Abstract
Background
Recent research has linked overall dietary patterns to survival in older adults.
Objectives
The objective of this study was to determine the dietary patterns of a cohort of older adults, and to explore associations of these dietary patterns with survival over a 10-year period. A secondary goal was to evaluate participants’ quality of life and nutritional status according to their dietary patterns.
Design
The Health, Aging, and Body Composition Study is a prospective cohort study of 3,075 older adults. In this study, all-cause mortality was assessed from baseline through Year 10. Food intake was estimated with a modified Block food frequency questionnaire, and dietary patterns of 2,582 participants with complete data were derived by cluster analysis.
Results
Six dietary pattern clusters were identified, including a Healthy Foods cluster, characterized by higher intake of low-fat dairy products, fruit, whole grains, poultry, fish, and vegetables. Both the High-Fat Dairy Products and Sweets and Desserts clusters had a 1.4-fold higher risk of mortality than the Healthy Foods cluster after adjusting for potential confounders. The Healthy Foods cluster also had significantly more years of healthy life and more favorable levels of selected nutritional biomarkers than the other clusters.
Conclusions
A dietary pattern consistent with current guidelines to consume relatively high amounts of vegetables, fruit, whole grains, poultry, fish, and low-fat dairy products may be associated with superior nutritional status, quality of life and survival in older adults.
Between 2000 and 2030, the number of adults worldwide aged 65 years and older is projected to more than double from approximately 420 million to 973 million (1). In the past century, the leading causes of death have shifted from infectious diseases to chronic diseases such as cardiovascular disease and cancer, which may be influenced by diet (2). This has drawn more attention to the effect of diet on mortality. As the older adult population increases, so does the need to identify how dietary choices affect quality of life and survival.
Past studies have primarily assessed dietary components or specific nutrients in relation to health. Dietary pattern analysis, which examines the overall diet, has recently emerged as an alternative approach that may have some advantages (3). Dietary pattern analysis can capture the complexity of the diet because it accounts for the high correlation among intakes of specific foods and nutrients, as well as interactive effects of foods or nutrients, which are often interdependent in their bioavailability. Furthermore, the effects of individual foods or nutrients may be more difficult to detect than that of the diet as a whole. In addition, dietary pattern analysis can enhance our understanding of current dietary practices, provide a way to evaluate health outcomes of those who adhere to dietary guidelines, and produce results that may be directly applicable to updating dietary guidelines.
Dietary patterns have been examined in several ways: an a priori approach involves calculating a score of the overall quality of a diet based on the purported health effects of specific dietary constituents, whereas an empirical a posteriori approach uses the dietary data at hand to identify dietary patterns of the study population independently of their relevance to health. Several studies, predominantly in Europe, have explored associations of diet scores with mortality, and many have employed a Mediterranean diet score (4–13). These studies found inverse relationships between a Mediterranean diet score or a plant-based diet score and mortality. Fewer studies have investigated the associations of empirical dietary patterns with mortality, especially in the United States. The objective of this study was to determine the dietary patterns of a US cohort of older adults and to explore associations of these dietary patterns with survival over a 10-year period.
SUBJECTS AND METHODS
Study Population
Participants aged 70 to 79 years were recruited for the Health, Aging, and Body Composition (Health ABC) Study, a prospective cohort study, from a random sample of white Medicare beneficiaries and all age-eligible black residents in selected areas of Pittsburgh, PA, and Memphis, TN. Individuals were eligible for Health ABC if they planned to remain in the area for at least 3 years and reported no life-threatening cancers and no difficulty with basic activities of daily living, walking one-quarter mile or climbing 10 steps. Those who used assistive devices were excluded, as were participants in any research studies that involved medications or modification of eating or exercise habits. All participants provided informed consent, and institutional review board approval was obtained at both clinical centers (University of Memphis, Memphis, TN, and University of Pittsburgh, Pittsburgh, PA) and at the University of California, San Francisco, Coordinating Center. An interview on behavior, health status, and social, demographic, and economic factors, and a clinical examination of body composition, biochemical variables, weight-related health conditions, and physical function were administered between 1997 and 1998, with subsequent follow-up assessments.
Data from baseline through Year 10 of the Health ABC Study were used in this analysis. The sample size for this study was 2,582, after excluding participants who did not have a dietary assessment (n=343); men who reported an energy intake <800 kcal/day or >4,000 kcal/day and women who reported an energy intake <500 kcal/day or >3,500 kcal/day (n=103); and those with incomplete information on control variables of interest (n=47).
Dietary Assessment
Food intake was measured during Year 2 of the Health ABC Study, at the first annual follow-up visit, with a 108-item food frequency questionnaire (FFQ). The FFQ reference period was the preceding year. This FFQ was designed specifically for the Health ABC Study by Block Dietary Data Systems (Berkeley, CA), based on reported intakes of non-Hispanic white and black residents of the Northeast and South older than age 65 years in the third National Health and Nutrition Examination Survey. The FFQ was administered by a trained dietary interviewer, and interviews were periodically monitored to assure quality and consistency. Wood blocks, real food models, and flash cards were used to help participants estimate portion sizes. Nutrient and food group intakes were determined by Block Dietary Data Systems. A Healthy Eating Index score, which reflects how well the diet conforms to the recommendations of the Dietary Guidelines for Americans and the Food Guide Pyramid, was also calculated for each participant (14).
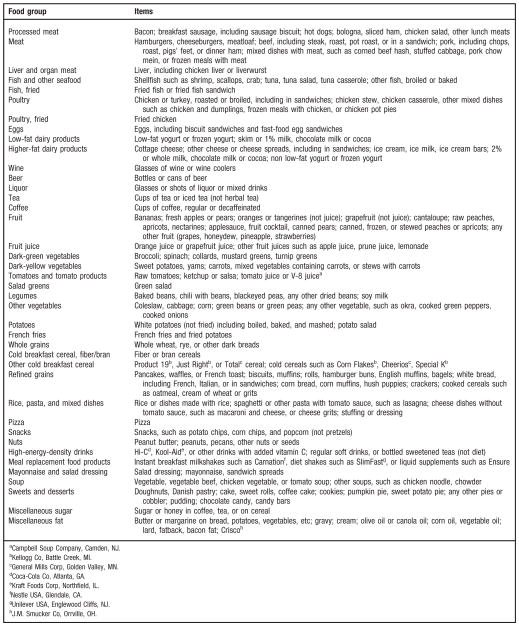
In this study, individuals were grouped according to their overall dietary patterns by cluster analysis, based on methods used in previous studies (15,16). The purpose of the cluster analysis was to place individuals into mutually exclusive groups such that persons in a given cluster had similar diets that differed from those of persons in other clusters. First, the 108 FFQ food items were consolidated into 40 food groups according to similarity in nutrient content (see the Figure). The percentage of energy contributed by each food group for each participant was calculated and used in the cluster analysis. The reason for this standardization was to account for differences in total energy needs due to sex, age, body size, and level of physical activity.
Figure.
Food groupings used in the Health, Aging, and Body Composition Study dietary pattern analysis.
The FASTCLUS procedure in SAS (version 9.1, 2003, SAS Institute Inc, Cary, NC) was used to generate dietary pattern clusters. This procedure requires the number of clusters to be specified in advance, and generates mutually exclusive clusters by comparing Euclidean distances between each subject and each cluster center in an interactive process using a k-means method. The k-means method of clustering is sensitive to outliers, which tend to be selected as the original cluster centers. For this reason, an initial cluster analysis was conducted with a predefined number of 20 clusters, and only seeds of clusters with more than 20 members from this initial analysis were used in subsequent analyses with different numbers of clusters. Cluster analysis requires advance selection of the number of clusters, which is a subjective decision. To determine the most appropriate number of clusters, two to eight cluster solutions were run. A plot of R2, the proportion of variance accounted for by the clusters, vs the number of clusters, and a plot of within-cluster variance vs the number of clusters were examined to assess the ability of the clusters to segregate the study population. A set of six clusters was selected, as this solution most clearly identified distinct and nutritionally meaningful dietary patterns while maintaining a reasonable sample size in each group for subsequent regression analyses. Mean percent energy contributions from food groups were examined according to dietary pattern clusters. Clusters were named according to food groups that on average contributed relatively more to total energy intake.
Biochemical Measures
Fasting glucose and fasting insulin were assessed at baseline, from blood drawn through venipuncture after an overnight fast and stored at −70°C. Plasma glucose was measured by an automated glucose oxidase reaction (YSI 2300 Glucose Analyzer, Yellow Springs Instruments, Yellow Springs, OH), and serum insulin with a commercially available radioimmunoassay kit (Pharmacia, Uppsala, Sweden). Specimens were processed according to standardized protocols by the Laboratory of Clinical Biochemistry at the University of Vermont (17). Serum concentrations of folate, homocysteine, vitamin B-12, and holotranscobalamin, the biologically active fraction of vitamin B-12 and possibly a more pertinent marker of vitamin B12 status, were quantified in a subset of participants during Year 3 of Health ABC. Homocysteine was measured by a fluorescence polarization immunoassay, vitamin B-12 and folate by microbiological methods, and holotranscobalamin by a solid phase radioimmunoassay (18). During Year 2 of Health ABC, the antioxidants vitamin C, beta carotene, and α-tocopherol, the predominant and most active form of vitamin E, were also determined in a subset of participants. Vitamin C was measured by a spectrophotometric assay performed on a robotic chemical analyzer, and beta carotene and α-tocopherol by high pressure liquid chromatography.
Body Composition
Total fat mass, weight, and height were measured at baseline. Total fat mass was assessed by dual energy x-ray absorptiometry (Hologic QDR 4500A, version 9.03, 1998, Hologic, Inc, Waltham, MA). Weight was measured with a standard balance beam scale, and height measured twice with a Harpenden stadiometer (Holtain Ltd, Crosswell, Wales, UK). The two height measurements were averaged, and body mass index was calculated as weight divided by the square of height.
Survival Assessment
All-cause mortality was evaluated from baseline of Health ABC through November 26, 2007. Deaths were identified through attempts to contact participants, notification by proxy, hospital records, local newspaper obituaries, and Social Security Death Index data, and were confirmed by death certificates. Immediate and underlying causes of death were adjudicated by a committee. Survival time was defined as the time between the baseline clinical examination and the date of death and/or date of last contact.
Participants were asked to report their general health every 6 months during in-person examinations or telephone interviews. The number of years of healthy life for each participant was defined as the number of years from baseline through Year 9 of Health ABC in which the participant reported either excellent, very good, or good general health, as opposed to fair or poor health, or if the person was no longer alive.
Sociodemographic and Lifestyle Variables
Sociodemographic variables including age, sex, self-identified racial group and education, and lifestyle variables, including smoking status, alcohol consumption, and physical activity were assessed at baseline of the Health ABC study. Lifetime pack-years of cigarette smoking were calculated by multiplying cigarette packs smoked per day by the number of years of smoking. Physical activity was evaluated by a standardized questionnaire specifically designed for the Health ABC study. This questionnaire was derived from the leisure time physical activity questionnaire and included activities commonly performed by older adults (19). The frequency, duration, and intensity of specific activities were determined, and approximate metabolic equivalent unit values assigned to each activity category to estimate weekly energy expenditure.
Statistical Analysis
Characteristics of men and women were examined by dietary pattern cluster, and each cluster was compared to the Healthy Foods cluster with Dunnett’s test for continuous variables and χ2 test for categorical variables. For the all-cause mortality analyses, the censor date was the reported date of death and/or the documented date of last contact with the participant. The sample size was not sufficient to examine cause-specific mortality by dietary pattern cluster. Cox proportional hazards regression was used to compare the risk of all-cause mortality of each cluster to the Healthy Foods cluster, and models were adjusted for possible confounding factors, including sex, age, race, clinical site, education, physical activity, smoking, and total energy intake. None of the covariates deviated from the proportional hazards assumption required by the Cox regression model. The interaction of dietary pattern and sex was tested, as was the interaction of dietary pattern and race. As these interactions were not found to be significant, analyses were conducted in the study population as a whole. Statistical significance was set at P≤0.05, and analyses were performed using SAS (version 9.1, 2003, SAS Institute Inc, Cary, NC).
RESULTS
Six clusters were identified: Healthy foods (n=374); High-Fat Dairy Products (n=332); Meat, Fried Foods, and Alcohol (n=693); Breakfast Cereal (n=386); Refined Grains (n=458); and Sweets and Desserts (n=339). Table 1 presents mean percent of total energy intake from selected food groups by dietary pattern cluster. The Healthy Foods cluster was characterized by relatively higher intake of low-fat dairy products, fruit, whole grains, poultry, fish and vegetables, and lower consumption of meat, fried foods, sweets, high-energy drinks, and added fat.
Table 1.
Percent of total energy intake from selected food groups by dietary pattern cluster among Health, Aging, and Body Composition Study participants
| Food group | Percent of Total Energy Intake
|
|||||
|---|---|---|---|---|---|---|
| Healthy foods (n=374) | High-fat dairy products (n=332) | Meat, fried foods, and alcohol (n=693) | Breakfast cereal (n=386) | Refined grains (n=458) | Sweets and desserts (n=339) | |
| mean±standard deviation | ||||||
| Processed meat | 1.7±1.9a | 3.0±2.8 | 3.9±3.3 | 2.7±2.8 | 4.1±3.6a | 2.9±2.6 |
| Meat | 2.8±2.7a | 3.7±3.1 | 4.0±3.1a | 3.5±3.1 | 3.7±3.0 | 3.4±2.7 |
| Fish and other seafood | 2.8±2.8a | 1.4±1.8 | 1.7±2.0 | 1.8±2.3 | 1.4±1.9 | 1.3±1.5a |
| Poultry, not fried | 3.4±4.2a | 1.9±2.5 | 2.5±3.1 | 2.1±2.3 | 1.9±2.4 | 1.9±2.3a |
| Fried poultry | 0.4±1.1a | 1.0±1.8 | 1.5±2.6a | 0.7±1.4 | 1.2±2.2 | 0.8±1.5 |
| Low-fat dairy products | 10.4±6.3a | 0.5±1.4a | 1.0±1.9 | 2.3±3.7 | 1.3±2.5 | 1.6±2.9 |
| Higher-fat dairy products | 3.4±2.7a | 17.1±6.0a | 5.1±3.0 | 6.4±3.9 | 5.7±4.0 | 6.2±4.3 |
| Beer | 0.3±1.5a | 0.4±2.0 | 1.2±4.1a | 0.5±2.0 | 0.3±1.8 | 0.4±1.5 |
| Liquor | 0.5±1.8 | 0.5±1.6 | 1.1±3.5a | 0.6±1.8 | 0.4±1.5a | 0.5±2.0 |
| Fruit | 8.3±5.4a | 4.2±3.6 | 4.5±3.7 | 4.8±3.9 | 4.2±4.0 | 3.5±2.9a |
| Dark green vegetables | 0.4±0.5a | 0.2±0.3 | 0.3±0.3 | 0.2±0.3 | 0.3±0.3 | 0.2±0.2a |
| Dark yellow vegetables | 1.0±1.2a | 0.7±0.9 | 0.8±1.0 | 0.7±0.8a | 0.9±1.4 | 0.7±1.0 |
| Other vegetables | 1.4±1.4a | 1.2±1.3 | 1.2±1.3 | 1.1±1.1 | 1.3±1.2 | 1.0±1.1a |
| Whole grains | 5.1±4.6a | 3.0±3.8 | 3.8±4.1 | 2.9±3.7 | 2.0±3.1a | 2.3±2.9 |
| Cold breakfast cereal, fiber/bran | 3.1±3.7 | 2.0±3.1 | 1.6±2.5 | 3.3±4.9a | 1.0±2.0a | 1.6±2.7 |
| Other cold breakfast cereal | 6.9±4.3 | 6.3±4.5 | 4.4±3.4 | 19.3±6.7a | 4.3±4.3a | 5.3±4.2 |
| Refined grains | 10.1±5.3 | 10.9±4.8 | 10.2±4.2 | 9.0±4.9a | 24.6±6.7a | 10.0±5.3 |
| Rice, pasta, and mixed dishes | 3.9±3.8 | 2.9±2.8a | 4.1±3.9a | 3.0±2.8 | 3.1±2.8 | 2.9±2.5 |
| Snacks | 1.4±2.9a | 1.8±3.1 | 2.8±5.2a | 1.6±3.0 | 1.6±2.7 | 2.3±4.0 |
| Nuts | 3.6±4.4 | 3.1±4.0 | 4.6±6.4a | 2.9±4.0a | 3.2±3.8 | 3.1±3.7 |
| High-energy-density drinks | 0.7±1.8a | 2.7±4.7 | 3.8±5.4a | 1.8±3.2 | 2.7±4.3 | 2.1±3.4 |
| Mayonnaise and salad dressing | 3.2±3.3 | 3.9±3.4 | 4.3±3.8a | 3.5±3.1 | 3.2±3.1 | 3.0±2.6a |
| Sweets and desserts | 6.0±4.9a | 6.8±4.8 | 7.1±4.6 | 6.6±5.0 | 6.9±5.3 | 25.8±8.9a |
| Miscellaneous fat | 3.4±3.3a | 4.7±3.8 | 5.8±4.5a | 3.8±3.3 | 5.2±4.0 | 3.9±3.4 |
Cluster with the highest or lowest percent energy contribution from this food group.
As shown in Table 2, the Healthy Foods cluster had a significantly higher percent of women than all other clusters, as well as a higher percent of white participants, a higher level of education, and fewer pack-years of smoking. The Healthy Foods cluster also had a significantly higher percent energy intake from protein, higher intake of fiber, lower percent energy from saturated fat, and lower dietary glycemic index than all other clusters. In addition, the Healthy Foods cluster had a significantly higher level of physical activity, higher percent energy from carbohydrate, lower total energy intake, lower percent energy from total fat, and lower dietary glycemic load than most other clusters. The Healthy Foods cluster also had a significantly higher Healthy Eating Index score and more years of healthy life than any other cluster.
Table 2.
Characteristics of Health, Aging, and Body Composition (Health ABC) Study participants by dietary pattern cluster
| Healthy foods (n=374) | High-fat dairy products (n=332) | Meat, fried foods, and alcohol (n=693) | Breakfast cereal (n=386) | Refined grains (n=458) | Sweets and desserts (n=339) | |
|---|---|---|---|---|---|---|
| mean±standard error | ||||||
| Characteristic | ||||||
| Sex (% men) | 35.8 | 44.9* | 48.8* | 57.0* | 51.3* | 49.3* |
| Age (y)a | 74.1±0.1 | 74.5±0.2 | 73.7±0.1 | 74.2±0.1 | 74.1±0.1 | 74.3±0.2 |
| Race (% white) | 83.4 | 64.8* | 48.1* | 71.0* | 47.8* | 73.2* |
| Education (% completed high school)a | 91.4 | 80.1* | 74.9* | 83.2* | 59.4* | 82.6* |
| Smoking (lifetime pack-years)a | 13.2±1.2 | 20.4±1.6* | 19.6±1.1* | 18.8±1.4* | 19.1±1.3* | 20.7±1.6* |
| Alcohol (% any consumption)a | 58.8 | 47.0* | 53.1 | 51.0* | 38.7* | 55.5 |
| Physical activity (kcal/wk)a | 1,538±127 | 924±85* | 1,071±78* | 1,222±94 | 875±77* | 1,011±105* |
| Body compositiona | ||||||
| Body mass index | 26.7±0.2 | 27.1±0.3 | 28.1±0.2* | 27.5±0.2 | 27.4±0.2 | 26.5±0.2 |
| Total body fat (%) | 35.9±0.4 | 35.1±0.4 | 35.5±0.3 | 34.7±0.4 | 34.4±0.4* | 34.8±0.4 |
| Dietary factorsb | ||||||
| Total energy intake (kcal) | 1,703±28 | 1,903±35* | 1,840±25* | 1,735±28 | 1,848±31* | 2,076±36* |
| % kcal from carbohydrate | 56.9±0.4 | 50.9±0.4* | 50.2±0.3* | 59.2±0.4* | 52.5±0.3* | 52.6±0.3* |
| % kcal from protein | 17.0±0.2 | 14.8±0.1* | 14.3±0.1* | 14.1±0.1* | 14.0±0.1* | 12.7±0.1* |
| % kcal from fat | 27.5±0.3 | 35.6±0.4* | 35.8±0.3* | 28.4±0.3 | 34.6±0.3* | 36.1±0.3* |
| % kcal from saturated fat | 7.5±0.1 | 11.7±0.1* | 9.9±0.1* | 8.1±0.1* | 9.5±0.1* | 10.6±0.1* |
| Total dietary fiber (g) | 20.7±0.4 | 16.4±0.4* | 17.2±0.3* | 17.5±0.3* | 16.7±0.3* | 17.5±0.4* |
| Healthy Eating Index score | 80.8±0.4 | 68.1±0.7* | 67.2±0.4* | 72.8±0.5* | 67.9±0.5* | 63.8±0.7* |
| Quality of life | ||||||
| Years of healthy life | 6.8±0.1 | 6.0±0.2* | 6.0±0.1* | 6.3±0.1* | 5.7±0.1* | 6.1±0.1* |
Values from baseline of the Health ABC study.
Values from Year 2 of the Health ABC study.
Significantly different from the Healthy Foods cluster, at P≤0.05, using Dunnett’s test for continuous variables and χ2 test for categorical variables.
Nutrition-related biomarkers of two subsets of the study population by dietary pattern cluster are presented in Table 3. In these subsets, participants were relatively evenly distributed throughout the six clusters. The Healthy Foods cluster had a significantly higher level of folate, vitamin B-12, holotranscobalamin, and beta carotene and a significantly lower level of homocysteine than most other clusters. The Healthy Foods cluster also had significantly higher levels of vitamin C and α-tocopherol than the Refined Grains cluster.
Table 3.
Nutritional biomarkers of two subsets of Health, Aging, and Body Composition (Health ABC) Study participants by dietary pattern cluster
| Biomarker | n | Healthy foods | High-fat dairy products | Meat, fried foods, and alcohol | Breakfast cereal | Refined grains | Sweets and desserts |
|---|---|---|---|---|---|---|---|
| mean±standard error | |||||||
| Folate (nmol/L)ab | 809 | 83.9±4.0 | 69.1±4.8* | 71.4±2.6* | 76.0±3.5 | 61.9±3.1* | 70.7±4.3 |
| Vitamin B-12 (pmol/L)ac | 803 | 577.6±31.2 | 466.3±24.9* | 455.7±15.9* | 487.2±38.1 | 439.0±22.9* | 405.2±24.3* |
| Holotranscobalamin (pmol/L)ac | 785 | 174.1±12.7 | 140.4±13.6 | 133.0±5.9* | 131.1±9.9* | 114.3±6.5* | 112.5±9.0* |
| Homocysteine (μmol/L)a | 813 | 8.6±0.3 | 9.5±0.3 | 9.4±0.2 | 9.8±0.3* | 9.9±0.3* | 10.4±0.5* |
| Vitamin C (ascorbic acid+dehydroascorbic acid, mg/dL)de | 208 | 35.1±2.2 | 30.2±2.7 | 28.6±1.5 | 29.0±2.1 | 24.6±2.0* | 32.1±2.0 |
| Beta carotene (all-trans, μmol/L)df | 208 | 1.1±0.1 | 0.6±0.2* | 0.7±0.1* | 0.6±0.1* | 0.8±0.1 | 0.7±0.1 |
| Vitamin E (α-tocopherol, μmol/L)dg | 207 | 50.7±4.3 | 39.8±4.3 | 40.0±2.2 | 43.3±3.6 | 37.1±2.7* | 40.3±2.8 |
Values from Year 3 of the Health ABC study.
To convert nmol/L folate to ng/mL, multiply nmol/L by 0.441. To convert ng/mL folate to nmol/L, multiply ng/mL by 2.26. Folate of 83.9 nmol/L=37 ng/mL.
To convert pmol/L vitamin B-12 to pg/mL, multiply pmol/L by 1.355. To convert pg/mL vitamin B-12 to pmol/L, mulitpy pg/mL by 0.7378. Vitamin B-12 of 577.6 pmol/L=782.6 pg/mL.
Values from Year 2 of the Health ABC study.
To convert mg/dL vitamin C to μmol/L, multiply mg/dL by 56.78. To convert μmol/L vitamin C to mg/dL, multiply μmol/L by 0.0176. Vitamin C of 35.1 mg/dL=1,993 μmol/L.
To convert μmol/L beta carotene to μg/dL, multiply μmol/L by 53.76. To convert μg/dL beta carotene to μmol/L, multiply μg/dL by 0.0186. Beta carotene of 1.1 μmol/L=59.14 μg/dL.
To convert μmol/L vitamin E to mg/dL, multiply μmol/L by 0.043. To convert mg/dL vitamin E to μmol/L, multiply mg/dL by 23.22. Vitmain E of 50.7 μmol/L=2.18 mg/dL.
Significantly different from the Healthy Foods cluster at P≤0.05, based on Dunnett’s test for continuous variables and χ2 test for categorical variables.
In the all-cause mortality analysis, the mean follow-up time from baseline was 8.4 years, with a range of 1.1 to 10.4 years. During the follow-up period, 739 participants (29.5%) died. Table 4 displays the relative risk of mortality according to dietary pattern cluster. The Healthy Foods cluster had a significantly lower risk of mortality than the High-Fat Dairy Products cluster, the Meat, Fried Foods, and Alcohol cluster, and the Sweets and Desserts cluster, after controlling for sex, age, and race. After further adjustment for clinical site, education, physical activity, smoking and total energy intake, the High-Fat Dairy Products cluster (relative risk 1.40 [95% confidence interval 1.04, 1.88]) and the Sweets and Desserts cluster (relative risk 1.37 [95% confidence interval 1.02, 1.86]) still showed significantly higher risk of mortality than the Healthy Foods cluster. No significant differences in risk of mortality were seen between the Healthy Foods cluster and the Breakfast Cereal or Refined Grains clusters.
Table 4.
Relative risk (95% confidence interval) of all-cause mortality of Health, Aging, and Body Composition Study participants by dietary pattern cluster
| Healthy foods (n=374) | High-fat dairy products (n=332) | Meat, fried foods, and alcohol (n=693) | Breakfast cereal (n=386) | Refined grains (n=458) | Sweets and desserts (n=339) | |
|---|---|---|---|---|---|---|
| Number of deaths | 77 | 109 | 209 | 105 | 135 | 104 |
| % | 21.0 | 34.0 | 30.9 | 28.2 | 30.2 | 32.0 |
| relative risk (95% confidence interval) | ||||||
| Model 1a | 1.00 | 1.59 (1.19, 2.14)* | 1.39 (1.06, 1.82)* | 1.25 (0.93, 1.69) | 1.32 (0.99, 1.76) | 1.52 (1.13, 2.04)* |
| Model 2b | 1.00 | 1.40 (1.04, 1.88)* | 1.21 (0.92, 1.60) | 1.16 (0.86, 1.56) | 1.08 (0.80, 1.45) | 1.37 (1.02, 1.86)* |
Adjusted for sex, age, and race.
Adjusted for sex, age, race, clinical site, education, physical activity, smoking status, and total energy intake.
Significantly different from the Healthy Foods cluster at P≤0.05, based on Cox proportional hazards regression.
DISCUSSION
Dietary patterns were significantly associated with all-cause mortality in this study of older adults. The Healthy Foods cluster, with relatively higher intake of low-fat dairy products, fruit, whole grains, poultry, fish, and vegetables, and lower intake of meat, fried foods, sweets, high-energy drinks, and added fat, showed lower risk of mortality than both the High-Fat Dairy Products and Sweets and Desserts clusters after adjusting for relevant confounders. The High-Fat Dairy Products cluster had higher intake of foods such as ice cream, cheese, and 2% and whole milk and yogurt, and lower intake of poultry, low-fat dairy products, rice, and pasta, whereas the Sweets and Desserts cluster had relatively higher consumption of foods such as doughnuts, cake, cookies, pudding, chocolate, and candy, and lower intake of fruit, fish, other seafood, and dark green vegetables.
Results of this study confirm findings of previous studies that also found associations between dietary patterns and mortality (4,5,8,9,11,20–26). Several studies showed inverse relationships between a Mediterranean dietary pattern and all-cause and cardiovascular mortality (7,8,25), whereas multiple others showed inverse associations between a plant-based diet and all-cause and cardiovascular mortality (4,5,11,12,20,21,23,24,26). Bamia and colleagues (4) for example, linked increased adherence to a plant-based diet to lower all-cause mortality in adults aged 60 years and older in the European Prospective Investigation into Cancer and Nutrition-Elderly Study. Similarly, in a prospective study of adults in Denmark aged 30 to 70 years at baseline, Osler and colleagues (5) found inverse associations between a pattern high in wholemeal bread, vegetables, fruit, and fish and both all-cause and cardiovascular mortality. Also, in the Seven Countries Study, Menotti and colleagues (26) found a positive relationship between food patterns high in butter, dairy products, and other animal products and mortality due to coronary heart disease, and an inverse association between food patterns high in cereals, legumes, vegetables, fish, oils, and wine and coronary heart disease mortality.
Although culture influences dietary patterns, which are specific to each study population, patterns associated with mortality in this and previous studies have features in common. Virtually all studies linked a dietary pattern high in food groups such as vegetables, fruit, whole grains, poultry, fish, and low-fat dairy products to lower mortality compared to other dietary patterns. Multiple studies also related a dietary pattern high in plant foods to reduced risk of mortality. Unexpectedly, in this and several other studies, a pattern higher in red meat was not significantly associated with increased risk of mortality when controlled for relevant confounding factors. One suggested explanation is that plant-based diets may lower health risk because plant foods are protective, whereas diets high in animal foods may be more likely to increase risk only if the animal foods displace protective plant foods in the diet (5,25). In our study, the Meat, Fried Foods, and Alcohol clusters did have a slightly higher percentage of total energy from vegetables, fruit, and whole grains than both the High-Fat Dairy Products and Sweets and Desserts clusters, which showed higher risk of mortality.
In our study, the Healthy Foods cluster had more optimal levels of nutritional biomarkers than the other clusters, particularly the Refined Grains cluster. Older adults are at risk of inadequate vitamin B12 and folate status, which has been linked to increased levels of homocysteine (27). Elevated homocysteine has itself been related to poor cognitive function, dementia, Alzheimer’s disease, coronary heart disease, stroke, and mortality (28–32). Inadequate antioxidant status is also of concern to older adults, as it has been linked to risk of multiple chronic diseases (33–35). The more favorable nutritional status of those in the Healthy Foods cluster, who generally adhered to dietary guidelines, provides additional support for current guidelines.
Healthy People 2010 is a set of health objectives for people in the United States to achieve in the first decade of the 21st century. A primary goal of Healthy People 2010 is to increase quality and years of healthy life (36). In our study, those in the Healthy Foods cluster had significantly more years of healthy life than any other cluster. Similarly, in the US Cardiovascular Health Study of adults aged 65 years and older, a dietary pattern higher in fiber and total carbohydrate and lower in total fat was associated with more years of healthy life (21).
Strengths of this study include its thorough assessment of participants’ health status, relatively long 10-year follow-up period, and measurement of many potential confounding factors, unlike several previous studies that evaluated few confounders. A limitation of this study is that despite its relatively large sample size, the study population consisted of residents of two metropolitan areas, and therefore cannot be considered nationally representative. Also, participants may have changed their dietary patterns over the 10-year follow-up period, though changes in diet would most likely attenuate differences in health risk between the Healthy Foods and other clusters. Furthermore, as dietary patterns have been found to be part of specific lifestyles, it may be difficult by statistical methods to fully separate effects of diet from effects of physical activity and other lifestyle characteristics.
Results of this study suggest that older adults who follow a dietary pattern consistent with current guidelines to consume relatively high amounts of vegetables, fruit, whole grains, low-fat dairy products, poultry, and fish may have a lower risk of mortality. Because a substantial percentage of older adults in this study followed the Healthy Foods dietary pattern, adherence to such a diet appears a feasible and realistic recommendation for potentially improved survival and quality of life in the growing older adult population.
Acknowledgments
FUNDING/SUPPORT: The Health ABC Study was supported by National Institute on Aging contracts N01-AG-6-2101, N01-AG-6-2103, and N01-AG-6-2106. This research was supported in part by the Intramural Research Program of the National Institutes of Health, National Institute on Aging.
Footnotes
STATEMENT OF POTENTIAL CONFLICT OF INTEREST: No potential conflict of interest was reported by the authors.
Contributor Information
AMY L. ANDERSON, Department of Nutrition and Food Science, University of Maryland, College Park, MD.
TAMARA B. HARRIS, Geriatric Epidemiology Section, National Institute on Aging, Bethesda, MD.
FRANCES A. TYLAVSKY, Preventive Medicine, University of Tennessee Health Science Center, Memphis, TN.
SARA E. PERRY, School of Public Health and Tropical Medicine, Tulane University, New Orleans, LA.
DENISE K. HOUSTON, Sticht Center on Aging, Department of Internal Medicine, Wake Forest University School of Medicine, Winston-Salem, NC.
TRISHA F. HUE, Department of Epidemiology and Biostatistics, University of California, San Francisco.
ELSA S. STROTMEYER, Center for Aging and Population Health, Department of Epidemiology, Graduate School of Public Health, University of Pittsburgh, Pittsburgh, PA.
NADINE R. SAHYOUN, Department of Nutrition and Food Science, University of Maryland, College Park, MD.
References
- 1.Centers for Disease Control and Prevention. Public health and aging: Trends in aging—United States and worldwide. JAMA. 2003;289:1371–1373. [PubMed] [Google Scholar]
- 2.Gorina Y, Hoyert D, Lentzner H, Goulding M. Trends in causes of death among older persons in the United States. Aging Trends. 2005;6:1–12. [PubMed] [Google Scholar]
- 3.Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002;13:3–9. doi: 10.1097/00041433-200202000-00002. [DOI] [PubMed] [Google Scholar]
- 4.Bamia C, Trichopoulos D, Ferrari P, Overvad K, Bjerregaard L, Tjønneland A, Halkjaer J, Clavel-Chapelon F, Kesse E, Boutron-Ruault MC, Boffetta P, Nagel G, Linseisen J, Boeing H, Hoffmann K, Kasapa C, Orfanou A, Travezea C, Slimani N, Norat T, Palli D, Pala V, Panico S, Tumino R, Sacerdote C, Bueno-de-Mesquita HB, Waijers PM, Peeters PH, van der Schouw YT, Berenguer A, Martinez-Garcia C, Navarro C, Barricarte A, Dorronsoro M, Berglund G, Wirfält E, Johansson I, Johansson G, Bingham S, Khaw KT, Spencer EA, Key T, Riboli E, Trichopoulou A. Dietary patterns and survival of older Europeans: The EPIC-Elderly Study (European Prospective Investigation into Cancer and Nutrition) Public Health Nutr. 2007;10:590–598. doi: 10.1017/S1368980007382487. [DOI] [PubMed] [Google Scholar]
- 5.Osler M, Heitmann BL, Gerdes LU, Jorgensen LM, Schroll M. Dietary patterns and mortality in Danish men and women: A prospective observational study. Br J Nutr. 2001;85:219–225. doi: 10.1079/bjn2000240. [DOI] [PubMed] [Google Scholar]
- 6.Osler M, Schroll M. Diet and mortality in a cohort of elderly people in a north European community. Int J Epidemiol. 1997;26:155–159. doi: 10.1093/ije/26.1.155. [DOI] [PubMed] [Google Scholar]
- 7.Knoops KT, Groot de LC, Fidanza F, Alberti-Fidanza A, Kromhout D, van Staveren WA. Comparison of three different dietary scores in relation to 10-year mortality in elderly European subjects: The HALE project. Eur J Clin Nutr. 2006;60:746–755. doi: 10.1038/sj.ejcn.1602378. [DOI] [PubMed] [Google Scholar]
- 8.Knoops KT, de Groot LC, Kromhout D, Perrin AE, Moreiras-Varela O, Menotti A, van Staveren WA. Mediterranean diet, lifestyle factors, and 10-year mortality in elderly European men and women: The HALE project. JAMA. 2004;292:1433–1439. doi: 10.1001/jama.292.12.1433. [DOI] [PubMed] [Google Scholar]
- 9.Huijbregts P, Feskens E, Räsänen L, Fidanza F, Nissinen A, Menotti A, Kromhout D. Dietary pattern and 20 year mortality in elderly men in Finland, Italy, and The Netherlands: Longitudinal cohort study. BMJ. 1997;315:13–17. doi: 10.1136/bmj.315.7099.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lagiou P, Trichopoulos D, Sandin S, Lagiou A, Mucci L, Wolk A, Weiderpass E, Adami HO. Mediterranean dietary pattern and mortality among young women: A cohort study in Sweden. Br J Nutr. 2006;96:384–392. doi: 10.1079/bjn20061824. [DOI] [PubMed] [Google Scholar]
- 11.Kant AK, Schatzkin A, Graubard BI, Schairer C. A prospective study of diet quality and mortality in women. JAMA. 2000;283:2109–2115. doi: 10.1001/jama.283.16.2109. [DOI] [PubMed] [Google Scholar]
- 12.Kant AK, Graubard BI, Schatzkin A. Dietary patterns predict mortality in a national cohort: The National Health Interview Surveys, 1987 and 1992. J Nutr. 2004;134:1793–1799. doi: 10.1093/jn/134.7.1793. [DOI] [PubMed] [Google Scholar]
- 13.Seymour JD, Calle EE, Flagg EW, Coates RJ, Ford ES, Thun MJ American Cancer Society. Diet Quality Index as a predictor of short-term mortality in the American Cancer Society Cancer Prevention Study II nutrition cohort. Am J Epidemiol. 2003;157:980–988. doi: 10.1093/aje/kwg077. [DOI] [PubMed] [Google Scholar]
- 14.Kennedy ET, Ohls J, Carlson S, Fleming K. The Healthy Eating Index: Design and applications. J Am Diet Assoc. 1995;95:1103–1108. doi: 10.1016/S0002-8223(95)00300-2. [DOI] [PubMed] [Google Scholar]
- 15.Newby PK, Muller D, Hallfrisch J, Qiao N, Andres R, Tucker KL. Dietary patterns and changes in body mass index and waist circumference in adults. Am J Clin Nutr. 2003;77:1417–1425. doi: 10.1093/ajcn/77.6.1417. [DOI] [PubMed] [Google Scholar]
- 16.Tucker KL, Chen H, Hannan MT, Cupples LA, Wilson PW, Felson D, Kiel DP. Bone mineral density and dietary patterns in older adults: The Framingham Osteoporosis Study. Am J Clin Nutr. 2002;76:245–252. doi: 10.1093/ajcn/76.1.245. [DOI] [PubMed] [Google Scholar]
- 17.Operations manual. [Accessed June 17, 2008.];Health, Aging and Body Composition Study Web site. https://psg-mac43.ucsf.edu.
- 18.Refsum H, Smith AD. Low vitamin B-12 status in confirmed Alzheimer’s disease as revealed by serum holotranscobalamin. J Neurol Neurosurg Psychiatry. 2003;74:959–961. doi: 10.1136/jnnp.74.7.959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Taylor HL, Jacobs DR, Jr, Schucker B, Knudsen J, Leon AS, Debacker G. A questionnaire for the assessment of leisure time physical activities. J Chronic Dis. 1978;31:741–755. doi: 10.1016/0021-9681(78)90058-9. [DOI] [PubMed] [Google Scholar]
- 20.Hoffmann K, Boeing H, Boffetta P, Nagel G, Orfanos P, Ferrari P, Bamia C. Comparison of two statistical approaches to predict all-cause mortality by dietary patterns in German elderly subjects. Br J Nutr. 2005;93:709–716. doi: 10.1079/bjn20051399. [DOI] [PubMed] [Google Scholar]
- 21.Diehr P, Beresford SA. The relation of dietary patterns to future survival, health, and cardiovascular events in older adults. J Clin Epidemiol. 2003;56:1224–1235. doi: 10.1016/s0895-4356(03)00202-6. [DOI] [PubMed] [Google Scholar]
- 22.Trichopoulou A, Kouris-Blazos A, Wahlqvist ML, Gnardellis C, Lagiou P, Polychronopoulos E, Vassilakou T, Lipworth L, Trichopoulos D. Diet and overall survival in elderly people. BMJ. 1995;311:1457–1460. doi: 10.1136/bmj.311.7018.1457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Masala G, Ceroti M, Pala V, Krogh V, Vineis P, Sacerdote C, Saieva C, Salvini S, Sieri S, Berrino F, Panico S, Mattiello A, Tumino R, Giurdanella MC, Bamia C, Trichopoulou A, Riboli E, Palli D. A dietary pattern rich in olive oil and raw vegetables is associated with lower mortality in Italian elderly subjects. Br J Nutr. 2007;98:406–415. doi: 10.1017/S0007114507704981. [DOI] [PubMed] [Google Scholar]
- 24.Waijers PM, Ocké MC, van Rossum CT, Peeters PH, Bamia C, Chloptsios Y, van der Schouw YT, Slimani N, Bueno-de-Mesquita HB. Dietary patterns and survival in older Dutch women. Am J Clin Nutr. 2006;83:1170–1176. doi: 10.1093/ajcn/83.5.1170. [DOI] [PubMed] [Google Scholar]
- 25.Harriss LR, English DR, Powles J, Giles GG, Tonkin AM, Hodge AM, Brazionis L, O’Dea K. Dietary patterns and cardiovascular mortality in the Melbourne Collaborative Cohort Study. Am J Clin Nutr. 2007;86:221–229. doi: 10.1093/ajcn/86.1.221. [DOI] [PubMed] [Google Scholar]
- 26.Menotti A, Kromhout D, Blackburn H, Fidanza F, Buzina R, Nissinen A. Food intake patterns and 25-year mortality from coronary heart disease: Cross-cultural correlations in the Seven Countries Study. The Seven Countries Study Research Group. Eur J Epidemiol. 1999;15:507–515. doi: 10.1023/a:1007529206050. [DOI] [PubMed] [Google Scholar]
- 27.Clarke R, Refsum H, Birks J, Evans JG, Johnston C, Sherliker P, Ueland PM, Schneede J, McPartlin J, Nexo E, Scott JM. Screening for vitamin B-12 and folate deficiency in older persons. Am J Clin Nutr. 2003;77:1241–1247. doi: 10.1093/ajcn/77.5.1241. [DOI] [PubMed] [Google Scholar]
- 28.Prins ND, Den Heijer T, Hofman A, Koudstaal PJ, Jolles J, Clarke R, Breteler MM Rotterdam Scan Study. Homocysteine and cognitive function in the elderly. The Rotterdam Scan Study. Neurology. 2002;59:1375–1380. doi: 10.1212/01.wnl.0000032494.05619.93. [DOI] [PubMed] [Google Scholar]
- 29.Seshadri S, Beiser A, Selhub J, Jacques PF, Rosenberg IH, D’Agostino RB, Wilson PW, Wolf PA. Plasma homocysteine as a risk factor for dementia and Alzheimer’s disease. N Engl J Med. 2002;346:476–483. doi: 10.1056/NEJMoa011613. [DOI] [PubMed] [Google Scholar]
- 30.The Homocysteine Studies Collaboration. Homocysteine and risk of ischemic heart disease and stroke: A meta-analysis. JAMA. 2002;288:2015–2022. doi: 10.1001/jama.288.16.2015. [DOI] [PubMed] [Google Scholar]
- 31.Clarke R, Birks J, Nexo E, Ueland PM, Schneede J, Scott J, Molloy A, Evans JG. Low vitamin B-12 status and risk of cognitive decline in older adults. Am J Clin Nutr. 2007;86:1384–1391. doi: 10.1093/ajcn/86.5.1384. [DOI] [PubMed] [Google Scholar]
- 32.Dangour AD, Breeze E, Clarke R, Shetty PS, Uauy R, Fletcher AE. Plasma homocysteine, but not folate or vitamin B-12, predicts mortality in older people in the United Kingdom. J Nutr. 2008;138:1121–1128. doi: 10.1093/jn/138.6.1121. [DOI] [PubMed] [Google Scholar]
- 33.van’t Veer P, Jansen MC, Klerk M, Kok FJ. Fruits and vegetables in the prevention of cancer and cardiovascular disease. Public Health Nutr. 2000;3:103–107. doi: 10.1017/s1368980000000136. [DOI] [PubMed] [Google Scholar]
- 34.Lonn E, Bosch J, Yusuf S, Sheridan P, Pogue J, Arnold JM, Ross C, Arnold A, Sleight P, Probstfield J, Dagenais GR HOPE and HOPE-TOO Trial Investigators. Effects of long-term vitamin E supplementation on cardiovascular events and cancer: A randomized controlled trial. JAMA. 2005;293:1338–1347. doi: 10.1001/jama.293.11.1338. [DOI] [PubMed] [Google Scholar]
- 35.Gao X, Martin A, Lin H, Bermudez OI, Tucker KL. Alpha-Tocopherol intake and plasma concentration of Hispanic and non–Hispanic white elders is associated with dietary intake pattern. J Nutr. 2006;136:2574–2579. doi: 10.1093/jn/136.10.2574. [DOI] [PubMed] [Google Scholar]
- 36.Healthy people 2010. [Accessed September 11, 2008.];US Department of Health and Human Services Web site. http://www.healthypeople.gov/About/goals.htm.