Abstract
Background
Dental visits represent an opportunity to identify and assist patients with substance use, but little is known about how dentists are addressing tobacco, alcohol and illicit drugs. We surveyed dentists to learn about the role their practices might play in providing substance use screening and interventions.
Methods
A 41-item, web-based survey was distributed to all 210 dentists active in the PEARL dental practice-based research network. The questionnaire assessed clinic policies and current practices, attitudes, and perceived barriers to providing services for tobacco, alcohol, and illicit drug use.
Results
143 dentists completed the survey (68% response rate). While screening was common, fewer were providing follow-up counseling or referrals for substance use. Insufficient knowledge/training was the most frequently cited barrier to intervention. Many dentists said they would offer assistance for tobacco (67%) or alcohol or illicit drugs (52%) if reimbursed; an affirmative response was more likely among those who saw publicly insured patients.
Conclusions
Dentists recognize the importance of screening for substance use, but lack clinical training and systems that could facilitate intervention.
Practice Implications
If barriers were reduced through changes in reimbursement, education, and systems-level support, our findings indicate that dentists may be willing to address substance use, including use of alcohol and illicit drugs as well as tobacco.
Keywords: Substance use, tobacco cessation, dental tobacco interventions, dental practice, dental clinics, PEARL Network
Introduction
Misuse of tobacco, alcohol and other drugs leads to more death and disability than any other preventable health condition, yet a remarkably small percentage of users are offered treatment within healthcare settings.1,2,3,4 Patient visits to health care providers are increasingly viewed as opportunities to provide screening and interventions for substance use disorders. There is strong evidence that even brief interventions in primary medical care settings can produce significant and sustained reductions in tobacco use and alcohol consumption.5,6,7 The United States Preventive Services Task Force (USPSTF) recommends that health care providers screen and intervene for tobacco use for all adults, and the 2008 Public Health Service (PHS) Guideline, Treating Tobacco Use and Dependence, advises multiple interventions to occur at each point of contact with the health care system.8,9 The USPSTF also recommends that primary care providers screen and counsel for risky alcohol use and misuse,10 and a growing body of research supports this approach for users of illicit drugs as well.11
Dentists represent a largely untapped resource for identifying harmful substance use and increasing access to treatment. Dental clinics see a broad proportion of the population, and have regular contact with individuals who do not otherwise see medical providers. In 2008, an estimated 42% of adults in the U.S. visited a dentist,12 23% of whom saw no other healthcare provider during the year.13
In addition to public health benefits, substance use interventions have high clinical relevance for dentists, due to the substantial effects of tobacco, alcohol, and other drugs on oral health. Tobacco and alcohol use are the primary risk factors for oral and pharyngeal cancer in the US.14 Tobacco is also associated with early tooth loss, periodontal disease, gingivitis and caries.15,16,17,18 Direct consequences of alcohol and illicit drugs on oral health include early and severe periodontitis and dental caries.19,20,21,22
Screening and interventions in dental settings can be effective in helping patients to stop using tobacco, and are highly cost effective.23,24,25,26 As an endorsement of the role of dentistry in tobacco cessation efforts, the newly released Healthy People 2020 includes as a key objective improving the rates of screening and cessation counseling in dental care settings.27 Surveys of dentists conducted over the past fifteen years indicate that screening for tobacco use has increased, from about one-third of dentists reporting that they conducted routine tobacco screening in early surveys, to a majority (59%) doing so in a more recent survey of Florida dentists.28,29,30 Yet while tobacco screening is becoming more routine in dental clinics, rates of tobacco cessation assistance remain relatively low. Dentists cite multiple barriers to providing tobacco cessation assistance, including limited time and knowledge, lack of reimbursement, and concern that patients will not be receptive to addressing tobacco use in the dental setting.28,31,32,33 Gaining a current and nuanced understanding of these barriers is important for developing interventions that can be widely implemented and sustained as part of regular clinical practice.
Much less is known about dentist practices surrounding their patients’ use of alcohol and illicit drug use. No prior studies have assessed what types of screening practices dentists may have in place to identify substance use disorders, or whether they are offering services (counseling, referral to drug treatment) to high-risk patients. This issue is particularly salient in light of rising rates of prescription opioid abuse,34 and the role of dentists and oral surgeons as frequent prescribers of these medications for treatment of post-procedure pain.35,36
To learn more about dentist practice patterns, experiences, and attitudes regarding substance use screening and interventions, we undertook a survey of primary care dentists. Our goal was to assess the current potential for the dental practice to play a greater role in identifying and providing assistance to patients with substance use disorders, and to determine potential barriers to integration of these services in the dental setting. This study represents the first attempt to characterize US dental practitioners’ attitudes toward screening and interventions for alcohol and illicit drugs alongside tobacco, and contributes to the growing body of knowledge about preventive dental interventions.13,37,38,39,40,41
Methods
Study Design and Population
Dentists surveyed were members of the National Institute on Dental and Craniofacial Research (NIDCR)-sponsored Practitioners Engaged in Applied Research and Learning (PEARL) practice-based research network (PBRN). PEARL Network members are practicing dentists who have expressed interest in conducting research in their own clinical practices. PEARL recruits dentists from a variety of settings including private and group practices, corporate models of dentistry and community health centers. PEARL dentists were chosen for the current study because of interest within the PBRN in studying dental tobacco cessation interventions. All 210 dentists active in the PEARL Network as of May 2010 were eligible to participate. Responses were collected over an 8-week period during the summer of 2010.
All PEARL Network dentists received an email notifying them of the study and directing them to a secure website to participate in the web-based survey. Follow-up phone calls and up to six e-mails were made to dentists who did not complete the survey following the initial notification. Participants were asked to read a statement of consent prior to beginning, and a click-to-consent process was used. Dentists received compensation of $100 for completing the survey. The study was approved by the New York University School of Medicine Institutional Review Board.
Variables and Measures
Survey
A 41-item survey was the primary means of data collection. The survey was developed by the authors, with additional input from the PEARL data coordinating center (The EMMES Corporation), and PEARL staff. The survey questionnaire was pilot tested with members of the PEARL executive committee, which includes dental Practitioner-Investigators. A telephone focus group of pilot participants was conducted by the authors (JM and FC) to discuss the survey, and changes to the preamble and phrasing of survey questions were made based on their review.
The survey assessed individual characteristics and attitudes of respondents as well as aspects of their clinical practice sites, including policies and procedures on addressing substance use. All information was based on the individual respondent’s self-report. For practice characteristics, dentists were asked to base their responses on the clinic where they work the majority of the time. The respondent and practice characteristics collected on the survey were: practice type and setting, staffing and insurance accepted, provider demographics, provider specialty, and year of graduation from dental school.
Survey items asked for responses specific to tobacco, alcohol or illicit drug use. Providers were asked about attitudes and practices toward screening, counseling, and referral for patients who use these substances. The survey included specific questions about evidence-based tobacco cessation practices, and about potential barriers to implementation of screening and interventions for tobacco, alcohol and illicit drug use in dental clinics. Illicit drugs were defined in the survey as ‘street drugs, narcotics, illegal drugs, and nonmedical use of prescription drugs.’ A survey item that asked respondents to rate the importance of screening for tobacco, alcohol use, illicit drug use, HIV and hypertension used a broad definition of screening to include ‘having patients fill out a medical/dental history or survey form, asking them in person, or a diagnostic test.’ Survey items about the respondent’s clinical practice defined screening more specifically as 1) ‘does the patient dental/medical history form include questions about [tobacco/alcohol/illicit drugs] in one item, and 2) do providers ‘routinely ask patients verbally about [tobacco/alcohol/illicit drugs]’ in a separate item. Similar items about providing assistance asked if providers ‘routinely counsel and/or provide referrals.’ Six barriers were explicitly queried: lack of time, belief that dental practices are not effective in helping patients quit, lack of knowledge/training in providing interventions, belief that the dental office is not an appropriate setting, staff resistance, and having nowhere to refer patients with substance use problems.
Respondent Profile
Additional information on respondent and practice characteristics was gathered from the PEARL Network’s membership profiles of survey respondents, which provided the following variables: dental degree, ownership status, and geographic region.
Statistical Analysis
Descriptive analyses consisted of frequencies and distributions of clinic and individual characteristics. Univariate logistic regression was used to independently examine associations of respondent characteristics, practice characteristics, and perceived barriers with readiness to offer either tobacco assistance, alcohol, or illicit drug assistance. Readiness to offer assistance was based on responses to a survey item asking: ‘If third-party reimbursement were available, I would offer counseling and assistance to patients who use [tobacco/alcohol/illicit drugs].’ Answer categories were ‘yes’, ‘no’, or ‘neutral/don’t know’. Responses were dichotomized, with ‘yes’ considered positive and any other response negative. ‘Neutral/don’t know’ was considered a negative response because it implies that the individual is not currently ready to offer substance use counseling and assistance.
Responses to items assessing readiness to offer alcohol or illicit drug assistance indicated that our sample of dentists regarded intervention for these two substance classes similarly. The univariate analyses indicated that the same characteristics associated with readiness to offer assistance to patients who use alcohol were also associated with readiness to offer assistance to patients who use illicit drugs. We observed a very high correlation (phi=0.89) between readiness to offer assistance for alcohol and for illicit drugs. Given the high degree of overlap in responses regarding these two substance classes, we inferred that respondents were not making a distinction between alcohol and illicit drugs. Based on this observation, and a recognition that alcohol and drug problems demand similar clinical interventions,42,43 for analytic purposes alcohol and illicit drugs were later combined into a single variable; alcohol and other drugs (AOD). Readiness to offer assistance variable for AOD was ranked as ‘yes’ if the response was positive to readiness to address either alcohol or other drugs, and ‘no’ for all other responses.
For items addressing potential barriers, responses were assessed using a 5-point scale, ranging from ‘Strongly Agree’ (5) to ‘Strongly Disagree’ (1). In the descriptive analyses, these responses were dichotomized into ‘Agree’ versus ‘Disagree,’ with neutral responses included in the ‘Disagree’ category. We then examined the intercorrelation between the six barriers, for each substance class (tobacco, alcohol, illcit drugs), using Cronbach’s alpha. The results suggested that with the exception of the item addressing referral sources, the barrier items could be combined into a single score. When the lack of referral sources barrier was excluded from the barrier score, Cronbach’s Alpha was .71 for the tobacco barriers, .72 for the alcohol barriers, and .72 for the illicit drug barriers. In a second step, barrier scores were calculated to indicate the strength of perceived barriers to addressing tobacco or alcohol and other drug use, across the queried domains pertaining to knowledge and training, time, staff resistance, effectiveness and setting. The scores for individual substances (tobacco, alcohol, illicit drugs ) are a sum of ranked answers (possible range 5–25), while the AOD barrier score variable sums across responses to alcohol barriers and responses to illicit drug barriers, and then takes the midpoint (possible range 5–25). A higher barrier score indicates a stronger perception of barriers to addressing these issues. The association between perceived lack of referral sources and readiness to offer tobacco, alcohol, or illicit drug assistance was examined independently from the combined barrier scores.
Two multivariate models were developed to examine predictors of readiness to offer assistance to users of tobacco or substances other than tobacco (i.e. alcohol or illicit drugs). In Model A, the dependent variable was readiness to provide tobacco assistance, and in Model B the dependent variable was readiness to provide assistance for AOD. A stepwise model-building approach was used to develop each multivariate model with entry P value of 0.10 and an exit P value of 0.05, thus statistical significance is assessed at the 0.05 level. PASW Statistics version 18 (SPSS) was used for all final analyses.
Results
Of the 210 dentists eligible, 143 participated in the survey (response rate 68%). Characteristics of dentist respondents and their primary dental clinics are shown in Table 1. We compared the member profiles of survey respondents to the PEARL Network as a whole, and found no substantial differences between them in age, sex, race, or practice setting. Most participants (88%) were in general practice settings, including four public health and two dental medicine clinics. The majority of practices had one full-time dentist, and were located in the northeastern US. Payment was primarily private insurance or no insurance/self-pay; a minority of clinics had at least one patient covered by Medicare (21%) or Medicaid (30%).
Table 1.
Dentists Respondent and Dental Practice Characteristics (N=143)
| Dentist Responder Characteristics | |
|---|---|
| Characteristic | N (%) |
| Age | |
| Median | 53 |
| Range | 30–70 |
| IQR | 11 |
| Gender | |
| Male | 100 (70%) |
| Female | 43 (30%) |
| Race/Ethnicity1 | |
| White | 99 (69%) |
| Asian | 15 (10%) |
| Black | 12 (8%) |
| Hispanic | 12 (8%) |
| Other | 5 (3%) |
| Degree | |
| DDS | 80 (56%) |
| DMD | 63 (44%) |
| Years Since Graduation | |
| Median | 26 |
| Range | 2–43 |
| IQR | 11 |
| Provider Type | |
| Generalist | 130 (91%) |
| Specialist | 13 (9%) |
| Ownership Status | |
| Owner | 92 (64%) |
| Co-owner/partner | 28 (20%) |
| Neither | 23 (16%) |
| Dental Practice Characteristics | |
|---|---|
| Characteristic | N (%) |
| Practice Type | |
| General | 126 (88%) |
| Pediatric | 8 (6%) |
| Periodontics | 5 (3%) |
| Other | 4 (3%) |
| Practice Setting | |
| Suburban | 86 (60%) |
| Urban | 43 (30%) |
| Rural | 12 (8%) |
| Other | 2 (1%) |
| Practice Region | |
| Northeast | 100 (70%) |
| South | 25 (17%) |
| Midwest | 12 (8%) |
| West | 6 (4%) |
| Active Patients | |
| <1000 | 31 (22%) |
| 1000–1999 | 62 (43%) |
| ≥2000 | 50 (35%) |
| Number of Full-time Dentists | |
| No full-time dentist | 3(2%) |
| 1 dentist | 82 (57%) |
| 2–3 dentists | 35 (24%) |
| 4+ dentists | 14 (10%) |
| Missing | 9 (6%) |
| Number of Full-time Hygienists | |
| No hygienists | 38 (27%) |
| 1 hygienist | 43 (30%) |
| 2–3 hygienists | 28 (20%) |
| >3 hygienists | 13 (9%) |
| Missing | 21 (15%) |
| Practices utilizing this insurance |
Percentage of patients covered by this insurance2 | |||
|---|---|---|---|---|
| Insurance Type | N (% of practices) | Median | Range | IQR |
| Private | 141 (99%) | 60 | 2–100 | 35 |
| No Insurance/self pay | 139 (97%) | 25 | 2–90 | 28 |
| Medicaid | 43 (30%) | 20 | 1–95 | 25 |
| Medicare | 30 (21%) | 13 | 11–75 | 21 |
| Other | 17 (12%) | 15 | 1–100 | 18 |
Dentists reporting Hispanic ethnicity classified as Hispanic, regardless of race.
Percentage reported for practices having at least one patient with this insurance type.
Screening and assistance for users of tobacco, alcohol and other drugs
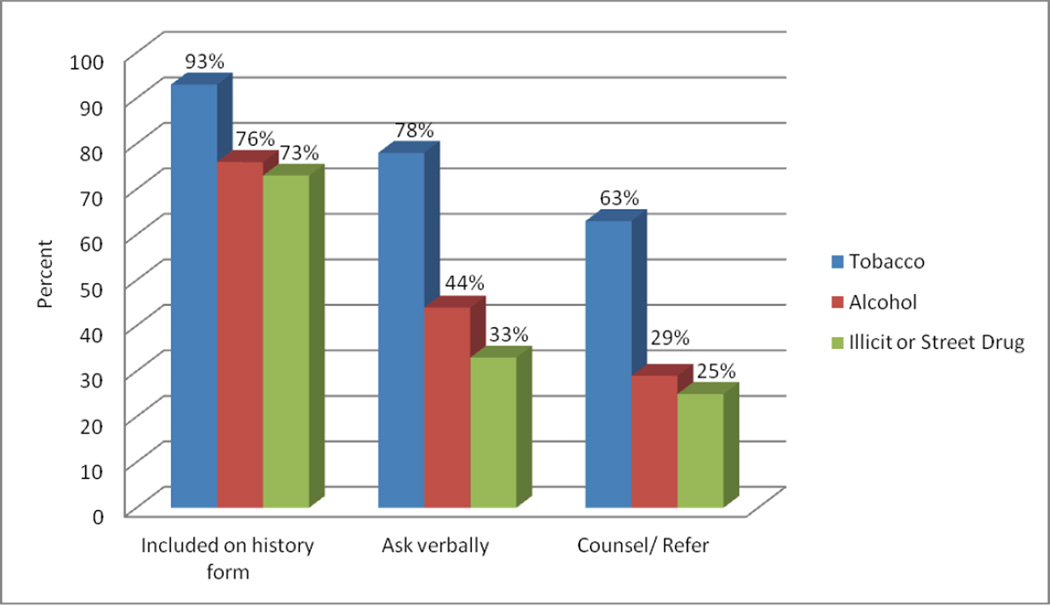
The majority of participants responded that it was ‘somewhat important’ or ‘very important’ for dental practices to screen patients for tobacco (99%), alcohol (92%) and illicit drug use (93%). Participants also responded that they considered it ‘somewhat important’ or ‘very important’ to screen for hypertension (99%) and HIV (91%). Many dental practices were conducting screening for substance use (Figure 1). Screening was provided primarily through the written dental/medical history form, but verbal (in-person) screening was frequently conducted as well, more often for tobacco than for alcohol or other drugs. Most respondents (63%) reported that providers in their practice ‘routinely’ counseled and/or provided referrals to tobacco users, but these services were less frequently reported as being offered to alcohol and illicit drug users (29% and 25%, respectively).
Figure 1.
Percent of dentists reporting that their dental clinic provides screening or assistance for tobacco, alcohol or other drug use (N=143)
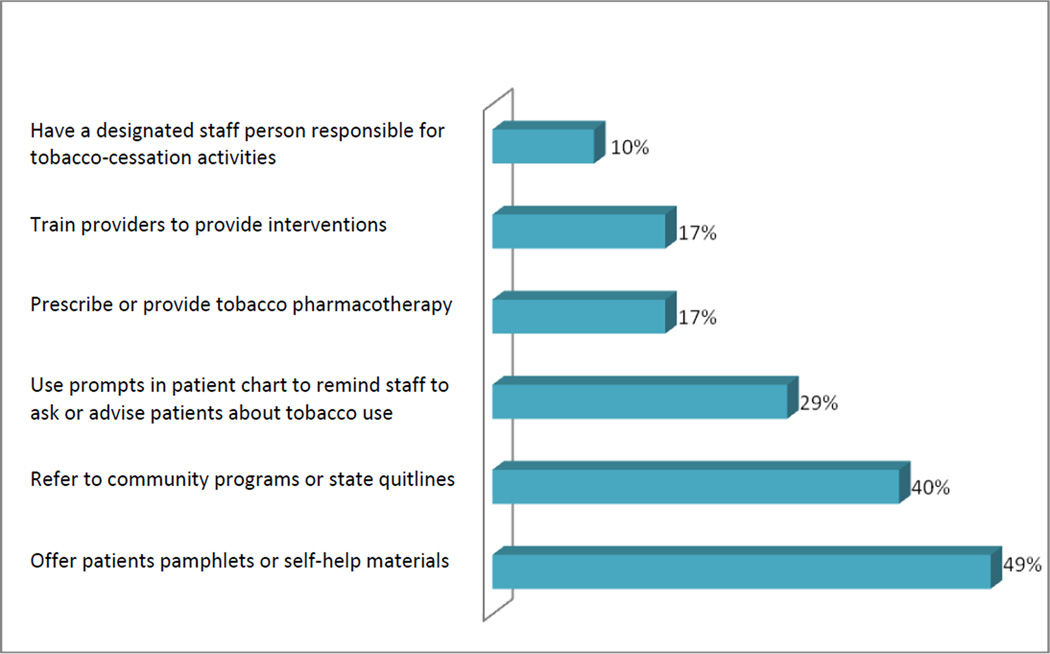
Evidence-based practices for tobacco cessation
The survey asked a number of specific questions about evidence-based practices for tobacco cessation assistance (Figure 2). The most frequently reported activities were providing pamphlets and self-help materials, and referring patients to community programs or state ‘quitlines.’ Tobacco pharmacotherapy was provided at 17% of practices. Dentists and hygienists were most frequently named as the staff persons primarily responsible for providing counseling to tobacco users.
Figure 2.
Percent of dental practices engaged in specific evidence-based tobacco cessation interventions (N=143)
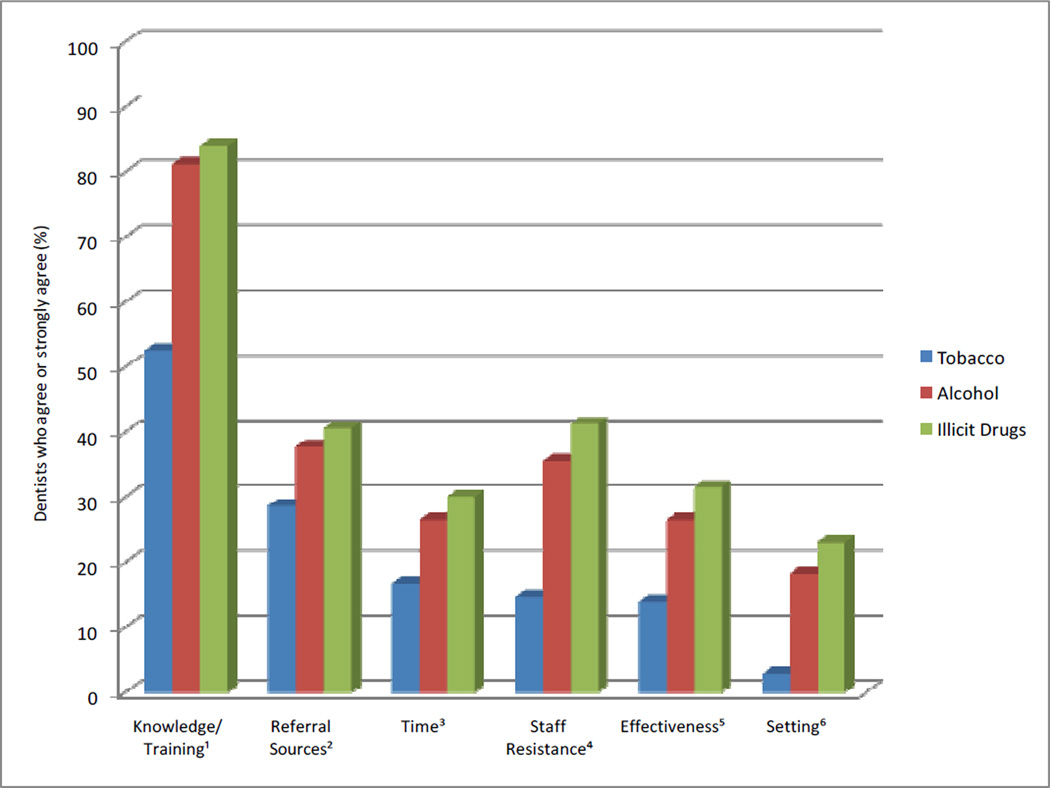
Barriers to addressing tobacco, alcohol and substance use
Dentists were asked to identify their level of agreement with six specific potential barriers to addressing tobacco, alcohol and illicit drug use among their patients (Figure 3). Barriers to addressing tobacco use were ranked lower than those for alcohol and other drugs. Lack of knowledge or training was the most frequently cited barrier to addressing tobacco (53%), alcohol (81%), and illicit drug use (84%). The second most commonly cited barrier for tobacco and alcohol was lack of referral resources; for illicit drugs it was a belief that clinic staff would be resistant to providing the intervention. There was a statistically significant (P<0.001) difference between tobacco and alcohol or illicit drug responses as to whether the dental setting was appropriate for intervention. Three percent of respondents felt it was an inappropriate setting to address tobacco, while for alcohol and illicit drugs it was 18% and 23% respectively.
Figure 3.
Perceived barriers to addressing tobacco, alcohol, and illicit drug use in dental practices (N=143)
1 My staff and I don’t have enough knowledge/training in providing interventions for [tobacco/alcohol/illicit drugs].
2 I have nowhere to refer patients who have problems with [tobacco/alcohol/illicit drugs].
3 My staff and I do not have time to help patients quit using [tobacco/alcohol/illicit drugs].
4 My staff would be resistant to addressing [tobacco/alcohol/illicit drugs].
5 I do not think dental practices can be effective at helping patients quit using [tobacco/alcohol/illicit drugs].
6 I don’t think dental practices are an appropriate setting to address [tobacco/alcohol/illicit drugs].
Readiness to offer tobacco or alcohol and other drug assistance
Dentists were asked whether they would offer counseling and assistance to patients who use tobacco, alcohol and illicit drugs, if third-party reimbursement were available for these services. A majority of dentists indicated readiness to provide assistance to users of tobacco (67%) and of alcohol/illicit drugs (52%). Sixty-seven participants (47%) indicated that they would provide assistance to users of all three substances. Among those who were not ready to offer assistance, the majority of responses were ‘neutral/don’t know’ rather than ‘no’.
Table 2 presents the univariate associations between respondent and practice characteristics associated with readiness to offer assistance for either tobacco or alcohol and other drugs that had P<0.10, and would thus be considered in building the final multivariate models. Among practice characteristics, having patients with Medicaid or Medicare coverage (at least 5% of patients in the practice) was positively associated with readiness to provide assistance for tobacco. Eighty-two percent of dentists from Medicaid practices responded that they would offer tobacco assistance, compared to 62% of those from non-Medicaid practices. The difference between these two groups in readiness to offer tobacco assistance was statistically significant (P=0.02). Similarly, dentists from Medicaid practices were significantly more likely to respond that they were ready to offer assistance for alcohol or other drugs (P<0.05). A higher percentage of non-white respondents indicated they were ready to provide assistance for AOD users. However, race was significantly associated with having at least 5% Medicaid patients in the practice (39% of non-white participants versus 22% of white participants, P=.04).
Table 2.
Dental practice and dentist characteristics associated with readiness to offer either tobacco or alcohol and other drug assistance
| Characteristic | Number of respondents |
Would offer assistance to tobacco users |
Would not offer assistance to tobacco users |
P valuea tobacco) |
Would offer assistance to alcohol/other drug (AOD) users |
Would not offer assistance to alcohol/other drug (AOD) users |
P valuea (AOD) |
|---|---|---|---|---|---|---|---|
| N | N (% of row) | ||||||
| Total population | 143 | 96 (67%) | 47 (33%) | -- | 75 (52%) | 68 (48%) | -- |
| Dentist Responder Characteristics | |||||||
| Age (years) | 143 | 96 (67%) | 47 (33%) | 0.505 | 75 (52%) | 68 (48%) | 0.400 |
| Gender | 0.736 | 0.840 | |||||
| Male | 100 | 68 (68%) | 32 (32%) | 53 (53%) | 47 (47%) | ||
| Female | 43 | 28 (65%) | 15 (35%) | 22 (51%) | 21 (49%) | ||
| Race/Ethnicity | 0.184 | 0.033 | |||||
| White | 99 | 63 (64%) | 36 (36%) | 46 (46%) | 53 (54%) | ||
| Non-White | 44 | 33 (75%) | 11 (25%) | 29 (66%) | 15 (34%) | ||
| Degree | 0.745 | 0.707 | |||||
| DDS | 80 | 56 (70%) | 24 (30%) | 45 (56%) | 35 (44%) | ||
| DMD | 63 | 40 (63%) | 23 (37%) | 30 (48%) | 33 (52%) | ||
| Provider Type | 4 | 0.291 | 0.634 | ||||
| Generalist | 130 | 89 (68%) | 1 (32%) | 69 (53%) | 61 (47%) | ||
| Specialist | 13 | 7 (54%) | 6 (46%) | 6 (46%) | 7 (54%) | ||
| Ownership Status | 0.513 | 0.139 | |||||
| Solo owner | 92 | 60 (65%) | 32 (35%) | 44 (48%) | 48 (52%) | ||
| Co- or non-owner | 51 | 36 (71%) | 15 (29%) | 31 (61%) | 20 (39%) | ||
| Barrier Score: Tobaccob | 143 | 96 (67%) | 47 (33%) | 0.005 | 75 (52%) | 68 (48%) | 0.039 |
| Mean | 12.1 | 11.5 | 13.3 | 11.5 | 12.8 | ||
| Standard Deviation | 3.6 | 2.9 | 4.5 | 3.0 | 4.0 | ||
| Range | 5–24 | 6–18 | 5–24 | 6–18 | 5–24 | ||
| Barrier Score: AODb | 143 | 96 (67%) | 47 (33%) | 0.056 | 75 (52%) | 68 (48%) | <.001 |
| Mean | 15.4 | 14.9 | 16.3 | 13.7 | 17.2 | ||
| Standard Deviation | 4.0 | 4.2 | 3.4 | 3.5 | 3.8 | ||
| Range | 6–25 | 6–25 | 10–25 | 6–22 | 10–25 | ||
| Dental Practice Characteristics | |||||||
| Practice Type | 0.190 | 0.636 | |||||
| General | 126 | 87 (69%) | 39 (31%) | 67 (53%) | 59 (47%) | ||
| Other | 17 | 9 (53%) | 8 (47%) | 8 (47%) | 9 (53%) | ||
| Practice Setting | 0.055 | 0.825 | |||||
| Urban | 43 | 35 (81%) | 8 (19%) | 24 (56%) | 19 (44%) | ||
| Suburban | 86 | 52 (60%) | 34 (40%) | 43 (50%) | 43 (50%) | ||
| Rural/Other | 14 | 9 (64%) | 5 (36%) | 8 (57%) | 6 (43%) | ||
| Practice Region | 0.469 | 0.870 | |||||
| Northeast | 100 | 69 (69%) | 31 (31%) | 52 (52%) | 48 (48%) | ||
| Other | 43 | 27 (63%) | 16 (37%) | 23 (53%) | 20 (47%) | ||
| Active Patients | 0.953 | 0.815 | |||||
| <1000 | 31 | 20 (65%) | 11 (35%) | 16 (52%) | 15 (48%) | ||
| 1000–1999 | 62 | 43 (69%) | 19 (31%) | 32 (52%) | 30 (48%) | ||
| ≥2000 | 50 | 33 (66%) | 17 (34%) | 27 (54%) | 23 (46%) | ||
| Number of full-time dentists | 0.863 | 0.830 | |||||
| 0–1 dentist | 85 | 56 (66%) | 29 (34%) | 45 (53%) | 40 (47%) | ||
| >1 dentist | 49 | 33 (67%) | 16 (33%) | 25 (51%) | 24 (49%) | ||
| Number of full-time hygienists | 0.963 | 0.567 | |||||
| 0–1 Hygienist | 81 | 53 (65%) | 28 (35%) | 41 (51%) | 40 (49%) | ||
| >1 hygienist | 41 | 27 (66%) | 14 (34%) | 23 (56%) | 18 (44%) | ||
| Patient Coverage: Medicaid | 0.023 | 0.006 | |||||
| <5% Medicaid | 104 | 64 (62%) | 40 (38%) | 47 (45%) | 57 (55%) | ||
| ≥5% Medicaid | 39 | 32 (82%) | 7 (18%) | 28 (72%) | 11 (28%) | ||
| Patient Coverage: Medicare | 0.022 | 0.091 | |||||
| <5% Medicare | 118 | 74 (63%) | 44 (37%) | 58 (49%) | 60 (51%) | ||
| ≥5% Medicare | 25 | 22 (88%) | 3 (12%) | 17 (68%) | 8 (32%) | ||
P values are based on univariate logistic regression using readiness to provide counseling and assistance for tobacco users or users of alcohol or other drugs as the dependent variable.
Barrier score indicates the sum of individual responses to barriers faced in addressing tobacco or alcohol/other drug use. Respondents were asked to rank their response on a 5-point Likert scale (1=strongly disagree, 5=strongly agree).
We found that the mean barrier scores for tobacco were lower among individuals who responded that they were ready to offer assistance to tobacco users (mean score of 11.5 versus 13.3, out of a possible maximum score of 25), and that the tobacco barrier score was significantly associated with readiness to offer assistance to both tobacco users (P<.005) and AOD users (P=.039). The mean AOD barrier scores were lower for those who responded that they were ready to offer assistance to AOD users (mean score of 13.7 versus 17.2 out of a possible score of 25). The AOD barrier score was significantly associated with readiness to provide assistance for AOD (P<.001) but not for tobacco (P=.056). The potential barrier of lack of referral sources was not significantly associated with readiness to offer tobacco or AOD services. There was no significant association between race and barrier score for tobacco or AOD.
Two multivariate models presented in Table 3 examine respondent and practice characteristics that may predict readiness to offer substance use counseling or referrals. Model A specifically examines predictors of readiness to offer tobacco cessation assistance, and Model B readiness to offer alcohol or illicit drug (AOD) assistance. In Model A, the adjusted odds of readiness to offer tobacco cessation assistance were significantly decreased for dentists who perceived high barriers to offering tobacco cessation services, controlling for having at least 5% of patients covered by Medicaid. Individuals with higher tobacco barrier scores were only 89% as likely as those with lower barrier scores to say that they were ready to offer tobacco cessation assistance (P=.039). Readiness to offer tobacco cessation services was not significantly affected by perceived barriers to offering AOD services in the multivariate model. Similarly, in Model B, high perceived barriers to providing AOD services significantly decreased the adjusted odds of readiness to offer assistance for these substances (OR=.76, P<.001). Having patients with Medicaid significantly increased the adjusted odds of being ready to offer assistance to AOD users (OR=3.06, P=.020), controlling for perceived barriers to providing either tobacco or AOD services.
Table 3.
Multivariate models of individual- and practice-level characteristics and adjusted odds of readiness to offer Model A) tobacco or Model B) alcohol or illicit drug assistance
| Model A | Model B | |||
|---|---|---|---|---|
| Would offer tobacco cessation assistance |
Would offer alcohol or illicit drug use cessation assistance |
|||
| Variable | OR (95% CI) | P value | OR (95% CI) | P value |
| ≥ 5% of patients covered by Medicaida | NA | NA | 3.06 (1.19–7.87) | 0.020 |
| Tobacco barriers score | 0.89 (0.79–0.99) | 0.039 | NA | NA |
| Alcohol and Illicit drug barriers score | NA | NA | 0.87 (0.82–0.93) | <0.001 |
NA: Variable did not remain in the multivariate model after variable selection.
Reference category is <5% of patients covered by Medicaid
Model A: Dependent variable is readiness to offer tobacco assistance (Yes vs. No/Neutral response to Q28) Hosmer and Lemeshow Test P=0.40
Model B: Dependent variable is readiness to offer alcohol or other drug assistance (Yes vs. No/Neutral response to Q28) Hosmer and Lemeshow Test P=0.42
Discussion
Our survey indicates that dentists in the PEARL practice-based research network highly approve of screening for substance use, and most were conducting screening within their clinics. As PBRN members, these practitioners have already expressed a strong interest in research, and may be more favorably disposed to adopting newer practices such as screening and interventions for substance use. Yet even among this group, rates of follow-up counseling and referrals for patients with positive screening results were much lower than rates of screening, particularly with respect to alcohol and other drugs. Our findings suggest that more support is needed for implementation of clinical interventions that go beyond screening, to offer assistance to patients who are identified as having harmful use of tobacco and other substances.
Screening and cessation assistance was more often offered for tobacco use than for alcohol or illicit drugs, and dentists saw fewer barriers to providing tobacco-related services. These providers had higher rates of tobacco screening and interventions than has been shown in prior surveys of dentists. 28,30, 32 While some of this discrepancy may be attributable to characteristics of PBRN dentists, it is also likely to reflect regional variation as well as temporally changing patterns of dental practice. Our results are comparable to a 2003–2004 national survey of health care providers which found that 90% of dentists ‘ever ask if a patient smokes’ and 71% of dentists advised smokers to quit,4 and to a 2009 survey of Florida dentists, in which 59% reported routine tobacco screening and 46% offered advice.29 However, although a majority of respondents in our study said that their practices offer some counseling and referrals to tobacco users, our analysis showed that the adoption of effective evidence-based approaches to tobacco cessation assistance, including provision of pharmacotherapy, was low. This is consistent with findings from prior studies of tobacco cessation efforts in dentistry.30,31,32,44
Dentists indicated that they perceived numerous barriers to integrating substance use services into dental practice, and these barriers as a whole were associated with readiness to offer assistance to substance users. In the multivariate analyses, perceived greater barriers to providing tobacco services decreased the odds of being ready to provide tobacco (but not AOD) cessation assistance, and greater barriers to providing AOD services decreased the odds of being ready to provide either tobacco or AOD assistance. Of the specific potential barriers queried in our survey, the most frequently perceived single barrier to addressing all substances was lack of knowledge and training. This was also identified as one of the most common barriers to addressing tobacco cessation in the survey of Florida dentists.27 Other barriers identified in our dentist population have also been found in prior studies of dentists on tobacco activities, including lack of referral resources, time pressures, and staff resistance.28,44 Our study is unique in also examining barriers to providing assistance to users of alcohol and illicit drugs. Perhaps not surprisingly given the relative lack of focus on alcohol and drug interventions compared to tobacco cessation in dental practices, dentists saw fewer barriers to addressing tobacco than they did for alcohol and other drugs.
Notably, we found that dentists from practices with Medicaid patients were more willing to offer alcohol and drug services, if reimbursement was provided. It is possible that clinics accepting patients with public insurance have a more explicit public health mission, or a service delivery system that is more accommodating of behavioral interventions. Our sample did not include enough of these providers to identify specific individual or practice characteristics that could explain their greater readiness to provide substance use interventions.
Limitations
Our study does have important limitations. The survey sample was drawn exclusively from practitioners in the PEARL Network, and cannot be assumed to represent a more general population of dentists. Dentists participating in a PBRN may be expected to have more favorable views toward incorporating new approaches to care, such as screening and interventions for tobacco and other substance use, into their clinical practice. This could bias our sample toward having higher rates of support for addressing tobacco and other substance use than might be found in a general sample of dentists. A recent study from another dental PBRN showed that overall their members have similar characteristics to those of US dentists at large, though activities and attitudes directed at addressing substance use was not part of that analysis.45 Also related to the restriction of the survey to members of the PEARL Network, the sample is relatively homogeneous in terms of both respondent and practice characteristics. These results largely represent the practices and attitudes of experienced general practice dentists in fairly small suburban and urban dental clinics. While this does represent the predominant practice model in dentistry,46 a greater diversity of clinic types, including larger or public clinics, may have provided more insight into practice characteristics associated with willingness to address substance use. Having more geographic variation and representation of rural practitioners would similarly have helped provide a more comprehensive picture of dental activities to address substance use. Though our response rate compares favorably to similar surveys,4,29,30,47 it is possible that dentists who elected to participate differ in their attitudes and practice patterns, and that they may be more supportive of providing the types of substance use services that were the focus of our survey.
Some of the terms used in our survey lacked precision. In particular, the survey asked whether providers in the practice ‘routinely’ engage in screening (defined as asking patients verbally) or providing assistance (defined as counseling and/or referrals), but did not explicitly define the frequency implied by ‘routinely’ or specific approaches (i.e. screening questionnaires, particulars of the counseling approach, etc.) to conducting these activities. Reliance on dentist self-report may have inflated estimates of substance use-related practices, due to social desirability bias. We also do not know how accurately respondents were able to characterize the activities of their dental clinic, including the practices of other dentists and other clinic staff. This information bias was countered, however, by the fact that most dentists worked at small single-provider clinics. Finally, our survey specifically asked about readiness to provide substance use assistance if reimbursement were available for these clinical services. We did not explore how responses would differ at varying levels of reimbursement, though this could be a relevant area for future research.
Conclusions
Dentists in the PEARL Network recognize the importance of screening for substance use, but they do not consistently follow up screening results with effective interventions, and perceive significant barriers to doing so. The most frequently cited barrier was lack of knowledge and training about substance use, and in this area educational interventions could be expected to have a favorable impact. But dentists also endorsed systems-level barriers that may require more complex and practice-specific solutions. Perhaps the most important barrier may be the lack of reimbursement for substance use screening and interventions for tobacco or alcohol and other drug use in dental practice.
If barriers were reduced through changes in reimbursement, education, and systems-level support, our findings indicate that dentists may be willing to address substance use among their patients. In medicine more generally, with the shift toward patient-centered medical homes there is an evolving focus on addressing behavioral health conditions, including substance use, as part of primary care. Given this changing focus, and the potential for dentistry to have a broad impact on public health, the involvement of dentists as partners in identifying and addressing substance use may deserve further exploration.
Acknowledgements
Damon Collie and Don Vena, EMMES Corporation
George E. Bigelow, CTN Publications Committee
We would also like to thank Nora Volkow, M.D., Director of the National Institute on Drug Abuse (NIDA) at the National Institutes of Health, and colleagues at the Clinical Trials Network for support and encouragement in exploring acceptability and sustainability of innovation in approaches to tobacco cessation.
Funding disclosure:
NIH/NIDA Clinical Trials Network (5U10DA013046 and U10 DA13035) NIH/NIDCR (U01 DE016755)
Dr. McNeely received support from NIH/NIDA (K23DA030395) and NIH/NYU CTSI (KL2RR029891)
Footnotes
Disclosure: No authors have any financial, economic or professional interests that influence positions presented in this article.
Statement of Contributions:
Jennifer McNeely, Fredrick A. Curro, John Rotrosen and Donna Shelley conceived of the study.
Jennifer McNeely and Matthew Buchholz directed the study.
Jennifer McNeely led the writing and analysis.
Shana Wright and Abigail G. Matthews made major contributions to the writing and analysis.
All authors advised on the analysis and contributed to the writing.
Contributor Information
Jennifer McNeely, Department of Population Health, Department of Medicine, Division of General Internal Medicine, NYU School of Medicine, 227 E. 30th Street, Room 623, New York, NY 10016, (p) 212/ 263-4975 (f) 646/ 501-2706, Jennifer.McNeely@nyumc.org.
Shana Wright, Department of Psychiatry, Department of Population Health, NYU School of Medicine, 423 E. 23rd Street, 12N-147, New York, NY 10010, (p) 212/ 686-7500 x3178 (f) 212/ 951-5848, Shana.Wright@nyumc.org.
Abigail G. Matthews, EMMES Corporation, 401 N. Washington Street, Suite 700, Rockville, MD 20850, (p) 301/ 251-1161 x 2819 (f) 301/ 576-3696, amatthews@emmes.com.
John Rotrosen, Center of Excellence on Addiction, NYU School of Medicine, VA New York Harbor Healthcare System, 423 E. 23rd Street, Room 17014W, New York, NY 10010, (p) 212/ 951-3294 (f) 212/ 951-6891, John.Rotrosen@nyumc.org.
Donna Shelley, Department of Population Health, Department of Medicine, Division of General Internal Medicine, NYU School of Medicine, 227 E. 30th Street, Room 608, New York, NY 10016, (p) 646-501-2526 (f) 646/ 501-2706, Donna.shelley@nyumc.org.
Matthew P. Buchholz, PEARL Practice-Based Research Network, New York University College of Dentistry, 380 Second Avenue, Suite 302, New York, NY 10010, (p) 646/ 429-9925 (f) 212/ 995-4568, mbuchholz@emmes.com.
Frederick A. Curro, Director of Clinical Operations, PEARL Network, Director of Regulatory Affairs, Bluestone Center for Clinical Research, New York University College of Dentistry, 380 Second Avenue, Suite 302, New York, NY 10010, (p) 212/ 998-9555 (f) 212/ 995-4568, fac3@nyu.edu.
References
- 1.Robert Wood Johnson Foundation and Schneider Institute for Health Policy. Substance abuse: The nation’s number one health problem. Princeton, NJ: Robert Wood Johnson Foundation; 2001. [Accessed Feb. 5, 2010]. Available at: “ http://www.rwjf.org/files/publications/other/SubstanceAbuseChartbook.pdf”. [Google Scholar]
- 2.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 3.Results from the 2008 National Survey on Drug Use and Health: National Findings. Rockville, MD: U.S. Department of Health and Human Services. Substance Abuse and Mental Health Services Administration, Office of Applied Studies; 2009. [Accessed Feb. 5, 2010]. NSDUH Series H-36, HHS Publication SMA 09-4434. Available at “ http://oas.samhsa.gov/nsduh/2k8nsduh/2k8Results.cfm#1.1”. [Google Scholar]
- 4.Tong E, Strouse R, Hall J, Kovac M, Schroeder SA. National survey of U.S. health professionals’ smoking prevalence, cessation practices, and beliefs. Nicotine Tob Res. 2010;12(7):724–733. doi: 10.1093/ntr/ntq071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Solberg L, Maciosek M, Edwards N, Khanchandani H, Goodman M. Repeated tobacco-use screening and intervention in clinical practice: health impact and cost effectiveness. Am J Prev Med. 2006;31(1):62–71. doi: 10.1016/j.amepre.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 6.Fiore MC, Jaen CR, Baker TB, et al. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2008. Treating tobacco use and dependence: 2008 update. [Google Scholar]
- 7.Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140:557–568. doi: 10.7326/0003-4819-140-7-200404060-00017. [DOI] [PubMed] [Google Scholar]
- 8.U.S. Preventive Services Task Force. Counseling and Interventions to Prevent tobacco Use and Tobacco-Caused Disease in Adults and Pregnant Women. Rockville, MD: Agency for Healthcare Research and Quality, U.S. Preventive Services Task Force; 2009. [Accessed July 12, 2012]. Available at “ http://www.uspreventiveservicestaskforce.org/uspstf/uspstbac2.htm”. [Google Scholar]
- 9.Tobacco Use and Dependence Guideline Panel. Treating Tobacco Use and Dependence: 2008 Update. Rockville, MD: U.S. Department of Health and Human Services; 2008. [Accessed July 12, 2012]. Available at “ http://www.ncbi.nlm.nih.gov/books/NBK63952”. [Google Scholar]
- 10.U.S. Preventive Services Task Force. Screening and Behavioral Counseling Interventions in Primary Care to Reduce Alcohol Misuse, Topic Page. Rockville, MD: Agency for Healthcare Research and Quality, U.S. Preventive Services Task Force; 2004. [Accessed July 12, 2012]. Available at “ http://www.uspreventiveservicestaskforce.org/uspstf/uspsdrin.htm”. [Google Scholar]
- 11.Madras B, Compton W, Avula D, Stegbauer T, Stein J, Clark HW. Screening, brief interventions, referral to treatment (SBIRT) for illicit drug and alcohol use at multiple healthcare sites: comparison at intake and 6 months later. Drug Alcohol Depend. 2009;99(1–3):280–295. doi: 10.1016/j.drugalcdep.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Medical Expenditure Panel Survey (MEPS) 2008 MEPSnet Query Tool. Rockville, MD: Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services 2008; [Accessed Oct. 12, 2011]. Available at http://www.meps.ahrq.gov/mepsweb/data_stats/MEPSnetHC.jsp. [Google Scholar]
- 13.Strauss SM, Alfano MC, Shelley D, Fulmer T. Identifying unadressed systemic health conditions at dental visits: Patients who visited dental practices but not general health care providers in 2008. Am J Public Health. doi: 10.2105/AJPH.2011.300420. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blot WJ, McLaughlin JK, Winn DM, et al. Smoking and drinking in relation to oral and pharyngeal cancer. Cancer Res. 1988;48:3282–3287. [PubMed] [Google Scholar]
- 15.Silverman S, Rankin K. Oral and pharyngeal cancer control through continuing education. J Cancer Educ. 2010;(3):277–278. doi: 10.1007/s13187-010-0044-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tomar S. Smoking increases the incidence of tooth loss and smoking cessation reduces it. J Evid Based Dent Pract. 2008;8(2):105–107. doi: 10.1016/j.jebdp.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 17.Christen AG. Tobacco cessation, the dental profession, and the role of dental education. J Dent Educ. 2001;65(4):368–374. [PubMed] [Google Scholar]
- 18.Hanioka T, Ojima M, Tanaka K, Aoyama H. Association of total tooth loss with smoking, drinking alcohol and nutrition in elderly Japanese: analysis of national database. Gerodontology. 2007;24(2):87–92. doi: 10.1111/j.1741-2358.2007.00166.x. [DOI] [PubMed] [Google Scholar]
- 19.Khocht A, Janal M, Schleifer S, Keller S. The influence of gingival margin recession on loss of clinical attachment in alcohol-dependent patients without medical disorders. J Periodontol. 2003;74(4):485–493. doi: 10.1902/jop.2003.74.4.485. [DOI] [PubMed] [Google Scholar]
- 20.Hamamoto DT, Rhodus NL. Methamphetamine abuse and dentistry. Oral Dis. 2009;15(1):27–37. doi: 10.1111/j.1601-0825.2008.01459.x. [DOI] [PubMed] [Google Scholar]
- 21.Tezal M, Grossi S, Ho A, Genco R. Alcohol consumption and periodontal disease. The Third National Health and Nutrition Examination Survey. J Clin Periodontol. 2004;31(7):484–488. doi: 10.1111/j.1600-051X.2004.00503.x. [DOI] [PubMed] [Google Scholar]
- 22.Angelillo IF, Grasso GM, Sagliocco G, Villari P, D'Errico MM. Dental health in a group of drug addicts in Italy. Community Dent Oral Epidemiol. 1991;19(1):36–37. doi: 10.1111/j.1600-0528.1991.tb00102.x. [DOI] [PubMed] [Google Scholar]
- 23.Gordon J, Andrews J, Albert D, Crews K, Payne T, Severson H. Tobacco cessation via public dental clinics: results of a randomized trial. Am J Public Health. 2010;100(7):1307–1312. doi: 10.2105/AJPH.2009.181214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Carr AB, Ebbert JO. Interventions for tobacco cessation in the dental setting. Cochrane DB Syst Rev. 2006;(1):CD005084–CD005084. doi: 10.1002/14651858.CD005084.pub2. [DOI] [PubMed] [Google Scholar]
- 25.Binnie V, McHugh S, Jenkins W, Borland W, Macpherson L. A randomised controlled trial of a smoking cessation intervention delivered by dental hygienists: a feasibility study. BMC Oral Health. 2007;7:5–5. doi: 10.1186/1472-6831-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fiore MC, Jaen CR, Baker TB, et al. Clinical Practice Guideline. Rockville, MD: U.S. Department of Health and Human Services. Public Health Service; 2008. Treating Tobacco Use and Dependence: 2008 Update. [Google Scholar]
- 27.U.S. Department of Health and Human Services. Healthy People. Washington, DC: U.S. Department of Health and Human Services, Office of Disease Prevention and Health Promotion; 2020. [Accessed September 6, 2011]. Available at http://www.healthypeople.gov/2020. [Google Scholar]
- 28.Albert D, Severson H, Gordon J, Ward A, Andrews J, Sadowsky D. Tobacco attitudes, practices, and behaviors: a survey of dentists participating in managed care. Nicotine Tob Res. 2005;7(Suppl 1):S9–S18. doi: 10.1080/14622200500078014. [DOI] [PubMed] [Google Scholar]
- 29.Succar CT, Hardigan PC, Fleisher JM, Godel JH. Survey of tobacco control among Florida dentists. J Community Health. 2011;36:211–218. doi: 10.1007/s10900-010-9299-5. [DOI] [PubMed] [Google Scholar]
- 30.Dolan TA, McGorray SP, Ginstead-Skigen CL, Mecklenburg R. Tobacco control activities in U.S. dental practices. JADA. 1997;128(12):1669–1679. doi: 10.14219/jada.archive.1997.0129. [DOI] [PubMed] [Google Scholar]
- 31.Gordon J, Lichtenstein E, Severson H, Andrews J. Tobacco cessation in dental settings: research findings and future directions. Drug Alcohol Rev. 2006;25(1):27–37. doi: 10.1080/09595230500459495. [DOI] [PubMed] [Google Scholar]
- 32.Simoyan O, Badner V, Freeman K. Tobacco cessation services in dental offices. Are we doing all we can? NY State Dent J. 2002;68(7):34–40. [PubMed] [Google Scholar]
- 33.Jones RB. Tobacco or oral health: Past progress, impending challenge. J Am Dent Assoc. 2000;131:1130–1136. doi: 10.14219/jada.archive.2000.0345. [DOI] [PubMed] [Google Scholar]
- 34.Morbidity and Mortality Weekly Report. 43. Vol. 60. Atlanta, GA: Centers for Disease Control and Prevention; 2011. Vital signs: Overdoses of prescription opioid pain relievers --- United States, 1999–2008; pp. 1487–1492. [PubMed] [Google Scholar]
- 35.Denisco RC, Kenna GA, O’Neil MG, et al. Prevention of prescription opioid abuse: the role of the dentist. J Am Dent Assoc. 2011;142(7):800–810. doi: 10.14219/jada.archive.2011.0268. [DOI] [PubMed] [Google Scholar]
- 36.Volkow ND, McLellan TA, Cotto JH, Karithanom M, Weiss SR. Characteristics of opioid prescriptions in 2009. JAMA. 2011;305(13):1299–1301. doi: 10.1001/jama.2011.401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Esmeili T, Ellison J, Walsh MM. Dentists’ attitudes and practices related to diabetes in the dental setting. J Public Health Dent. 2010;70(2):108–114. doi: 10.1111/j.1752-7325.2009.00150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Greenberg BL, Glick M, Goodchild J, Duda PW, Conte NR, Conte M. Screening for cardiovascular risk factors in a dental setting. J Am Dent Assoc. 2007;138(6):798–804. doi: 10.14219/jada.archive.2007.0268. [DOI] [PubMed] [Google Scholar]
- 39.Greenberg BL, Glick M, Frantsve-Hawley J, Kantor ML. Dentists’ attitudes toward chairside screening for medical conditions. J Am Dent Assoc. 2010;141(1):52–62. doi: 10.14219/jada.archive.2010.0021. [DOI] [PubMed] [Google Scholar]
- 40.Pollack HA, Metsch LR, Abel S. Dental examinations as an untapped opportunity to provide HIV testing for highrisk individuals. Am J Public Health. 2010;100(1):88–89. doi: 10.2105/AJPH.2008.157230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.McRee B. Open wide! Dental settings are an untapped resource for substance misuse screening and brief intervention. Addiction. 2012;107(7):1197–1198. doi: 10.1111/j.1360-0443.2012.03777.x. [DOI] [PubMed] [Google Scholar]
- 42.Substance Abuse and Mental Health Services Administration. Treatment Improvement Protocol (TIP) Series No. 24. Rockville, MD: U.S. Department of Health and Human Services. Substance Abuse and Mental Health Services Administration; 1997. A guide to substance abuse services for primary care clinicians. [PubMed] [Google Scholar]
- 43.Substance Abuse and Mental Health Services Administration. [Accessed August 14, 2012];White paper on screening, brief intervention and referral to treatment (SBIRT) in behavioral healthcare. 2011 Apr; Available at http://www.samhsa.gov/prevention/sbirt/SBIRTwhitepaper.pdf.
- 44.Needleman I, Warnakulasuriya S, Sutherland G, et al. Evaluation of tobacco use cessation (TUC) counseling in the Dental Office. Oral Health Prev Dent. 2006;4(1):27–47. [PubMed] [Google Scholar]
- 45.Makhija SK, Gilbert GH, Rinda DB, et al. Dentists in practice-based research networks have much in common with dentists at large: evidence from the Dental Practice-Based Research Network. Gen Dent. 2009;57(3):270–275. [PMC free article] [PubMed] [Google Scholar]
- 46.American Dental Association Survey Center. [Accessed October 14, 2011];2009 Survey of dental practice: Characteristics of dentists in private practice and their patients. 2010 Available at http://www.ada.org/1443.aspx. [Google Scholar]
- 47.Albert D, Ward A, Ahluwalia K, Sadowsky D. Addressing tobacco in managed care: A survey of dentists’ knowledge, attitudes, and behaviors. Am J Public Health. 2002;92(6):997–1001. doi: 10.2105/ajph.92.6.997. [DOI] [PMC free article] [PubMed] [Google Scholar]