Figure 1.
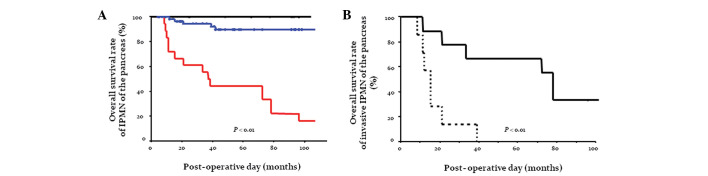
(A) Actuarial survival curves following resection of IPMN based on pathological type. Patients with an invasive IPMC had a significantly worse outcome compared with those with borderline or non-invasive IPMC. The rate of cumulative 5-year survival following curative resection of invasive adenocarcinoma derived from IPMN was 44.4% (median survival, 37.0 months). Overall survival rate of borderline IPMN of the pancreas (%) (blue line), non-invasive IPMC (black line) and invasive IPMC (red line). (B) Cumulative survival curves following resection of invasive adenocarcinoma derived from IPMN. Patients with an invasive adenocarcinoma derived from branch duct-type IPMN had a significantly worse outcome compared with those with invasive adenocarcinoma derived from main duct-type IPMN. The 5-year survival rates following curative resection of invasive adenocarcinoma were 0.0% (median survival, 15.0 months) for those tumors derived from branch duct-type IPMN and 66.7% (median survival, 78.0 months) for tumors derived from main duct-type IPMN. Overall survival rate of invasive IPMC derived from main duct-type IPMN of the pancreas (%) (solid line) and those derived from branch duct-type IPMN of the pancreas (broken line). IPMN, intraductal papillary mucinous neoplasm; IPMC, intraductal papillary mucinous carcinoma.
