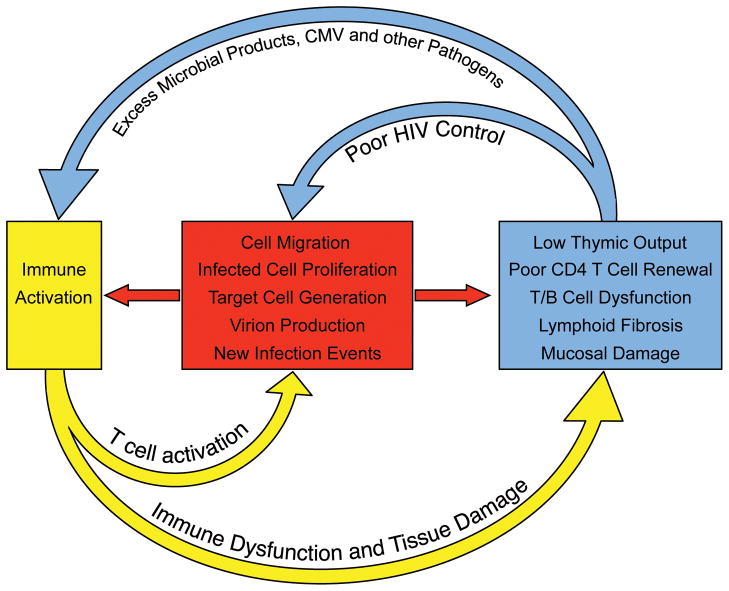
Fig. 2. Immune activation sustains HIV persistence during antiretroviral therapy.
HIV-associated damage to the lymphoid system is only partially reversible. During long-term antiretroviral therapy, the residual immune dysfunction (which is due in part to loss of thymic tissue, fibrosis in germinal centers of secondary lymphoid structure, hematopoietic stem cell loss, and mucosal barrier breakdown) results in immunodeficiency, excess amounts of pathogens and chronic immune activation. The immune activation in turn leads to migration of CD4+ T cells to foci of HIV replication, generation of activated and susceptible target cells, and production of virus from latently infected cells (all of which enable more efficient cell-to-cell spread of HIV and replenishment of infected cells). The inflammatory environment also leads to proliferation and maintenance of latently infected cells. The residual HIV replication/production in turn contributes to sustained tissue damage and immune activation.