Figure 2.
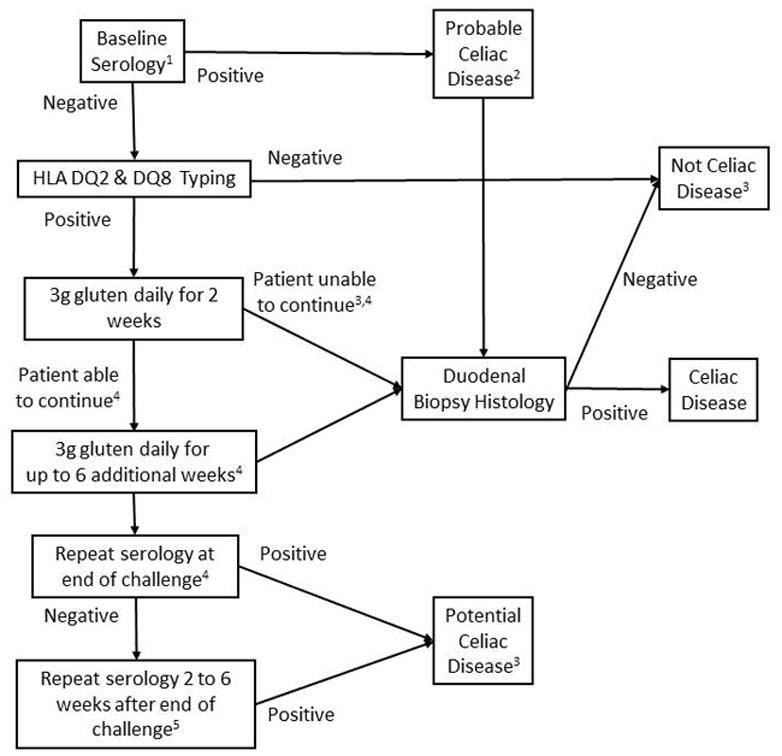
An approach to gluten challenge for the diagnosis or exclusion of CD in patients maintained on a gluten free diet without prior definitive diagnostic testing. [Adapted from reference Leffler D, Gut 2012]
1. Tissue transglutaminase, endomysium and/or deamidated gliadin peptide antibody serology.
2. Normal or non-diagnostic histology in a patient with positive serology while maintaining a GFD requires gluten challenge and repeat biopsy for definitive diagnosis or exclusion of CD.
3. Those with positive celiac serology but a normal biopsy have potential CD and should be evaluated and monitored further depending upon their clinical circumstances
4. In one study of subjects receiving a gluten challenge for 14 days Marsh III histology was seen in 68%, positive celiac serology in 75% and either Marsh III histology or positive serology in 90%. Thus, a 2 week gluten challenge may yield false negative results in 10% of patients. The added diagnostic sensitivity of extending the challenge to 8 weeks is unknown.
5. Celiac serology antibody concentrations may continue to rise after a gluten challenge ends. In one study positive tTG serology was seen in 25% of subjects and positive DGP serology in 30% at the end of a 14 day gluten challenge; 50% had at least one positive serology on day 14. Positivity rates rose to 55% and 45% respectively 14 days later, despite the fact that subjects had resumed a GFD; 75% had at least one positive serology on day 28, 14 days after the gluten challenge ended.
