Abstract
The incidence of stroke is substantially higher among hemodialysis patients than among patients with earlier stages of CKD, but to what extent the initiation of dialysis accelerates the risk for stroke is not well understood. In this cohort study, we analyzed data from incident hemodialysis and peritoneal dialysis patients in 2009 who were at least 67 years old and had Medicare as primary payer. We noted whether each of the 20,979 hemodialysis patients initiated dialysis as an outpatient (47%) or inpatient (53%). One year before initiation, the baseline stroke rate was 0.15%–0.20% of patients per month (ppm) for both outpatient and inpatient initiators. Among outpatient initiators, stroke rates began rising approximately 90 days before initiation, reached 0.5% ppm during the 30 days before initiation, and peaked at 0.7% ppm (8.4% per patient-year) during the 30 days after initiation. The pattern was similar among inpatient initiators, but the stroke rate peaked at 1.5% ppm (18% per patient-year). For both hemodialysis groups, stroke rates rapidly declined by 1–2 months after initiation, fluctuated, and stabilized at approximately twice the baseline rate by 1 year. Among the 620 peritoneal dialysis patients, stroke rates were slightly lower and variable, but approximately doubled after initiation. In conclusion, these data suggest that the process of initiating dialysis may cause strokes. Further studies should evaluate methods to mitigate the risk for stroke during this high-risk period.
Patients with stage 3–5 CKD (defined as an estimated GFR <60 ml/min per 1.73 m2) have an elevated risk of stroke compared with non-CKD patients1,2; this risk increases further during the first year after hemodialysis initiation.2 The transition period beginning 1 year before and ending 1 year after initiation is marked by well recognized accelerated rates of adverse cardiovascular outcomes and mortality, including higher rates of acute stroke.3,4 The first 90 days after initiation are especially treacherous, because cardiovascular and mortality rates can increase by >50%.5 However, there has been relatively little investigation of the epidemiology of stroke during this transition period, compared with investigation of other cardiovascular outcomes.
In this analysis, we sought to determine to what extent hemodialysis or peritoneal dialysis initiation may accelerate the risk of incident stroke. We measured incident stroke in a cohort of Medicare CKD patients through the hemodialysis and peritoneal dialysis transition periods, beginning 1 year before dialysis initiation and ending 1 year after initiation.
Results
Description of Cohorts
Hemodialysis Inpatient and Outpatient Cohorts
We identified a total of 20,969 incident hemodialysis patients in 2009; 53% were inpatients at the time of hemodialysis initiation. Inpatient and outpatient initiators were the same age (mean 77 years), with similar racial distribution (23% nonwhite), but outpatients were more often men (58% versus 53%) (Table 1). Disease burden was modestly higher for the inpatients, including higher prevalence of atherosclerotic heart disease (ASHD) (41% versus 36%), congestive heart failure (CHF) (34% versus 26%), diabetes (56% versus 51%), chronic obstructive pulmonary disease (COPD) (20% versus 15%), and atrial fibrillation (19% versus 16%).
Table 1.
Cohort characteristics: Incident dialysis patients in 2009 aged ≥67 years at dialysis initiation
| Characteristic | Hemodialysis Patients | Peritoneal Dialysis Patients | |
|---|---|---|---|
| Inpatient Initiation | Outpatient Initiation | ||
| Patients (n) | 11,011 | 9958 | 650 |
| Age (yr) | |||
| Mean | 77.3 | 77.0 | 75.6 |
| Median | 77.0 | 77.0 | 75.0 |
| 65–74 | 4197 (38.1) | 3955 (39.7) | 295 (47.6) |
| 75–84 | 5144 (46.7) | 4542 (45.6) | 271 (43.7) |
| ≥ 85 | 1670 (15.2) | 1461 (14.7) | 54 (8.7) |
| Race | |||
| White | 8478 (77.0) | 7694 (77.3) | 521 (84.0) |
| Black | 2086 (18.9) | 1754 (17.6) | 67 (10.8) |
| Other/unknown | 447 (4.1) | 510 (5.1) | 32 (5.2) |
| Sex | |||
| Men | 5790 (52.6) | 5734 (57.6) | 341 (55.0) |
| Women | 5221 (47.4) | 4224 (42.4) | 279 (45.0) |
| Comorbid conditions | |||
| Anemia | 5576 (50.6) | 5383 (54.1) | 360 (58.1) |
| ASHD | 4497 (40.8) | 3546 (35.6) | 190 (30.6) |
| CHF | 3692 (33.5) | 2605 (26.2) | 132 (21.3) |
| COPD | 2173 (19.7) | 1528 (15.3) | 66 (10.6) |
| Diabetes | 6141 (55.8) | 5040 (50.6) | 303 (48.9) |
| Atrial fibrillation | 2137 (19.4) | 1583 (15.9) | 87 (14.0) |
| Hypertension | 9003 (81.8) | 7992 (80.3) | 528 (85.2) |
| PVD | 2540 (23.1) | 1971 (19.8) | 13 (2.1) |
| Other CVD | 603 (5.5) | 467 (4.7) | 93 (15.0) |
Unless otherwise indicated, values are n (%). PVD, peripheral vascular disease; CVD, cerebrovascular disease.
Peritoneal Dialysis Cohort
Peritoneal dialysis patients (n=620) were slightly younger than hemodialysis outpatient initiators (mean age 75.6 years versus 77.0 years, respectively), more were white (84% versus 77%), and slightly more had anemia and hypertension (Table 1). Disease burden for other comorbid conditions (CHF, COPD) was moderately lower, and history of peripheral vascular disease was almost 10-fold lower (2.1% versus 19.8%).
Stroke Subtypes
Strokes were subtyped as ischemic or hemorrhagic using claims diagnoses. For outpatients during hemodialysis initiation, 92.6% (638 of 689) of strokes were ischemic; for inpatients, 92.2% (939 of 1019) were ischemic. Hemorrhagic strokes were less common before initiation (6.5% of all strokes) than after initiation (7.5%).
Stroke Rates in Relation to Dialysis Initiation
For outpatients during hemodialysis initiation, incident stroke rates hovered around 0.15% of patients per month (ppm), or approximately 2.4% of patients per year (ppy), until 6 months before initiation, when rates increased to 0.2% of patients (Figure 1). Starting 3 months before initiation, stroke rates rose to 0.3% ppm, continued rising to 0.5% ppm at 0–30 days before, and peaked at 0.7% ppm (8.4% ppy) in the first 30 days after initiation, >4 times the baseline rate (P<0.0001). Stroke rates then fluctuated somewhat but remained higher than preinitiation rates, between 0.3% and 0.5% ppm, for a full year after initiation; the rate at 12 months postinitiation was twice the baseline rate, at 0.32% ppm.
Figure 1.
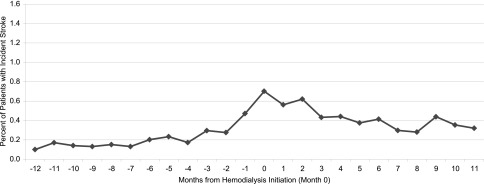
Incident stroke/transient ischemic attack rates for incident hemodialysis patients in 2009 who initiated hemodialysis as outpatients.
For inpatients during hemodialysis initiation, preinitiation incident stroke rates were similar to rates for outpatients, at about 0.20% ppm (Figure 2); rates rose to 0.3%–0.5% ppm within 90 days before initiation, and continued rising to 1.5% ppm (18% ppy), >7 times the baseline preinitiation rate (P<0.0001), during the hospital stay that bracketed hemodialysis initiation. After initiation, rates were 0.7%–0.8% ppm through about 120 days, and remained at 0.4% ppm (4.8% ppy), about double the preinitiation rate, for a full year.
Figure 2.
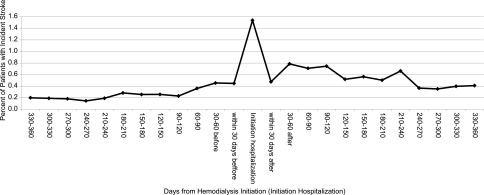
Incident stroke/transient ischemic attack rates for incident hemodialysis patients in 2009 who initiated hemodialysis as inpatients.
Overall, peak stroke rates during the month of initiation were approximately twice as high among inpatient initiators as among outpatient initiators (1.5% ppm and 18% ppy versus 0.7% ppm and 8.4% ppy), and rates remained about 30% higher after initiation.
Rates of All Strokes Including Recurrent Stroke in Hemodialysis Patients
The pattern for rates of all strokes was similar to the pattern for outpatient and inpatient incident strokes (Figure 3), but began at essentially double the outpatient stroke rates at 0.3% ppm, peaked at 6 times the baseline rate during the month before and month after initiation, and gradually declined to about 0.6 strokes per 100 patient-months at 10–12 months after initiation, or twice the combined baseline rate.
Figure 3.
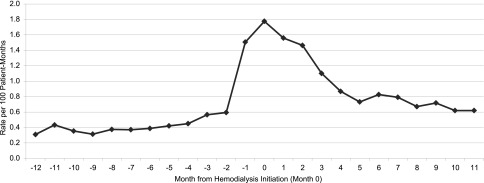
Incident stroke/transient ischemic attack rates for all incident hemodialysis patients, including recurrent stroke, in 2009.
Incident Stroke Rate in Peritoneal Dialysis Patients
In the much smaller incident peritoneal dialysis cohort (n=620), only 38 incident strokes occurred over the transition period, resulting in unstable monthly stroke rates. Stroke rates and frequency patterns overall were similar to rates and patterns for incident outpatient hemodialysis patients. Rates approximately doubled during most of the postinitiation period, but fluctuated widely month to month. Stroke rates ranged from 0% to 0.32% ppm from 12 months to 4 months before initiation, increased to 0.64% ppm at 3 months before and at 3 months after initiation, peaked at 1.17% ppm at 7 months after initiation, fluctuated, and declined to 0 strokes at 11 months after initiation (not shown).
Risk Factor Analyses for Incident Stroke before and after Hemodialysis Initiation
We conducted two separate analyses of factors associated with stroke using Cox regression models, one for strokes occurring before hemodialysis initiation, and another for strokes occurring after initiation; both used as predictors factors identified 13–24 months before the defined transition period (Table 2). Factors associated with increased risk of preinitiation stroke were black race (odds ratio [OR], 1.36; 95% confidence interval [95% CI], 1.12 to 1.66; P=0.002), female sex (OR, 1.31; 95% CI, 1.10 to 1.55; P=0.001), ASHD (OR, 1.28; 95% CI, 1.06 to 1.55; P=0.01), and hypertension (OR, 1.37; 95% CI, 1.06 to 1.78; P=0.018). Factors associated with lower risk of preinitiation stroke included anemia (OR, 0.79; 95% CI, 0.67 to 0.95; P=0.01) and CHF (OR, 0.81; 95% CI, 0.65 to 0.99; P=0.04).
Table 2.
Risk factors associated with strokes occurring before and after hemodialysis initiation
| Risk Factors | Hazard Ratio (95% CI) | P |
|---|---|---|
| Strokes before initiation | ||
| Age | 1.00 (0.98 to 1.01) | 0.61 |
| Black race | 1.36 (1.12 to 1.66) | 0.002 |
| Other race | 0.85 (0.55 to 1.31) | 0.46 |
| Female sex | 1.31 (1.10 to 1.55) | 0.001 |
| Anemia | 0.79 (0.67 to 0.95) | 0.01 |
| ASHD | 1.28 (1.06 to 1.55) | 0.01 |
| Cancer | 0.90 (0.70 to 1.17) | 0.44 |
| CHF | 0.81 (0.65 to 0.99) | 0.04 |
| COPD | 1.07 (0.86 to 1.32) | 0.57 |
| Diabetes | 1.14 (0.95 to 1.37) | 0.15 |
| Atrial fibrillation | 1.05 (0.84 to 1.32) | 0.66 |
| GI disease | 1.15 (0.82 to 1.61) | 0.43 |
| Hypertension | 1.37 (1.06 to 1.78) | 0.02 |
| Liver disease | 0.45 (0.19 to 1.08) | 0.08 |
| Other cardiac | 1.00 (0.80 to 1.24) | 0.99 |
| PVD | 1.16 (0.95 to 1.41) | 0.14 |
| Strokes after initiation | ||
| Age | 1.02 (1.01 to 1.03) | <0.0001 |
| Black race | 1.12 (0.97 to 1.30) | 0.12 |
| Other race | 0.91 (0.68 to 1.20) | 0.49 |
| Female sex | 1.48 (1.31 to 1.67) | <0.0001 |
| Anemia | 0.92 (0.81 to 1.08) | 0.21 |
| ASHD | 1.07 (0.93 to 1.23) | 0.34 |
| Cancer | 0.88 (0.73 to 1.06) | 0.19 |
| CHF | 0.92 (0.79 to 1.08) | 0.30 |
| COPD | 0.98 (0.83 to 1.15) | 0.76 |
| Diabetes | 1.17 (1.03 to 1.33) | 0.02 |
| Atrial fibrillation | 1.02 (0.87 to 1.21) | 0.79 |
| GI disease | 0.98 (0.75 to 1.27) | 0.88 |
| Hypertension | 0.86 (0.73 to 1.02) | 0.08 |
| Liver disease | 1.02 (0.64 to 1.60) | 0.95 |
| Other cardiac | 1.08 (0.93 to 1.27) | 0.33 |
| PVD | 1.08 (0.93 to 1.24) | 0.33 |
PVD, peripheral vascular disease; GI, gastrointestinal.
After initiation, factors associated with incident stroke were age (OR, 1.02; 95% CI, 1.01 to 1.03 per year >67 years; P<0.001), female sex (OR, 1.48; 95% CI, 1.31 to 1.67; P<0.001), and diabetes mellitus (OR, 1.17; 95% CI, 1.03–1.33; P=0.02).
Of note, atrial fibrillation was not found to be associated with incident stroke before or after initiation.
Characteristics of Patients with Incident Stroke before and after Initiation
We also measured characteristics of patients who experienced stroke after dialysis initiation compared with patients who experienced stroke before initiation. Patients who experienced stroke after initiation were somewhat older (mean age 77.8 versus 76.9 years) and slightly more likely to be white and female, and had less hypertension (80.7% versus 86.1%) and ASHD (38.2% versus 43.4%), but a markedly greater prevalence of COPD (16.8% versus 2.2%), than those who experienced stroke before initiation. There were no other substantial differences between the two groups (not shown).
Discussion
In this cohort of Medicare-insured incident dialysis patients, the incidence of stroke began to increase about 3 months before dialysis initiation and peaked during the month of hemodialysis initiation at >4 times the baseline rate in outpatient initiators and 7 times the baseline rate in inpatient initiators. In both groups, stroke rates rapidly declined by 1–2 months after initiation, then fluctuated and gradually stabilized at approximately twice the baseline rate by 1 year after initiation. Peak stroke rates during the month of initiation were approximately twice as high for inpatient as for outpatient initiators, and the rate remained about 30% higher for inpatient initiators after initiation. Among peritoneal dialysis patients, stroke rates overall were slightly lower and very unstable, but rates approximately doubled after initiation.
To our knowledge, no previous study has described the trajectory of incident stroke over the dialysis transition period. However, several previous studies have measured the incident stroke rate after initiation in incident dialysis patients over varying time intervals.
The Choices for Healthy Outcomes in Caring for ESRD (CHOICE) study measured cerebrovascular event rates after dialysis initiation in 1061 incident hemodialysis (73%) and peritoneal dialysis (27%) patients aged ≥18 years in the United States over a median 2.7 years of follow-up.6 The incidence rate during the first 2 years after dialysis initiation was 20.9 per 100 patient-years, including approximately 3% of patients who underwent carotid endartectomy; this is comparable with our peak rate of 1.5% ppm, or approximately 18% ppy, for inpatients during hemodialysis initiation, excluding carotid endartectomy patients. The CHOICE event rate was also likely somewhat higher because CHOICE did not exclude patients with previous stroke.
In the US Renal Data System (USRDS) Dialysis Morbidity and Mortality Studies, Waves 2–4 (DMMS 2–4), the incident rate for hospitalized or fatal stroke was 33 per 1000 patient-years (3.3 per 100 patient-years) among combined prevalent and incident dialysis patients,7 but the rate in incident hemodialysis patients was not reported separately. In a study of 449 incident dialysis patients with a mean age of 64 years in Spain,8 stroke incidence over approximately the first 3 years of dialysis was 2.4 per 100 patient-years, but incidence over the first year and in the time period preceding dialysis initiation was not described separately.
Risk Factors for Incident Stroke before and after Initiation
The risk factor analyses for incident stroke occurring before and after initiation shed minimal light on the pathophysiology of incident stroke in this dialysis cohort; the nonmodifiable demographic factors of age, black race, and female sex predominated. Hypertension and ASHD were associated with increased risk of incident stroke before initiation, and diabetes after initiation. Except for female sex, all of these are known risk factors for stroke in the general population. Anemia and CHF appeared to be protective against stroke before initiation, but not after initiation. Anemia has been found to be both protective and putative as a risk factor for stroke, with a U-shaped curve describing the relationship between hemoglobin level and acute stroke.9,10 The additional role of erythropoietin-stimulating agents, often prescribed for CKD patients, cannot be measured in this study. A history of chronic compensated CHF (assessed 1–2 years before initiation) could be protective against acute insults before initiation relative to acute decompensated CHF at or after initiation, but this association requires further assessment.
The risk factor analysis did not find COPD to be a significant predictor, but COPD was about 10-fold more common in hemodialysis patients who incurred stroke after initiation. COPD is a risk factor for stroke and is associated with carotid wall thickening.11,12 Low baseline oxygenation reserve may predispose patients with COPD to higher stroke risk at dialysis initiation.
In the DMMS 2–4 study using hospital discharge records, age, black race without previous cardiovascular disease, elevated systolic BP, diabetes, anemia (hemoglobin <9.0 g/dl), hypoalbuminemia, and malnutrition were strongly associated with incident stroke.7 In the Spanish study of 449 incident hemodialysis patients, age, diabetes, and atrial fibrillation were independent predictors of stroke.8
Although atrial fibrillation was highly prevalent at 19% among inpatient hemodialysis initiators, it was not a risk factor for stroke in our study. However, our risk factor analyses excluded patients with a previous stroke; these patients may have had higher prevalence of atrial fibrillation. The anticoagulation status of these patients before and after dialysis is also unknown. Although anticoagulation for atrial fibrillation decreases the risk of stroke in non-CKD patients, anticoagulation use in dialysis patients is controversial.13–15 It is also possible that the effect of the dialysis initiation process itself was so powerful that it overwhelmed the usual effect of atrial fibrillation as a moderately strong risk factor.
Female sex was associated with moderately high (24%–49%) increased risk of stroke in our study, unlike in previous studies.7,8 This requires further exploration, although female sex has been associated with increased risk of atrial fibrillation in incident hemodialysis patients.16
Acceleration of Incident Stroke before Hemodialysis Initiation
In our study, the incident stroke rate began to increase about 3 months before hemodialysis initiation, and peaked during the month of initiation. The predialysis stroke increase may reflect acceleration of the shared inflammatory load and vascular endothelial pathology in the brains and kidneys of these CKD patients, in turn triggering negative outcomes in either end organ in both hemodialysis and peritoneal dialysis patients. Baseline silent brain infarction on brain magnetic resonance imaging predicts accelerated decline in estimated GFR and increased risk of hemodialysis initiation in stage 3–5 CKD patients over 2 years of follow-up.17 CHF, with attendant circulatory congestion and volume-driven hypertension, could contribute to increased stroke risk shortly before dialysis initiation, and was prevalent in about one-third of both inpatient and outpatient hemodialysis initiators, but it appeared to be protective in our risk factor analysis (OR, 0.80). However, we measured prevalent CHF or history of previous CHF; incident decompensated CHF may be more likely to trigger stroke by potentially decreasing cerebral perfusion.
For some stroke patients, the stroke itself many have led to acute-on-chronic renal disease with subsequent ESRD, due to secondary complications of stroke (e.g., aspiration or other pneumonias or sepsis).
Dialysis initiation can occur in many different settings, which may complicate accurate ascertainment of first maintenance dialysis treatment. Misclassification of dialysis initiation timing may contribute to the spread of the stroke incidence peak over the time period immediately surrounding initiation. For example, the first hemodialysis session may occur during hospitalization for acute-on-chronic renal failure, before thrice-weekly maintenance dialysis begins; some patients begin with only 1–2 dialysis sessions per week. In addition, Medicare claims for hemodialysis can be delayed for a month or longer after initiation.
The Hemodialysis Process and Stroke
Evidence from observational cohort and imaging studies indicates that the hemodialysis procedure may itself induce strokes. For example, among 151 Japanese hemodialysis patients with acute stroke, 39.5% of 86 brain infarcts and 34.7% of 58 brain hemorrhages occurred during or <30 minutes after a dialysis session; the remainder occurred at other unspecified times.18 In the CHOICE cohort, of 90 strokes in hemodialysis patients with chart abstraction, 10 occurred during dialysis, 17 at another time that day, 35 on a nondialysis day, and 28 at an indeterminate time after last dialysis.6
Significantly decreased cerebral perfusion and blood flow velocity after versus before dialysis have been documented using Xenon inhalation scans of cerebral circulation19 and transcranial Doppler ultrasonography of the cerebrovascular arteries.20–22 Positron emission tomography scans also show decreased cerebral oxygen metabolism and regional blood flow in hemodialysis patients; cerebral blood flow in the frontal lobes and white matter is inversely related to dialysis duration.23 The number of intradialytic hypotensive episodes correlates with the degree of frontal cerebral atrophy on magnetic resonance imaging.24
The stroke rate decreased in the months after dialysis initiation but remained approximately twice the baseline rate by 1 year. This stabilization may represent partial recovery of cerebrovascular autoregulation in response to acute volume and electrolyte shifts after the first months of dialysis sessions. It may also be a survivor phenomenon, with dialysis functioning as a stress test; patients who were most susceptible to stroke in our study, such as those with obstructive carotid (or other vascular territory) disease, had already experienced a stroke or died within the first few months after dialysis initiation, resulting in a less-susceptible remaining population.
Potential Interventions to Decrease the Rate of Incident Stroke
Whether reducing the rate (K) of clearance through longer, slower dialysis might reduce the risk of cerebral edema and/or hypoperfusion and thus limit the risk of recurrent ischemic episodes during dialysis needs further exploration. Of note, in Europe, the average dialysis session lasts 4–4.5 hours, compared with about 3.5 hours in the United States. Studies in Europe, Japan, and the United States report that dialysis sessions longer than 4 hours are associated with 19%–50% lower adjusted mortality rates.25,26 However, comparative stroke rates with different dialysis session durations have not been described. The Frequent Hemodialysis Network study may offer the opportunity to evaluate the effect of shorter, more frequent hemodialysis on risk of stroke, because it compares outcomes of standard thrice-weekly hemodialysis to 5 or 6 sessions of daily or nocturnal dialysis per week.27
Potential modifications of standard thrice-weekly hemodialysis delivery include administering oxygen during dialysis (especially to patients with COPD) to decrease risk of cerebral hypoxemia secondary to cerebral ischemia, placing patients in the Trendelenburg position intermittently, or prescribing compression stockings or leg pumps to increase cerebral perfusion. To our knowledge, none of these interventions has been attempted in a clinical trial to decrease risk of incident stroke. In addition, women, who were at increased risk of stroke in our study, could be targeted for more aggressive primary and secondary stroke risk factor reduction.
Limitations
We were unable to identify the timing of incident stroke relative to initiation of maintenance hemodialysis, or relative to other acute events, among patients who initiated as inpatients, because date of stroke is not identified on hospital claims for incident stroke. Survival bias before dialysis initiation and known high mortality due to stroke after initiation likely contribute to the pattern of stroke incidence observed. Rates of symptomatic stroke reported here likely underestimate the true burden of stroke in incident hemodialysis patients, based on high rates of subclinical infarction evident on brain imaging in the dialysis population.28 Although we used a previously validated coding algorithm to identify stroke events,29 misclassification of stroke status and of other comorbid conditions may have occurred. Likewise, misclassification of dialysis initiation date may have occurred due to limitations related to accurate completion of the Medical Evidence Report (Centers for Medicare & Medicaid [CMS] form CMS-2728) and the USRDS database. We did not have access to laboratory values and medications for risk factor analyses because these data were not consistently available in Medicare claims. Lastly, use of Medicare claims diagnoses for risk factor analysis of incident stroke during hospitalization is inexact, because exact timing of inpatient stroke and acute events before stroke are not documented on claims. For this reason we used pre-transition zone identification of potential risk factors. A more detailed risk factor analysis would require a prospective longitudinal study examining daily electronic medical records to establish a time course of risk factors and incident stroke.
The incident stroke rate increased 4- to 7-fold during the month surrounding hemodialysis initiation, and stabilized at double the baseline rate by approximately 1 year after initiation. This stroke rate trajectory strongly suggests that the process of hemodialysis may cause strokes. Further study is needed to evaluate risk factors for stroke in incident hemodialysis patients, and determine whether modifications to the dialysis dose or duration of dialysis sessions, adjunct supportive treatment during dialysis, or alternative methods of dialysis delivery such as more frequent hemodialysis, might decrease the risk of incident stroke.
Concise Methods
We identified a cohort of incident hemodialysis and peritoneal dialysis patients in 2009 aged ≥67 years at initiation with Medicare as primary payer for 2 years before initiation. Patients with any stroke-related claim during months 13–24 before initiation were excluded; relevant International Classification of Diseases, Ninth Edition, Clinical Modification (ICD-9-CM) codes were 430.×, 431.×, 433. × 1, 434.×, 435.×, 436.×, 437.× (other and ill-defined cerebrovascular disease), and 438.× (late effects of cerebrovascular disease). Date of dialysis initiation was obtained from the USRDS database using the CMS Medical Evidence Report (form CMS-2728), which is required for Medicare coverage of dialysis.
Strokes were identified during the 12 months before and after initiation, or until death or change in treatment modality (defined as change to peritoneal dialysis or home dialysis, or kidney transplant). Incident strokes were identified by occurrence of one outpatient, inpatient, or skilled nursing facility claim. Patients classified with incident stroke were removed from the denominator for the remaining follow-up time.
Calculation of Stroke Frequency
Because time at risk during the hospital stay is not clearly definable by months at risk (because most lengths of stay are less than 1 month), we calculated frequency of strokes as the percentage of patients in each month of observation who had an incident stroke, referred to as percent of patients per month. (This calculation is not the same as a per-patient-per-month rate, but in most months matched a per-patient-per-month rate because approximately 100 patients were at risk in most months). This percent-of-patients-per-month rate can be multiplied by 12 to calculate the approximate percentage of patients per year with incident stroke, based only on that month’s stroke frequency. Strokes were identified from ICD-9-CM diagnosis codes on Medicare claims (in any position). A stroke event was defined as presence of one inpatient or skilled nursing facility Medicare claim for stroke, including claims for ischemic (433.×1, 434.×, 436.×) and hemorrhagic (430.×, 431.×) strokes. Diagnosis code 435.× represents transient ischemic attack; incident strokes were identified including this code for completeness. Stroke claims with traumatic brain injury or rehabilitation listed as the principal diagnosis code were excluded, using a previously validated stroke identification methodology by Tirschwell and Longstreth.29
Comorbid conditions were identified by one inpatient or two outpatient or Part B Medicare claims for that condition, with the exception of atrial fibrillation, which was identified by one inpatient or one outpatient Part B claim. For all patients, comorbid conditions were identified from claims from 13 to 24 months before initiation.
Patients were stratified by whether dialysis initiation occurred in an inpatient hospital setting. Patients who were hospitalized with an admission date before their dialysis initiation date and a discharge date after their dialysis initiation date were considered to be inpatients during hemodialysis initiation; patients not meeting this definition were considered to be outpatients during dialysis initiation. Rates were calculated separately for inpatient and outpatient groups.
To determine whether the observed accelerated incident stroke pattern after initiation persisted when recurrent strokes were included, we also measured the rate of all new inpatient and outpatient strokes combined that occurred over the 2-year observation period, including recurrent strokes, and including patients who experienced a stroke during the 1 year preceding our observation period.
For the analyses of potential risk factors for incident stroke among inpatient hemodialysis initiators, a Cox model was used to estimate the adjusted hazard ratio of incident stroke, both before and after initiation. This was done separately for incident stroke before dialysis initiation and incident stroke after dialysis initiation for patients with no stroke before initiation. In each case, comorbid conditions were identified from claims during the 13–24 months before dialysis initiation. Factors were measured before the transition period because it was not possible to assess their timing in relation to each stroke that occurred during the transition period or during the hospitalization for initiation. Separately, we also compared characteristics of patients who experienced stroke before initiation (−12 months to −1 month) with characteristics of patients who experienced stroke after initiation.
Disclosures
None.
Acknowledgments
The authors thank USRDS colleagues Beth Forrest for regulatory assistance, Anne C. Shaw for manuscript preparation, and Nan Booth, MSW, MPH, ELS, for manuscript editing.
This study was performed as a deliverable under Contract HHSN267200715002C (National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health, Bethesda, Maryland). The interpretation and reporting of these data are the responsibility of the authors and in no way should be seen as an official policy or interpretation of the US government.
Preliminary analyses for this manuscript were presented in the 2009 USRDS Annual Data Report, as well as at the 2009 Annual Meeting of the American Society of Nephrology, October 27 through November 1, 2009, in San Diego, California.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
References
- 1.Lee M, Saver JL, Chang KH, Liao HW, Chang SC, Ovbiagele B: Low glomerular filtration rate and risk of stroke: Meta-analysis. BMJ 341: c4249, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.US Renal Data System : Morbidity & mortality. Neuroepidemiology: Incident & prevalent stroke. In: USRDS 2006 Annual Data Report: Atlas of Chronic Kidney Disease & End-Stage Renal Disease in the United States, Vol. 1, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2006, p 140 [Google Scholar]
- 3.US Renal Data System: USRDS 2008 Annual Data Report: Atlas of Chronic Kidney Disease & End-Stage Renal Disease in the United States, Vol. 2, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2008, pp 50–60, 66–71 [Google Scholar]
- 4.US Renal Data System : USRDS 2012 Annual Data Report: Atlas of Chronic Kidney Disease & End-Stage Renal Disease in the United States, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2012, p 262 [Google Scholar]
- 5.US Renal Data System : USRDS 2010 Annual Data Report: Atlas of Chronic Kidney Disease & End-Stage Renal Disease in the United States, Vol. 2, Bethesda, MD, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, 2010, pp 228–229, 302 [Google Scholar]
- 6.Sozio SM, Armstrong PA, Coresh J, Jaar BG, Fink NE, Plantinga LC, Powe NR, Parekh RS: Cerebrovascular disease incidence, characteristics, and outcomes in patients initiating dialysis: The choices for healthy outcomes in caring for ESRD (CHOICE) study. Am J Kidney Dis 54: 468–477, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seliger SL, Gillen DL, Longstreth WT, Jr, Kestenbaum B, Stehman-Breen CO: Elevated risk of stroke among patients with end-stage renal disease. Kidney Int 64: 603–609, 2003 [DOI] [PubMed] [Google Scholar]
- 8.Sánchez-Perales C, Vázquez E, García-Cortés MJ, Borrego J, Polaina M, Gutiérrez CP, Lozano C, Liébana A: Ischaemic stroke in incident dialysis patients. Nephrol Dial Transplant 25: 3343–3348, 2010 [DOI] [PubMed] [Google Scholar]
- 9.Tanne D, Molshatzki N, Merzeliak O, Tsabari R, Toashi M, Schwammenthal Y: Anemia status, hemoglobin concentration and outcome after acute stroke: A cohort study. BMC Neurol 10: 22, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hao Z, Wu B, Wang D, Lin S, Tao W, Liu M: A cohort study of patients with anemia on admission and fatality after acute ischemic stroke. J Clin Neurosci 20: 37–42, 2013 [DOI] [PubMed] [Google Scholar]
- 11.Truelsen T, Prescott E, Lange P, Schnohr P, Boysen G: Lung function and risk of fatal and non-fatal stroke. The Copenhagen City Heart Study. Int J Epidemiol 30: 145–151, 2001 [DOI] [PubMed] [Google Scholar]
- 12.Lahousse L, van den Bouwhuijsen QJ, Loth DW, Joos GF, Hofman A, Witteman JC, van der Lugt A, Brusselle GG, Stricker BH: Chronic obstructive pulmonary disease and lipid core carotid artery plaques in the elderly: The Rotterdam Study. Am J Respir Crit Care Med 187: 58–64, 2013 [DOI] [PubMed] [Google Scholar]
- 13.Chan KE, Lazarus JM, Thadhani R, Hakim RM: Warfarin use associates with increased risk for stroke in hemodialysis patients with atrial fibrillation. J Am Soc Nephrol 20: 2223–2233, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wizemann V, Tong L, Satayathum S, Disney A, Akiba T, Fissell RB, Kerr PG, Young EW, Robinson BM: Atrial fibrillation in hemodialysis patients: Clinical features and associations with anticoagulant therapy. Kidney Int 77: 1098–1106, 2010 [DOI] [PubMed] [Google Scholar]
- 15.Herzog CA, Asinger RW, Berger AK, Charytan DM, Díez J, Hart RG, Eckardt KU, Kasiske BL, McCullough PA, Passman RS, DeLoach SS, Pun PH, Ritz E: Cardiovascular disease in chronic kidney disease. A clinical update from Kidney Disease: Improving Global Outcomes (KDIGO). Kidney Int 80: 572–586, 2011 [DOI] [PubMed] [Google Scholar]
- 16.Vazquez E, Sanchez-Perales C, Garcia-Garcia F, Castellano P, Garcia-Cortes MJ, Liebana A, Lozano C: Atrial fibrillation in incident dialysis patients. Kidney Int 76: 324–330, 2009 [DOI] [PubMed] [Google Scholar]
- 17.Kobayashi M, Hirawa N, Morita S, Yatsu K, Kobayashi Y, Yamamoto Y, Saka S, Toya Y, Yasuda G, Umemura S: Silent brain infarction and rapid decline of kidney function in patients with CKD: A prospective cohort study. Am J Kidney Dis 56: 468–476, 2010 [DOI] [PubMed] [Google Scholar]
- 18.Toyoda K, Fujii K, Fujimi S, Kumai Y, Tsuchimochi H, Ibayashi S, Iida M: Stroke in patients on maintenance hemodialysis: A 22-year single-center study. Am J Kidney Dis 45: 1058–1066, 2005 [DOI] [PubMed] [Google Scholar]
- 19.Gottlieb D, Mildworf B, Rubinger D, Melamed E: The regional cerebral blood flow in patients under chronic hemodialytic treatment. J Cereb Blood Flow Metab 7: 659–661, 1987 [DOI] [PubMed] [Google Scholar]
- 20.Postiglione A, Faccenda F, Gallotta G, Rubba P, Federico S: Changes in middle cerebral artery blood velocity in uremic patients after hemodialysis. Stroke 22: 1508–1511, 1991 [DOI] [PubMed] [Google Scholar]
- 21.Ishida I, Hirakata H, Sugimori H, Omae T, Hirakata E, Ibayashi S, Kubo M, Fujishima M: Hemodialysis causes severe orthostatic reduction in cerebral blood flow velocity in diabetic patients. Am J Kidney Dis 34: 1096–1104, 1999 [DOI] [PubMed] [Google Scholar]
- 22.Hata R, Matsumoto M, Handa N, Terakawa H, Sugitani Y, Kamada T: Effects of hemodialysis on cerebral circulation evaluated by transcranial Doppler ultrasonography. Stroke 25: 408–412, 1994 [DOI] [PubMed] [Google Scholar]
- 23.Kanai H, Hirakata H, Nakane H, Fujii K, Hirakata E, Ibayashi S, Kuwabara Y: Depressed cerebral oxygen metabolism in patients with chronic renal failure: A positron emission tomography study. Am J Kidney Dis 38[Suppl 1]: S129–S133, 2001 [DOI] [PubMed] [Google Scholar]
- 24.Mizumasa T, Hirakata H, Yoshimitsu T, Hirakata E, Kubo M, Kashiwagi M, Tanaka H, Kanai H, Fujimi S, Iida M: Dialysis-related hypotension as a cause of progressive frontal lobe atrophy in chronic hemodialysis patients: A 3-year prospective study. Nephron Clin Pract 97: c23–c30, 2004 [DOI] [PubMed] [Google Scholar]
- 25.Chazot C, Jean G: The advantages and challenges of increasing the duration and frequency of maintenance dialysis sessions. Nat Clin Pract Nephrol 5: 34–44, 2009 [DOI] [PubMed] [Google Scholar]
- 26.Saran R, Bragg-Gresham JL, Levin NW, Twardowski ZJ, Wizemann V, Saito A, Kimata N, Gillespie BW, Combe C, Bommer J, Akiba T, Mapes DL, Young EW, Port FK: Longer treatment time and slower ultrafiltration in hemodialysis: Associations with reduced mortality in the DOPPS. Kidney Int 69: 1222–1228, 2006 [DOI] [PubMed] [Google Scholar]
- 27.Chertow GM, Levin NW, Beck GJ, Depner TA, Eggers PW, Gassman JJ, Gorodetskaya I, Greene T, James S, Larive B, Lindsay RM, Mehta RL, Miller B, Ornt DB, Rajagopalan S, Rastogi A, Rocco MV, Schiller B, Sergeyeva O, Schulman G, Ting GO, Unruh ML, Star RA, Kliger AS, FHN Trial Group : In-center hemodialysis six times per week versus three times per week. N Engl J Med 363: 2287–2300, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Seliger SL, Longstreth WT, Jr, Katz R, Manolio T, Fried LF, Shlipak M, Stehman-Breen CO, Newman A, Sarnak M, Gillen DL, Bleyer A, Siscovick DS: Cystatin C and subclinical brain infarction. J Am Soc Nephrol 16: 3721–3727, 2005 [DOI] [PubMed] [Google Scholar]
- 29.Tirschwell DL, Longstreth WT, Jr: Validating administrative data in stroke research. Stroke 33: 2465–2470, 2002 [DOI] [PubMed] [Google Scholar]


