Abstract
INTRODUCTION
Semiconstrained total elbow replacement is now a well recognised and reliable surgical option for advanced elbow disease, mainly rheumatoid arthritis.
METHODS
We report a retrospective analysis of 31 primary total elbow replacements in 28 patients with a mean follow-up duration of 55 months. The mean age of the patients was 65 years. The indications included 27 cases of rheumatoid arthritis, 3 fractures and 1 case of osteoarthritis. Twenty-one elbows in nineteen patients were assessed using the Mayo elbow performance score (MEPS) in a special follow-up clinic. In the other nine patients (ten elbows), the assessment was carried out with case notes and x-rays.
RESULTS
The mean pre-operative MEPS in the 21 elbows recalled was 40. This improved to 89 post-operatively (range: 55-100). Sixteen of the twenty-one elbows were considered excellent, two good, two fair and one poor. The range of movement was recorded in eight of the other ten elbows and the mean was 98°. At the last follow-up visit, x-rays were normal in 23 elbows although the ulnar component was loose in 3, the humeral component loose in 2. There were also two cases of nonunion of the medial epicondyle and one patient had mild heterotopic ossification. Complications included one infection, which needed irrigation and debridement with a satisfactory final result, and two cases of ulnar nerve palsy/neurapraxia. Two elbows were considered failures due to severe pain caused by prosthetic loosening. These were referred for revision surgery.
CONCLUSIONS
Excellent pain relief and good function can be achieved in the medium and long term with the Coonrad-Morrey semiconstrained total elbow replacement prosthesis in patients with severe destructive elbow arthropathy.
Keywords: Elbow, Arthroplasty, Coonrad-Morrey, Loosening
In the past four decades total elbow replacement (TER) has emerged as a viable surgical option for advanced elbow disease.1 Improvements and modifications in implant designs based on an increased understanding of the biomechanics of the elbow joint (which is less well understood than hip and knee joints) have led to increasingly good clinical outcomes after elbow replacement. Earlier procedures like the in-terpositional arthroplasty and synovectomy provided some pain relief. In 1972 Dee introduced the first ‘modern’ constrained total elbow prosthesis using cement. Despite good initial clinical outcomes, loosening rates were extremely high due to high stress levels at the bone-cement interface. Non-constrained (resurfacing) and semiconstrained pros-theses were then developed to overcome the problem.
The original 1973 design of the Coonrad prosthesis was modified in 1978 to incorporate longer stems and also more laxity in the varus/valgus plane, thereby reducing the incidence of loosening. In 1981 the anterior flange was introduced to resist displacement forces for posterior dislocation and this Coonrad-Morrey prosthesis further reduced the incidence of loosening.2
So far, the heterogeneity of studies published, the use of more than one prosthesis in one study and inconsistency in clinical scoring criteria have led to difficulty in assessing long-term results of the Coonrad-Morrey prosthesis. However, in the last ten years many studies have been published with satisfactory results and survival analysis of this semiconstrained prosthesis.3–6 The aim of our study was to investigate the results of all the Coonrad-Morrey prostheses used in primary TERs at our institution.
Methods
A series of consecutive TERs performed at one institution was reviewed retrospectively. All operations were performed by the senior author. Antibiotic prophylaxis was given prior to the operation. A pneumatic tourniquet was used. A posterior Mayo triceps sparing approach was used, gently retracting and protecting the ulnar nerve. Bone cuts were made using the jigs, and the humeral and ulnar canals were prepared. The components were cemented using low viscosity Palacos® bone cement (Heraeus, Wehrheim, Germany) after a satisfactory trial reduction. A small bone graft was then placed between the flange and the humeral shaft. Post-operatively, the elbows were immobilised in extension for 48 hours before commencing flexion exercises.
Overall, 28 patients (31 elbows) had undergone Coon-rad-Morrey TERs (Table 1). With the approval of our institution's ethical committee, we were able to recall 19 patients (21 elbows) for clinical and radiological review in a special clinic. Assessment was made using the Mayo elbow performance score (MEPS). The remaining patients were either dead (seven patients, eight elbows) or could not be contacted (two patients, two elbows). In these patients, assessment was made using the case records and x-rays.
Table 1.
Details of all 28 patients (31 total elbow replacements)
| Elbow number | Age | Sex | Side | Diagnosis | Follow-up duration | MEPS | X-ray | Comment or complications |
| 1 | 56 | M | R | RA | 88 months | 75 | Loose ulnar component | Ulnar nerve palsy |
| 2 | 58 | F | L | OA | 33 months | 70 Loose ulnar component | Loose hinge | |
| 3 | 62 | M | R | RA | 78 months | 65 | Good | - |
| 4 | 68 | M | L | RA | 34 months | 55 | Loose humeral component | - |
| 5 | 67 | M | R | RA | 43 months | 100 | Good | - |
| 6 | 65 | M | L | RA | 6 months | 90 | Good | - |
| 7 | 61 | M | R | RA | 53 months | 90 | Loose ulnar component | - |
| 8 | 63 | M | R | RA | 103 months | 100 | Good | - |
| 9 | 68 | F | R | RA | 101 months | 100 | Good | - |
| 10 | 69 | F | L | NU# | 96 months | 90 | Good | - |
| 11 | 61 | F | L | RA | 84 months | 95 | Good | - |
| 12 | 65 | F | R | RA | 85 months | 100 | Good | - |
| 13 | 63 | F | R | RA | 83 months | 85 | Good | - |
| 14 | 68 | F | R | RA | 124 months | 100 | Satisfactory, mild heterotopic ossification | - |
| 15 | 57 | F | L | RA | 106 months | 100 | Good | Infection, wash out |
| 16 | 53 | M | R | RA | 38 months | 90 | Loose humeral component | - |
| 17 | 60 | F | R | RA | 42 months | 100 | NU of the medial epicondyle | - |
| 18 | 57 | F | L | RA | 61 months | 95 | Good | - |
| 19 | 65 | F | R | RA | 72 months | N/A | Loose* | Referred for revision |
| 20 | 80 | F | L | # | 30 months | N/A | Loose* | Referred for revision |
| 21 | 67 | M | R | RA | 36 months | N/A | Goord* | - |
| 22 | 59 | M | R | RA | 39 months | N/A | Good* | - |
| 23 | 58 | M | L | RA | 55 months | N/A | Good* | - |
| 24 | 73 | F | R | RA | 7 months | N/A | Good* | - |
| 25 | 70 | F | R | RA | 16 months | N/A | Good* | - |
| 26 | 67 | F | L | RA | 5 months | N/A | Good* | - |
| 27 | 61 | M | L | RA | 30 months | N/A | Good* | - |
| 28 | 83 | F | L | RA | 3 months | N/A | Good* | - |
| 29 | 76 | F | R | # | 12 months | 100 | Good | - |
| 30 | 63 | F | R | RA | 120 months | 100 | Good | - |
| 31 | 60 | F | R | RA | 5 months | 100 | Good | Ulnar neurapraxia |
MEPS = Mayo elbow performance score; RA = rheumatoid arthritis; OA = osteoarthritis; NU = non-union; # = fracture
deceased
unable to contact
The mean follow-up duration was 55 months (range: 3-124 months). The mean age at operation was 65 years (range: 53-83 years). Of the 28 patients, 19 were in women and 19 had surgery on the right and 9 on the left elbow. There were 3 bilateral procedures (sequential). The indications for surgery were rheumatoid arthritis in 27 cases, complex elbow fractures in 2 cases, non-union of fracture in 1 case and primary osteoarthritis in 1 case.
Results
Complications included one deep infection, requiring irrigation and debridement. This had a satisfactory final result with a MEPS of 100 at the eight-year assessment. Ulnar nerve palsy occurred in two patients. (This was permanent in one with no recovery. The other patient had neuraprax-ia with partial recovery but some residual sensory disturbance.)
The mean pre-operative MEPS for the 21 elbows for patients recalled was 40. The mean post-operative score in these patients was 89 (range: 55-100): 16 patients scored 90 or more (excellent), two scored 75-89 (good), two scored 60-74 (fair) and one scored 55 (poor).
The ten elbows assessed by case notes and x-rays alone had a mean range of movement arc of 98° at their last follow-up appointment. X-rays were available for all ten elbows. Eight had no evidence of loosening. When last seen, six elbows had no pain while one had mild pain, one moderate pain and two severe pain. The two elbows with persistent severe pain were found to have loosening of the implant and were referred for revision at six and three years post-operatively. One of these two elbows had undergone TER for trauma.
Of the 31 procedures, therefore, 3 (9.7%) were considered failures at 30, 34 and 72 months. The endpoint was the revision surgery in two elbows and the poor MEPS assessment in one elbow. The survival rate at 124 months was 90.6% (Fig 1).
Figure 1.
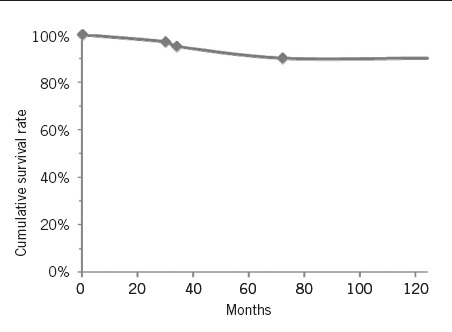
Survivorship analysis curve of the 31 elbows
X-ray assessment in the group as a whole showed no abnormality in 23 elbows. No specific criteria were used for radiographic analysis but radiolucent lines and region of lucency were noted. Progression of the lucent lines was also recorded. Three had a loose ulnar component (one of which also had a loose hinge), two had loose humeral components, one had a non-union of the medial epicondyle and one had mild heterotopic ossification. One of the patients who had a loose ulnar component at 5 years scored 90 on the MEPS assessment and had a bilateral TER with no radiological evidence of loosening on the other side at 18 months (Figs 2,3).
Figure 2.

X-rays of left elbow from one of the patients with bilateral total elbow replacements at 18 months after surgery. (See Fig 3 for x-rays of patient's right elbow.)
Figure 3.
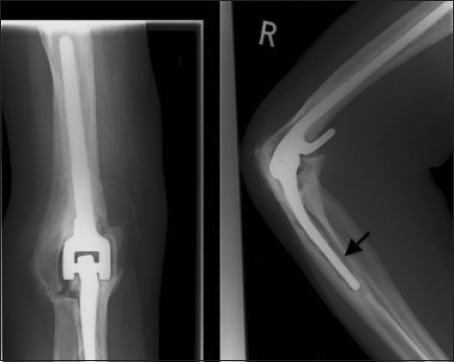
Figure 3 X-rays of right elbow from one of the patients with bilateral total elbow replacements at five years after surgery. Note loosening of the ulnar prosthesis (arrow). However, functionally the patient scored 90 on the Mayo elbow performance score. (See Fig 2 for x-rays of patient's left elbow.)
Discussion
The majority of TERs are performed for severe pain and disability in patients with advanced destructive elbow arthropathy due to rheumatoid arthritis. The Coonrad-Morrey semiconstrained prosthesis has provided good results in terms of significant improvement in function and excellent pain relief. Müller et al have published satisfactory results of primary TERs with a Coonrad-Morrey prosthesis in patients with distal humerus fractures.7
Gill and Morrey reported prosthesis survival at 10 years as 92%, with 86% having good or excellent results in 78 elbows with the Coonrad-Morrey prosthesis.4 Shi et al reported a post-operative mean MEPS of 84 for primary implants.8 In a long-term study by Aldredge et al with a follow-up duration of 10-31 years, the mean MEPS for the Coonrad-Morrey prosthesis was 91 in 41 elbows.3 In our series, we considered 3 elbows as failures and the overall survival rate at 124 months was 90.6%.
The inconsistency of post-operative assessment tools in the past has been overcome with the MEPS system. We feel that this is a reliable patient-based assessment tool for functional outcome measurement and it has been used widely in recently published studies. The SF-36® (Short Form 36) and DASH (Disabilities of the Arm, Shoulder and Hand) questionnaires have also been used in other studies5 but we consider the MEPS assessment to be more specific to elbow disease.
Ulnar nerve palsy is a well recognised complication of TER and the reported incidence varies from 1.7% to 28%.1 Transient median nerve palsy has also been reported7 but was not observed in our series. The exposure of ulnar nerve and transposition during TER is controversial.1,9 We perform TER with a triceps sparing approach and had 2 ulnar nerve palsies in 31 elbows.
Aseptic loosening and osteolysis is a concern a few years after TER but we found that this does not necessarily result in significant symptoms as most of these patients are low demand (with advanced rheumatoid disease) and do not always proceed to severe loosening or dislocation.10,11
Conclusions
TERs are performed much less often than hip and knee replacements, and they are less predictable in that there is a significantly greater risk of complications. It is important to counsel patients pre-operatively to obtain properly informed consent.
Nevertheless, our experience with the Coonrad-Morrey semiconstrained prostheses has been satisfactory and comparable with results published elsewhere. The clinical and radiological results do not appear to have deteriorated over the period of this study. With progressive understanding of elbow biomechanics, improvements in implant design and surgical techniques of the procedure, the results may improve further.
References
- 1.Hargreaves D, Emery R. Total elbow replacement in the treatment of rheumatoid disease. Clin Orthop Relat Res. 1999;366:61–71. doi: 10.1097/00003086-199909000-00009. [DOI] [PubMed] [Google Scholar]
- 2.van der Lugt JC, Rozing PM. Systematic review of primary total elbow prostheses used for the rheumatoid elbow. Clin Rheumatol. 2004;23:291–298. doi: 10.1007/s10067-004-0884-9. [DOI] [PubMed] [Google Scholar]
- 3.Aldridge JM, Lightdale NR, Mallon WJ, Coonrad RW. Total elbow arthroplasty with the Coonrad/Coonrad-Morrey prosthesis. A 10- to 31-year survival analysis. J Bone Joint Surg Br. 2006;88:509–514. doi: 10.1302/0301-620X.88B4.17095. [DOI] [PubMed] [Google Scholar]
- 4.Gill DR, Morrey BF. The Coonrad-Morrey total elbow arthroplasty in patients who have rheumatoid arthritis. A ten to fifteen-year follow-up study. J Bone Joint Surg Am. 1998;80:1,327–1,335. doi: 10.2106/00004623-199809000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Hildebrand KA, Patterson SD, Regan WD, et al. Functional outcome of semiconstrained total elbow arthroplasty. J Bone Joint Surg Am. 2000;82:1,379–1,386. doi: 10.2106/00004623-200010000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Schneeberger AG, Meyer DC, Yian EH. Coonrad-Morrey total elbow replacement for primary and revision surgery: a 2- to 7.5-year follow-up study. J Shoulder Elbow Surg. 2007;16:S47–S54. doi: 10.1016/j.jse.2006.01.013. [DOI] [PubMed] [Google Scholar]
- 7.Muller LP, Kamineni S, Rommens PM, Morrey BF. Primary total elbow replacement for fractures of the distal humerus. Oper Orthop Traumatol. 2005;17:119–142. doi: 10.1007/s00064-005-1125-3. [DOI] [PubMed] [Google Scholar]
- 8.Shi LL, Zurakowski D, Jones DG, et al. Semiconstrained primary and revision total elbow arthroplasty with use of the Coonrad-Morrey prosthesis. J Bone Joint Surg Am. 2007;89:1,467–1,475. doi: 10.2106/JBJS.F.00715. [DOI] [PubMed] [Google Scholar]
- 9.Szekeres M, King GJ. Total elbow arthroplasty. J Hand Ther. 2006;19:245–253. doi: 10.1197/j.jht.2006.02.010. [DOI] [PubMed] [Google Scholar]
- 10.Little CP, Graham AJ, Karatzas G, et al. Outcomes of total elbow arthroplasty for rheumatoid arthritis: comparative study of three implants. J Bone Joint Surg Am. 2005;87:2,439–2,448. doi: 10.2106/JBJS.D.02927. [DOI] [PubMed] [Google Scholar]
- 11.Morrey BF, Adams RA. Semiconstrained arthroplasty for the treatment of rheumatoid arthritis of the elbow. J Bone Joint Surg Am. 1992;74:479–490. [PubMed] [Google Scholar]


