency programs. Obstet Gynecol. 2006;108(2):303–308. doi: 10.1097/01.AOG.0000224705.79818.c9. [DOI] [PubMed] [Google Scholar]
- 8.MacKay HT, MacKay AP. Abortion training in obstetrics and gynecology residency programs in the United States, 1991–1992. Fam Plann Perspect. 1995;27(3):112–115. [PubMed] [Google Scholar]
- 9.Guiahi M, Lim S, Westover C, Gold M, Westhoff CL. Enablers and barriers of abortion training. J Grad Med Educ. 2013;5(2):238–243. doi: 10.4300/JGME-D-12-00067.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Guiahi M, Hruska L, Summers S, Kenton K. Developing a comprehensive family planning obstetrics and gynecology residency curriculum: a comparison of three family planning curriculum. Contraception. 2008;78:186. [Google Scholar]
- 11.Shanahan MA, Metheny WP, Star J, Peipert JF. Induced abortion. Physician training and practice patterns. J Reprod Med. 1999;44(5):428–432. [PubMed] [Google Scholar]
- 12.Steinauer J, Landy U, Filippone H, Laube D, Darney PD, Jackson RA. Predictors of abortion provision among practicing obstetrician-gynecologists: a national survey. Am J Obstet Gynecol. 2008;198(1):39.e31–36. doi: 10.1016/j.ajog.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 13.Dalton VK, Harris LH, Bell JD, et al. Treatment of early pregnancy failure: does induced abortion training affect later practices. Am J Obstet Gynecol. 2011;204(6):493.e1–6. doi: 10.1016/j.ajog.2011.01.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Cowett AA, Golub RM, Grobman WA. Cost-effectiveness of dilation and evacuation versus the induction of labor for second-trimester pregnancy termination. Am J Obstet Gynecol. 2006;194(3):768–773. doi: 10.1016/j.ajog.2005.09.003. [DOI] [PubMed] [Google Scholar]
- 15.Blumenthal PD, Remsburg RE. A time and cost analysis of the management of incomplete abortion with manual vacuum aspiration. Int J Gynaecol Obstet. 1994;45(3):261–267. doi: 10.1016/0020-7292(94)90252-6. [DOI] [PubMed] [Google Scholar]
- 16.Trussell J, Lalla AM, Doan QV, Reyes E, Pinto L, Gricar J. Cost effectiveness of contraceptives in the United States. Contraception. 2009;79(1):5–14. doi: 10.1016/j.contraception.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mandel LS, Goff BA, Lentz GM. Self-assessment of resident surgical skills: is it feasible. Am J Obstet Gynecol. 2005;193(5):1817–1822. doi: 10.1016/j.ajog.2005.07.080. [DOI] [PubMed] [Google Scholar]
- 18.Guiahi M, Cortland C, Graham MJ, et al. Addressing OB/GYN family planning educational objectives at a faith-based institution using the TEACH program. Contraception. 2011;83(4):367–372. doi: 10.1016/j.contraception.2010.07.012. [DOI] [PubMed] [Google Scholar]


