Fig. 8.
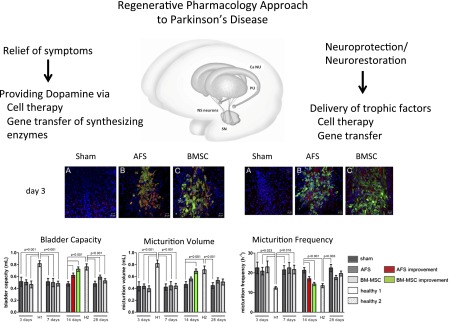
Regenerative pharmacology approaches to Parkinson’s disease. Functional analysis of preclinical cell therapy approach to one PD endpoint, namely, bladder dysfunction or overactivity. Top left and right panels show immunofluorescence (red) for superoxide dismutase-2 (SOD-2; A–C, left) and interleukin-6 (IL-6; A–C, right), respectively, in rat brain cells surrounding and in close contact to amniotic fluid derived stem cells (AFS) or BM-MSC (bone marrow-mesenchymal stem cell; both stem cell populations were green fluorescent protein labeled and green) injected into a unilateral nigrostriatal lesion created 2 weeks earlier by stereotactically injecting 8 μg of 6-OHDA into the right median forebrain bundle (MFB; see Soler et al., 2012 for details). The bottom panel shows representative examples of the corresponding cystometric parameter estimates obtained 14 days after sham-injection or injection of AFS cells or BM-MSC, compared with urodynamic responses observed on a healthy control animal; all data are expressed as the mean ± S.E.M. parameters in sham-treated, AFS, BM-MSC, and healthy control groups during follow up (H1, H2). Red bars represent improvement in AFS-injected versus sham-treated rats. Green bars represent improvement in BM-MSC-injected versus sham-treated rats. Of note, the immunofluorescence was no longer detectable 14 days after AFS injection, while the observed recovery was gone by 28 days post-AFS injection. These data highlight two important points. First, and not surprisingly, human stem cell survival in vivo is short lived (<28 days). Second, nonetheless, they can impart significant pharmacological effects and corresponding functional improvement. That is, human AFS cells can temporarily ameliorate bladder dysfunction in a rodent model of Parkinson’s disease. Panels were reproduced from Soler R, Fullhase C, Hanson A, Campeau L, Santos C, and Andersson KE (2012) J Urol; 2012 Apr;187(4):1491–1497.
