Abstract
This report updates surveillance results for COPD in the United States. For 1999 to 2011, data from national data systems for adults aged ≥ 25 years were analyzed. In 2011, 6.5% of adults (approximately 13.7 million) reported having been diagnosed with COPD. From 1999 to 2011, the overall age-adjusted prevalence of having been diagnosed with COPD declined (P = .019). In 2010, there were 10.3 million (494.8 per 10,000) physician office visits, 1.5 million (72.0 per 10,000) ED visits, and 699,000 (32.2 per 10,000) hospital discharges for COPD. From 1999 to 2010, no significant overall trends were noted for physician office visits and ED visits; however, the age-adjusted hospital discharge rate for COPD declined significantly (P = .001). In 2010 there were 312,654 (11.2 per 1,000) Medicare hospital discharge claims submitted for COPD. Medicare claims (1999-2010) declined overall (P = .045), among men (P = .022) and among enrollees aged 65 to 74 years (P = .033). There were 133,575 deaths (63.1 per 100,000) from COPD in 2010. The overall age-adjusted death rate for COPD did not change during 1999 to 2010 (P = .163). Death rates (1999-2010) increased among adults aged 45 to 54 years (P < .001) and among American Indian/Alaska Natives (P = .008) but declined among those aged 55 to 64 years (P = .002) and 65 to 74 years (P < .001), Hispanics (P = .038), Asian/Pacific Islanders (P < .001), and men (P = .001). Geographic clustering of prevalence, Medicare hospitalizations, and deaths were observed. Declines in the age-adjusted prevalence, death rate in men, and hospitalizations for COPD since 1999 suggest progress in the prevention of COPD in the United States.
COPD is a serious public health problem in the United States. In 2008, chronic lower respiratory diseases, of which COPD represents the principal component, became the third leading cause of mortality.1 Because smoking is the dominant risk factor for COPD and contributed to about 80% of COPD deaths in 2000 to 2004,2 much of this disease is potentially preventable. People with COPD experience worse health-related quality of life, more disabilities, and higher rates of comorbidities than people without COPD.3‐5 The direct economic cost attributable to COPD and asthma in 2008 has been estimated at $53.7 billion in the United States.6 These costs include those for prescription medicines ($20.4 billion), outpatient or office-based providers ($13.2 billion), hospital inpatient stays ($13.1 billion), home health care ($4.0 billion), and ED visits ($3.1 billion).
COPD consists of chronic bronchitis, emphysema, and small airways disease. This common lung disease is characterized by inflammation and thickening of the mucosae of the airways, weakening or destruction of alveolar walls, and excess mucus production. These mechanical and physiologic changes lead to airflow limitation with limited reversibility. Patients affected by this disorder may be asymptomatic or experience cough, dyspnea, wheezing, and chest tightness. With progression of the disease, dyspnea worsens and oxygenation impairment develops. As the capacity of the lung continues to decline, patients may have increasing difficulty in performing activities of daily living. Although the clinical course of COPD is variable, it is progressive in many patients. Increasingly, research is examining the relationships between COPD and comorbid disease.7,8
The condition has a diverse etiology.4,9 Although smoking is the chief cause of COPD in most populations, substantial proportions of COPD occur among nonsmokers.10‐12 Other important causes include indoor air pollution from burning of biomass, occupational exposures to a variety of dusts and smoke, asthma, and repeated respiratory infections. In addition, genetic causes, such as α1-antitrypsin deficiency, can result in emphysema.
In 2002, the Centers for Disease Control and Prevention (CDC) released the initial surveillance report about COPD that contained surveillance data through the year 2000.13 This report summarized data from national data systems regarding prevalence, physician outpatient visits, ED visits, hospitalizations, and mortality. Of note was that the age-adjusted mortality rate had increased from 1980 to 2000, especially in women. The current surveillance report seeks to characterize recent aspects of the burden of COPD by providing additional information from national datasets through 2011.
Materials and Methods
The following data sources were used to produce the estimates in this report: Behavioral Risk Factor Surveillance System (BRFSS) (2011), National Health Interview Survey (NHIS) (1999-2011), National Ambulatory Medical Care Survey (NAMCS) (1999-2010), National Hospital Ambulatory Medical Care Survey (NHAMCS) (1999-2010), National Hospital Discharge Survey (NHDS) (1999-2010), death certificate data from the National Vital Statistics System (NVSS) (1999-2010), and Medicare Part A hospital claims administrative data (1999-2010). We did not include data from the National Health and Nutrition Examination Survey in this report because data from NHIS has commonly been used to provide national estimates of the prevalence of COPD. Furthermore, prevalence estimates of obstructive impairment using recent National Health and Nutrition Examination Survey data have been published.14 Except for Medicare hospital claims, the data presented in this report are limited to adults aged ≥ 25 years, to remain consistent with the prior surveillance report. Because all the data that were used in the analyses are freely available in the public domain, our study was exempt from human subject review.
Behavioral Risk Factor Surveillance System
BRFSS data from 2011 were used to estimate the state specific and US prevalence of COPD. An annual sample representing the noninstitutionalized US adult population aged ≥ 18 years in each state was selected by state health departments in collaboration with the CDC using a complex multistage sampling design.15 Data from 475,616 respondents aged ≥ 25 years were analyzed for this report. The BRFSS is a random-digit-dialed telephone survey of landline and cellphone households, and one adult is selected for the telephone interview. The median survey response rate in 2011 for all states and the District of Columbia was 49.7% and ranged from 33.8% to 64.1%. The median cooperation rate (percentage of people who completed interviews among all eligible contacted people) was 74.2% and ranged from 52.7% to 84.3%. The following question was used to define COPD: “Have you ever been told by a doctor or other health professional that you have chronic obstructive pulmonary disease (COPD), emphysema, or bronchitis?” An affirmative response was defined as physician-diagnosed COPD. Demographic information was self-reported.
National Health Interview Survey
NHIS data from 1999 to 2011 were used to estimate the prevalence of COPD.16 The NHIS is implemented annually by the National Center for Health Statistics, CDC. During each year, a sample representing the civilian, noninstitutionalized US population aged ≥ 18 years was selected by using a complex multistage sampling design that involves stratification, clustering, and oversampling. The universe of primary sampling units (PSUs) (single counties or groups of adjacent counties—or equivalent jurisdictions—or metropolitan area) is organized into strata from which a sample of PSUs representing areas is drawn. From substrata (census blocks or combined blocks) created in these selected PSUs, secondary sampling units are systematically selected. From each substratum, households with African American, Hispanic, and Asian (since 2006) were oversampled, and a sample of all other households was selected. Only one randomly selected adult per family was asked to participate in the Sample Adult questionnaire. Participants were visited in their homes, where US Census Bureau interviewers conducted a computer-assisted personal interview with the participants. The number of adult participants and the response rates of the surveys are summarized in e-Table 1 (647.6KB, pdf) . Data from adult respondents aged ≥ 25 years were analyzed for this report. The following two questions were used to define COPD: “Have you ever been told by a doctor or other health professional that you had emphysema?” and “During the past 12 months, have you been told by a doctor or other health professional that you had chronic bronchitis?” An affirmative response to one or both of these questions was defined as physician-diagnosed COPD for this report. Demographic information was self-reported.
National Ambulatory Medical Care Survey
NAMCS data from 1999 to 2010 were used to estimate the annual number of physician office visits with the first-listed diagnosis of COPD.17 The NAMCS is an annual, national probability sample survey of ambulatory visits to nonfederally employed office-based physicians conducted by the National Center for Health Statistics, CDC. Beginning in 2006, visits to Community Health Centers (CHCs) were also included. NAMCS used a multistage design that involved probability samples of PSUs, physicians within PSUs, and patient visits within practices. The first-stage sample included 112 PSUs. In each sample PSU, a probability sample of practicing nonfederal office-based physicians was selected from master files maintained by the American Medical Association and American Osteopathic Association. The final stage involved systematic random samples of office visits during randomly assigned 7-day reporting periods. Starting in 2006, a dual-sampling procedure was used to select CHC physicians and other providers. First, the traditional NAMCS sample was selected using the methods described previously. Second, information from the Health Resources and Services Administration and the Indian Health Service was used to select a sample of CHCs. Within CHCs, a maximum of three health-care providers were selected, including physicians, physician assistants, nurse practitioners, or nurse midwives. After selection, CHC providers followed traditional NAMCS methods for selecting patient visits. The physician-patient encounter or visit represents the basic sampling unit in NAMCS.
Data are collected by the physician or the physician’s staff or by US Census Bureau field representatives. Information concerning race and ethnicity was based on the physician’s knowledge of the patient or on the physician’s or assistant’s judgment rather than the patient self-report. The number of physician office visits and the physicians’ response rates are shown in e-Table 2 (647.6KB, pdf) . Because the percent of office visit medical records that were missing race information ranged from 16.9% to 32.8% (e-Table 2 (647.6KB, pdf) ), we used information for race (whites and blacks only) that was imputed by the National Center for Health Statistics.
Three visit diagnosis fields were available to participating physicians. A diagnosis of COPD was established from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes 490 (bronchitis not specified as acute or chronic), 491 (chronic bronchitis), 492 (emphysema), or 496 (chronic airway obstruction, not elsewhere classified, which includes COPD) for the first-listed diagnosis. Rates for office visits were calculated using US civilian population estimates provided in the data file documentation for each year (e-Table 3 (647.6KB, pdf) ). SEs were produced with statistical software.
National Hospital Ambulatory Medical Care Survey
NHAMCS data for the years 1999 to 2010 were used to estimate the number of ED visits for COPD.17 The NHAMCS is an annual, national probability sample survey of ambulatory visits made to nonfederal, general, short-stay hospitals in the US conducted by the National Center for Health Statistics, CDC. NHAMCS uses a multistage probability design with samples of PSUs, hospitals within PSUs, EDs plus clinics within outpatient departments, and patient visits within EDs and outpatient clinics. Sample hospitals are randomly assigned to 16 panels that rotate across 13 4-week reporting periods throughout the year. The initial sample frame of hospitals was based on the 1991 SMG hospital database now maintained by IMS Health Incorporated. Hospital staff or US Census Bureau field representatives performed data collection for NHAMCS. The annual number of patient record forms submitted by EDs is shown in e-Table 4 (647.6KB, pdf) .
The NHAMCS files contained three visit diagnosis fields. An ICD-9-CM code of 490-492 or 496 for the first-listed diagnosis was defined as an ED visit for COPD. Because the percentage of ED records that were missing race information ranged from 10.4% to 15.3% (e-Table 4 (647.6KB, pdf) ), we used information for race (whites and blacks only) that was imputed by the National Center for Health Statistics. The US civilian population estimates that we used to calculate rates of ED visits were obtained from the data file documentation for each year (e-Table 3 (647.6KB, pdf) ). SEs were produced with statistical software.
National Hospital Discharge Survey
NHDS data from 1999 to 2010 were used to estimate the annual number of hospital discharges for COPD.18 NHDS is an annual survey of inpatient discharges from nonfederal, short-stay hospitals in the US conducted from 1965 to 2010 by the National Center for Health Statistics, CDC. Using the SMG Hospital Market Data File or its successors as the sampling frame, the NHDS samples inpatient discharges from nonfederal, general, short-stay hospitals located in the 50 states and the District of Columbia. A three-stage design has been used since 1988. Units selected at the first stage of sampling consisted of either hospitals or geographic areas, such as counties, groups of counties, or metropolitan statistical areas in the 50 states and the District of Columbia. Within sampled geographic areas, additional hospitals were selected. Finally, at the last stage, discharges were selected within the sampled hospitals using systematic random sampling. Data collection was performed with manual and automated systems. The annual number of sampled records and hospital response rates are provided in e-Table 5 (647.6KB, pdf) .
Using the first-listed diagnosis, hospital discharges for COPD were identified by using the ICD-9-CM codes 490-492 or 496 as the first-listed diagnosis or ICD-9-CM code 466-466.1 (acute bronchitis) if the first-listed diagnosis of acute bronchitis was accompanied by another listed diagnosis of COPD (490-492 or 496). The percent of hospital records missing race information ranged from 16.0% to 31.0% (e-Table 5 (647.6KB, pdf) ). US civilian population estimates used to calculate hospital discharge rates were obtained from the NHDS data documentation (e-Table 6 (647.6KB, pdf) ). Relative SEs were calculated from the following formula: RSE(X) = (a + b/X)1/2, where a and b represent coefficients provided in the data documentation, and X represents the number of discharges.
Medicare Part A Hospital Claims
Medicare data from 1999 to 2010 were used to estimate the annual number of hospital discharges for COPD among Medicare enrollees aged ≥ 65 years. Hospitalization information from 100% of Medicare Part A hospital claims data were obtained from an administrative claims dataset maintained by the Centers for Medicare and Medicaid Services. Information was limited to approximately 10 million annual claims submitted for short-term fee-for-service hospital stays among Medicare enrollees aged ≥ 65 years residing in one of the 50 states or the District of Columbia in a given year. A hospital discharge for COPD was defined for a first-listed discharge diagnosis with ICD-9-CM codes 490-492 or 496—about 3% of annual Medicare claims. Few Medicare claims (< 0.05%) were submitted for acute bronchitis (ICD-9-CM code 466-466.1) with concomitant COPD; therefore, we did not include these discharges in our analyses. Race/ethnicity information on the claims data for Medicare enrollees represents information provided by most Medicare enrollees at the time of enrollment into the Medicare system or is information updated for older enrollees. Less than 0.5% of COPD claims were missing race information. State of residence was also obtained from the claims data. Medicare enrollment records were obtained from the Centers for Medicare and Medicaid Services and were used as the denominator file to calculate hospital rates after restricting the denominator to Medicare enrollees who met all the following criteria on July 1 of any given year (alive, aged ≥ 65 years, entitled to Part A benefits, residing in one of the 50 states or the District of Columbia, and not enrolled in a managed care plan).
National Vital Statistics System
The number of deaths with COPD as the underlying cause for the years 1999 to 2010 come from the NVSS and are made available from CDC’s WONDER system (Compressed Mortality File).19 This interactive Web-based tool allows queries to obtain numbers of death for underlying causes, crude death rates, age-adjusted death rates, 95% CIs, and SEs for groups defined by various characteristics including year, place of residence (state, county, region, or division), sex, age group, race, and Hispanic origin.20 Data from the NVSS are based on information from all resident death certificates filed in the 50 States and the District of Columbia. Cause-of-death statistics presented in this report are classified in accordance with the International Classification of Diseases, Tenth Revision (ICD-10). ICD-10 codes J40-J44 were used to identify deaths from COPD as the underlying cause of death. These causes include chronic bronchitis (J40-J42), emphysema (J43), and other COPD (J44).
Mortality rates were calculated by using population estimates produced by the Bureau of the Census in collaboration with the National Center for Health Statistics.20 The 1999 population estimates are US Census Bureau bridged-race intercensal estimates of the July 1 resident population, based on the 1990 census and the bridged-race 2000 census. The 2000 and 2010 population estimates are April 1 modified 2000 and 2010 census counts with bridged-race categories, whereas the 2001 to 2009 population estimates are bridged-race intercensal estimates of July 1 resident populations, based on the year 2000 and the year 2010 census counts (released by CDC on October 26, 2012). Age-adjusted death rates for 2001 to 2009 may vary from previous reports because of the 2012 revision of the 2001 to 2009 population denominator estimates.
Data Analysis
SAS-callable SUDAAN (Research Triangle Institute) was used to obtain weighted US estimates and prevalence from NHIS and state-specific and US estimates and prevalence from BRFSS. SAS or SAS-callable SUDAAN analyses for data from NAMCS, NHAMCS, and NHDS were weighted to obtain national US estimates. SAS was also used to obtain the number of COPD hospital discharges from Medicare hospital claims. The reported numbers of deaths, age-specific death rates, and age-adjusted death rates from COPD were obtained from CDC WONDER.19 Estimates were produced for all adults aged ≥ 25 years as well as for groups defined by age (25-44, 45-54, 55-64, 65-74, and ≥ 75 years), sex, and race/ethnicity. Racial/ethnic categories varied between surveillance systems because of differences in Medicare definitions of race/ethnicity categories; absence of racial/ethnic information on many medical records abstracted for NAMCS, NHAMCS, and NHDS; or small numbers of NHIS respondents in some racial/ethnic categories in the population samples selected. Except for Medicare estimates, age-adjusted estimates were standardized to the 2000 standard US population aged ≥ 25 years using the direct method.21 Medicare estimates were age-standardized to the 2000 standard US population aged ≥ 65 years. Because of the well-known relationship between age and COPD and because of the aging of the US population, we calculated age-adjusted estimates of prevalence and rates. State-specific age-adjusted estimates for BRFSS prevalence, Medicare hospitalizations, and mortality for COPD were also obtained to examine geographic clustering of COPD burden.
The statistical significance of temporal trends for age-specific prevalence of COPD in NHIS was examined by using log-linear regression analysis with time as the independent variable; analyses for trends in the age-adjusted prevalence included age as a continuous variable. The statistical significance for linear trends in age-specific and age-adjusted rates of physician-office visits, ED visits, NHDS and Medicare hospitalizations, and mortality was examined using weighted least-squares regression, where the weights were the inverse of the squared SE.
Results
Prevalence (BRFSS Telephone Survey)
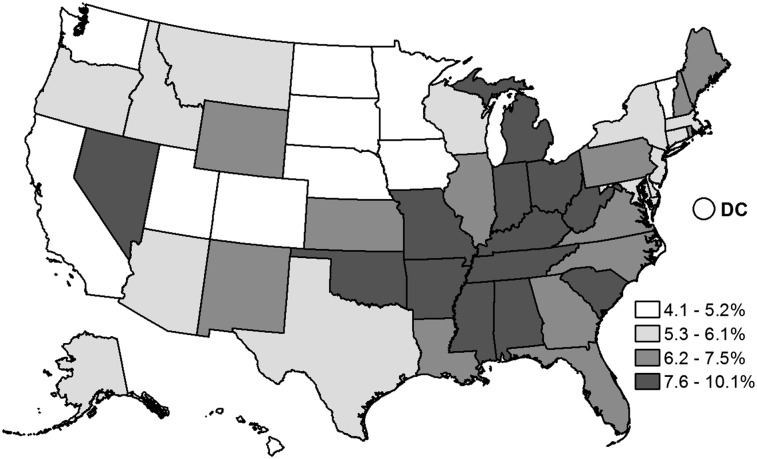
After age adjustment, 6.5% of US adults (unadjusted prevalence, 6.8%) representing 13.7 million noninstitutionalized adults aged ≥ 25 years in 2011 were estimated to have a self-reported physician diagnosis of COPD based on a telephone survey (Table 1). The age-adjusted prevalence displayed a strong age gradient, and the age-adjusted prevalence was higher in women (7.3%) than in men (5.7%) and higher in American Indian/Alaska Natives (11.0%) than in non-Hispanic whites (6.9%), non-Hispanic blacks (6.5%), Hispanics (4.1%), and Asian/Pacific Islanders (2.5%). The age-adjusted prevalence varied between states (Table 2). The highest age-adjusted prevalence of COPD in 2011 was clustered in the southern states and along the Ohio River Valley (Fig 1).
Table 1.
—Estimated Number and Prevalence of Self-Reported, Physician-Diagnosed COPD (Ever COPD, Chronic Bronchitis, or Emphysema) Among Adults Aged ≥ 25 Years, by Race, Sex, and Age Group—United States, Behavioral Risk Factor Surveillance System, 2011
| Characteristics | Estimated No.a | Age-Adjusted,b,c % | Unadjusted, %c |
| Race/ethnicity | |||
| White, non-Hispanic | 10,460,000 | 6.9 | 7.6 |
| Black, non-Hispanic | 1,418,000 | 6.5 | 6.4 |
| Hispanic | 1,030,000 | 4.1 | 3.6 |
| Asian/Pacific Islander | 173,000 | 2.5 | 2.2 |
| American Indian/Alaska Native | 247,000 | 11.0 | 11.5 |
| Other, non-Hispanic | 397,000 | 11.2 | 11.3 |
| Sex | |||
| Women | 8,197,000 | 7.3 | 7.8 |
| Men | 5,681,000 | 5.7 | 5.8 |
| Age group, y | |||
| 25-44 | 2,755,000 | … | 3.4 |
| 45-54 | 2,913,000 | … | 6.6 |
| 55-64 | 3,263,000 | … | 9.2 |
| 65-74 | 2,719,000 | … | 12.1 |
| ≥ 75 | 2,227,000 | … | 11.6 |
| Total | 13,724,000 | 6.5 | 6.8 |
Numbers for each variable may not add to total because of rounding.
Age-adjusted to the 2000 US standard population aged ≥ 25 y.
All relative SEs are ≤ 30%.
Table 2.
—Estimated Number and Prevalence of Self-Reported, Physician-Diagnosed COPD (Ever COPD, Chronic Bronchitis, or Emphysema) Among Adults Aged ≥ 25 Years, By State—United States, Behavioral Risk Factor Surveillance System, 2011
| State | Estimated No.a | Age-Adjusted,b,c % | Unadjusted, %c |
| Alabama | 330,000 | 9.9 | 10.4 |
| Alaska | 24,000 | 6.1 | 5.5 |
| Arizona | 253,000 | 5.8 | 6.1 |
| Arkansas | 171,000 | 8.1 | 8.9 |
| California | 1,073,000 | 4.7 | 4.9 |
| Colorado | 167,000 | 5.1 | 5.0 |
| Connecticut | 155,000 | 6.1 | 6.5 |
| Delaware | 35,000 | 5.4 | 5.8 |
| District of Columbia | 20,000 | 5.0 | 4.9 |
| Florida | 1,086,000 | 7.5 | 8.4 |
| Georgia | 462,000 | 7.4 | 7.4 |
| Hawaii | 43,000 | 4.5 | 4.7 |
| Idaho | 58,000 | 5.7 | 5.9 |
| Illinois | 549,000 | 6.4 | 6.6 |
| Indiana | 390,000 | 8.9 | 9.3 |
| Iowa | 109,000 | 5.0 | 5.5 |
| Kansas | 134,000 | 6.9 | 7.3 |
| Kentucky | 306,000 | 10.1 | 10.6 |
| Louisiana | 213,000 | 7.0 | 7.3 |
| Maine | 79,000 | 7.5 | 8.5 |
| Maryland | 239,000 | 6.1 | 6.2 |
| Massachusetts | 283,000 | 6.0 | 6.4 |
| Michigan | 574,000 | 8.2 | 8.8 |
| Minnesota | 148,000 | 4.1 | 4.2 |
| Mississippi | 170,000 | 8.6 | 9.0 |
| Missouri | 353,000 | 8.3 | 8.9 |
| Montana | 44,000 | 6.0 | 6.6 |
| Nebraska | 65,000 | 5.2 | 5.5 |
| Nevada | 143,000 | 7.9 | 8.1 |
| New Hampshire | 61,000 | 6.4 | 6.9 |
| New Jersey | 329,000 | 5.3 | 5.6 |
| New Mexico | 92,000 | 6.5 | 6.9 |
| New York | 822,000 | 6.0 | 6.3 |
| North Carolina | 458,000 | 6.9 | 7.3 |
| North Dakota | 21,000 | 4.5 | 5.0 |
| Ohio | 646,000 | 7.9 | 8.4 |
| Oklahoma | 225,000 | 8.6 | 9.3 |
| Oregon | 168,000 | 5.9 | 6.5 |
| Pennsylvania | 626,000 | 6.7 | 7.3 |
| Rhode Island | 49,000 | 6.5 | 7.0 |
| South Carolina | 252,000 | 7.7 | 8.2 |
| South Dakota | 31,000 | 5.2 | 5.9 |
| Tennessee | 391,000 | 8.6 | 9.2 |
| Texas | 928,000 | 6.0 | 5.9 |
| Utah | 68,000 | 4.4 | 4.3 |
| Vermont | 24,000 | 4.9 | 5.6 |
| Virginia | 363,000 | 6.6 | 6.8 |
| Washington | 205,000 | 4.4 | 4.5 |
| West Virginia | 124,000 | 8.8 | 9.7 |
| Wisconsin | 219,000 | 5.4 | 5.8 |
| Wyoming | 25,000 | 6.2 | 6.7 |
| Total | 13,724,000 | 6.5 | 6.8 |
Numbers may not add to total because of rounding.
Age-adjusted to the 2000 US standard population aged ≥ 25 y.
All relative SEs are ≤ 30%.
Figure 1.
Age-adjusted prevalence (%) of self-reported physician-diagnosed COPD among adults aged ≥ 25 years, by state—United States, Behavioral Risk Factor Surveillance System, 2011.
Prevalence (NHIS Interview Survey)
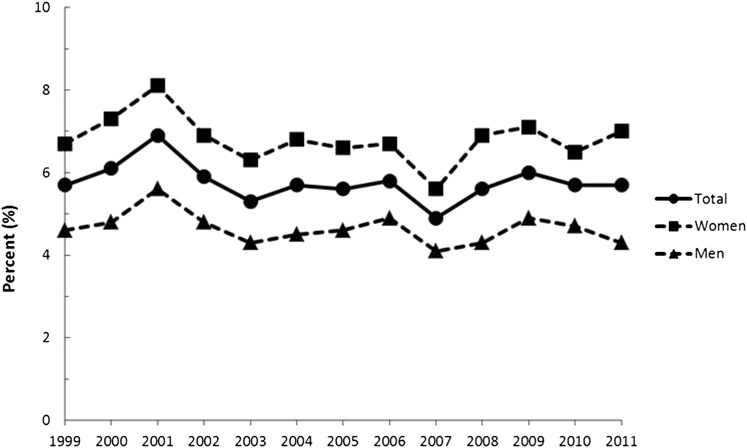
During the period from 1999 to 2011, the estimated numbers (Table 3) and age-adjusted prevalence of COPD (Table 4) fluctuated. Prevalence increased among successive age groups up to age 65 years and older, and the age-adjusted prevalence was usually higher among non-Hispanic whites compared with non-Hispanic blacks or Hispanics. The annual age-adjusted prevalence was higher in women than in men (Fig 2). The highest age-adjusted prevalence for both men and women was observed in 2001. Despite substantial interyear variation in age-adjusted prevalence estimates, significant tests for linear trend suggested declines during 1999 to 2011 in the age-adjusted prevalence among all adults (P = .019) and adults aged 25 to 44 years (P < .001).
Table 3.
—Estimated Annual Number of Adults Aged ≥ 25 Years With Self-Reported Physician-Diagnosed COPD (Lifetime Emphysema or Chronic Bronchitis During the Preceding 12 Months), by Race/Ethnicity, Sex, and Age Group—United States, National Health Interview Survey, 1999-2011
| Variable | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 |
| Race | |||||||||||||
| White, non-Hispanic | 8,193,000 | 8,792,000 | 10,034,000 | 8,449,000 | 8,050,000 | 8,792,000 | 8,751,000 | 9,105,000 | 7,789,000 | 9,275,000 | 9,902,000 | 9,153,000 | 9,038,000 |
| Black, non-Hispanic | 773,000 | 969,000 | 1,177,000 | 1,127,000 | 958,000 | 937,000 | 1,049,000 | 1,149,000 | 889,000 | 1,036,000 | 1,178,000 | 1,227,000 | 1,433,000 |
| Hispanic | 512,000 | 573,000 | 655,000 | 621,000 | 601,000 | 693,000 | 655,000 | 679,000 | 683,000 | 655,000 | 910,000 | 927,000 | 987,000 |
| Other, non-Hispanic | 224,000 | 182,000 | 273,000 | 253,000 | 214,000 | 261,000 | 236,000 | 376,000 | 285,000 | 324,000 | 347,000 | 323,000 | 441,000 |
| Sex | |||||||||||||
| Women | 6,126,000 | 6,717,000 | 7,550,000 | 6,514,000 | 6,168,000 | 6,750,000 | 6,677,000 | 6,891,000 | 5,849,000 | 7,266,000 | 7,682,000 | 7,066,000 | 7,658,000 |
| Men | 3,576,000 | 3,798,000 | 4,588,000 | 3,936,000 | 3,655,000 | 3,934,000 | 4,013,000 | 4,419,000 | 3,796,000 | 4,024,000 | 4,655,000 | 4,564,000 | 4,241,000 |
| Age group, y | |||||||||||||
| 25-44 | 3,087,000 | 3,157,000 | 3,899,000 | 3,129,000 | 2,526,000 | 2,987,000 | 2,868,000 | 2,552,000 | 2,159,000 | 2,795,000 | 2,597,000 | 2,699,000 | 2,560,000 |
| 45-54 | 1,811,000 | 2,184,000 | 2,671,000 | 2,311,000 | 1,964,000 | 2,294,000 | 2,274,000 | 2,461,000 | 2,039,000 | 2,703,000 | 2,773,000 | 2,383,000 | 2,430,000 |
| 55-64 | 1,725,000 | 1,879,000 | 2,135,000 | 2,014,000 | 2,126,000 | 2,043,000 | 2,199,000 | 2,747,000 | 2,351,000 | 2,330,000 | 2,937,000 | 2,740,000 | 3,053,000 |
| 65-74 | 1,639,000 | 1,721,000 | 1,773,000 | 1,678,000 | 1,791,000 | 1,702,000 | 1,845,000 | 1,703,000 | 1,624,000 | 1,902,000 | 2,120,000 | 2,018,000 | 2,253,000 |
| ≥ 75 | 1,439,000 | 1,573,000 | 1,661,000 | 1,318,000 | 1,414,000 | 1,658,000 | 1,504,000 | 1,847,000 | 1,473,000 | 1,560,000 | 1,910,000 | 1,790,000 | 1,604,000 |
| Total | 9,702,000 | 10,515,000 | 12,138,000 | 10,450,000 | 9,822,000 | 10,683,000 | 10,690,000 | 11,310,000 | 9,646,000 | 11,290,000 | 12,337,000 | 11,630,000 | 11,899,000 |
Numbers for each variable may not add to total because of rounding.
Table 4.
—Estimated Annual Prevalence of Self-Reported Physician-Diagnosed COPD (Lifetime Emphysema or Chronic Bronchitis During the Preceding 12 Months) Among Adults Aged ≥ 25 Years, by Race/Ethnicity, Sex, and Age Group—United States, National Health Interview Survey, 1999-2011
| Variable | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | P for Linear Trend |
| Racea | ||||||||||||||
| White, non-Hispanic | 6.1 | 6.6 | 7.5 | 6.2 | 5.7 | 6.3 | 6.1 | 6.3 | 5.4 | 6.4 | 6.7 | 6.1 | 6.0 | .130 |
| Black, non-Hispanic | 4.3 | 5.4 | 6.3 | 6.0 | 5.0 | 4.8 | 5.2 | 5.4 | 4.2 | 4.6 | 5.3 | 5.5 | 6.2 | .443 |
| Hispanic | 3.6 | 3.9 | 4.3 | 3.7 | 3.6 | 3.9 | 3.3 | 3.5 | 3.3 | 3.1 | 4.1 | 3.9 | 4.3 | .805 |
| Other, non-Hispanic | 4.0 | 2.8 | 3.9 | 3.2 | 3.3 | 3.6 | 2.9 | 4.1 | 2.9 | 3.1 | 3.4 | 3.1 | 3.9 | .626 |
| Sexa | ||||||||||||||
| Women | 6.7 | 7.3 | 8.1 | 6.9 | 6.3 | 6.8 | 6.6 | 6.7 | 5.6 | 6.9 | 7.1 | 6.5 | 7.0 | .136 |
| Men | 4.6 | 4.8 | 5.6 | 4.8 | 4.3 | 4.5 | 4.6 | 4.9 | 4.1 | 4.3 | 4.9 | 4.7 | 4.3 | .063 |
| Age group, y | ||||||||||||||
| 25-44 | 3.7 | 3.9 | 4.8 | 3.9 | 3.1 | 3.6 | 3.5 | 3.1 | 2.6 | 3.4 | 3.2 | 3.3 | 3.2 | < .001 |
| 45-54 | 5.1 | 5.9 | 7.0 | 5.9 | 4.9 | 5.6 | 5.4 | 5.7 | 4.7 | 6.2 | 6.3 | 5.4 | 5.6 | .655 |
| 55-64 | 7.5 | 8.0 | 8.8 | 7.9 | 7.7 | 7.1 | 7.3 | 8.8 | 7.2 | 7.0 | 8.4 | 7.7 | 8.2 | .929 |
| 65-74 | 9.2 | 9.6 | 10.0 | 9.5 | 9.9 | 9.3 | 10.0 | 8.9 | 8.4 | 9.6 | 10.3 | 9.5 | 10.3 | .566 |
| ≥ 75 | 9.8 | 10.6 | 11.0 | 8.6 | 8.8 | 10.2 | 9.1 | 11.1 | 8.7 | 9.0 | 11.1 | 10.3 | 9.0 | .679 |
| Totala | 5.7 | 6.1 | 6.9 | 5.9 | 5.3 | 5.7 | 5.6 | 5.8 | 4.9 | 5.6 | 6.0 | 5.7 | 5.7 | .019 |
| Totalb | 5.6 | 6.0 | 6.9 | 5.9 | 5.3 | 5.7 | 5.6 | 5.9 | 5.0 | 5.8 | 6.2 | 5.8 | 5.9 | .372 |
Annual prevalence per 100 population. All relative SEs are ≤ 30%.
Age-adjusted to the 2000 US standard population aged ≥ 25 y.
Unadjusted prevalence.
Figure 2.
Age-adjusted prevalence (%) of self-reported physician-diagnosed COPD among adults aged ≥ 25 years, by sex and year—United States, National Health Interview Survey, 1999-2011.
Physician Office Visits (NAMCS)
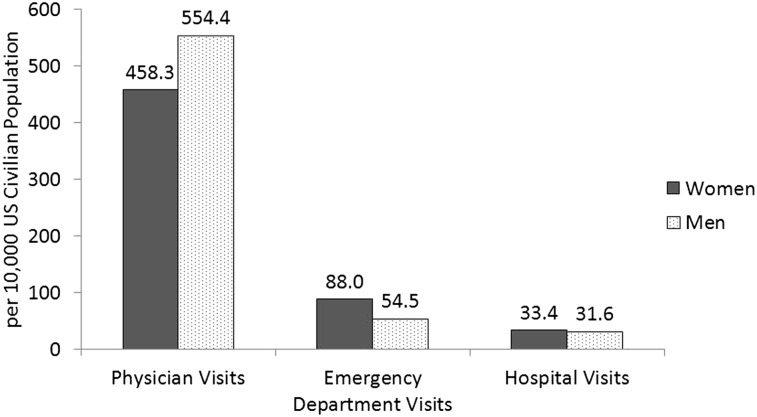
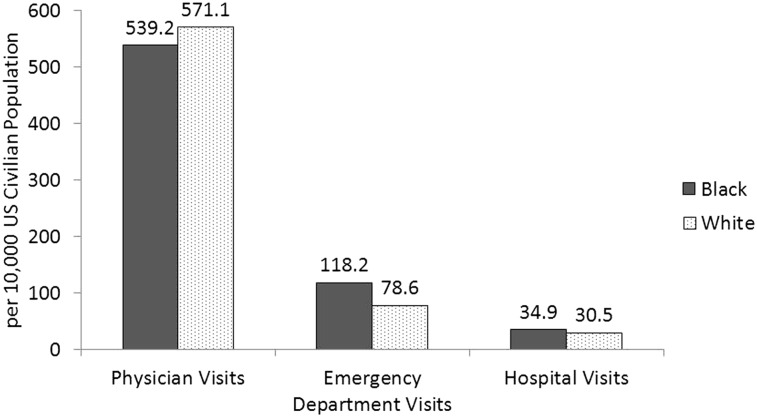
In 2010, there were an estimated 10.3 million (unadjusted, 516.1 per 10,000 US civilian population; age-adjusted, 494.8 per 10,000 US civilian population) physician office visits with a first-listed diagnosis of COPD among adults aged ≥ 25 years. The age-adjusted rate of office visits for COPD was higher among men than women in 2010 (Fig 3) and higher among whites than blacks during 2009 to 2010 (Fig 4). There was considerable temporal variability in the estimated number of physician-based office visits (Table 5). As expected for a chronic disease, age-specific rates for office visits for COPD increased substantially within each given year (Table 6), and age-specific rates declined during 1999 to 2010 among those aged 45 to 54 years (P = .033). No clear time trend was evident for age-adjusted rates among any group defined by sex or race (Table 6).
Figure 3.
Sex-specific age-adjusted rates (per 10,000 US civilian population) of physician office visits, ED visits, and hospital visits for COPD as the first-listed diagnosis among adults aged ≥ 25 years—United States, National Ambulatory Medical Care Survey, National Hospital Ambulatory Medical Care Survey, National Hospital Discharge Survey, 2010.
Figure 4.
Race-specific age-adjusted rates (per 10,000 US civilian population) of physician office visits, ED visits, and hospital visits for COPD as the first-listed diagnosis among adults aged ≥ 25 years—United States, National Ambulatory Medical Care Survey, National Hospital Ambulatory Medical Care Survey, National Hospital Discharge Survey, 2009-2010.
Table 5.
—Estimated Annual Number of Physician Office Visits for COPD as the First-Listed Diagnosis Among Adults Aged ≥ 25 Years, by Race, Sex, and Age Group—United States, National Ambulatory Medical Care Survey, 1999-2010
| Variable | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 |
| Racea | ||||||||||||
| White | 9,138,000 | 6,996,000 | 9,907,000 | 13,800,000 | 10,485,000 | 10,034,000 | 12,684,000 | 11,236,000 | 8,853,000 | 9,009,000 | 11,434,000 | 8,527,000 |
| Black | … | … | … | … | … | … | … | … | … | … | … | … |
| Sex | ||||||||||||
| Women | 6,080,000 | 4,041,000 | 6,260,000 | 9,391,000 | 6,667,000 | 6,878,000 | 6,405,000 | 6,929,000 | 6,099,000 | 5,947,000 | 8,001,000 | 5,210,000 |
| Men | 4,275,000 | 3,956,000 | 4,483,000 | 5,697,000 | 5,672,000 | 4,606,000 | 6,667,000 | 6,016,000 | 4,488,000 | 3,663,000 | 4,940,000 | 5,081,000 |
| Age group, y | ||||||||||||
| 25-44 | 1,784,000 | 1,446,000 | 1,850,000 | 3,022,000 | 2,709,000 | 2,126,000 | 2,106,000 | 1,301,000 | 1,913,000 | 1,902,000 | 1,649,000 | … |
| 45-54 | 1,295,000 | … | … | 1,970,000 | 2,405,000 | 1,599,000 | … | 1,758,000 | 1,409,000 | 1,005,000 | 2,158,000 | … |
| 55-64 | 2,276,000 | … | … | 2,538,000 | 1,704,000 | 2,440,000 | 2,415,000 | 3,171,000 | 1,919,000 | 2,077,000 | 3,024,000 | 2,153,000 |
| 65-74 | 2,854,000 | 2,175,000 | 2,563,000 | 3,878,000 | 2,871,000 | 2,499,000 | 3,349,000 | 3,418,000 | 3,191,000 | 1,895,000 | 2,303,000 | 3,191,000 |
| ≥ 75 | 2,147,000 | 2,084,000 | 2,920,000 | 3,680,000 | 2,649,000 | 2,820,000 | 3,522,000 | 3,298,000 | 2,154,000 | 2,730,000 | 3,808,000 | 3,431,000 |
| Total | 10,355,000 | 7,997,000 | 10,743,000 | 15,087,000 | 12,339,000 | 11,484,000 | 13,072,000 | 12,945,000 | 10,586,000 | 9,609,000 | 12,941,000 | 10,291,000 |
Numbers for each variable may not add to total because of rounding. COPD includes ICD-9-CM codes 490-492 or 496. Ellipses indicate unreliable estimate (relative SE > 30% and/or number of records < 30). ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification.
Data not available for other specific race groups.
Table 6.
—Estimated Annual Rate of Physician Office Visits for COPD as the First-Listed Diagnosis Among Adults Aged ≥ 25 Years, by Race, Sex, and Age Group—United States, National Ambulatory Medical Care Survey, 1999-2010
| Variable | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | P for Linear Trend |
| Racea,b | |||||||||||||
| White | 623.4 | 473.1 | 651.0 | 897.2 | 676.1 | 633.4 | 791.7 | 679.1 | 541.6 | 537.4 | 661.1 | 481.0 | .585 |
| Black | … | … | … | … | … | … | … | … | … | … | … | … | … |
| Sexa | |||||||||||||
| Women | 660.2 | 432.4 | 647.4 | 955.5 | 678.8 | 679.0 | 622.1 | 656.2 | 587.7 | 557.3 | 726.3 | 458.3 | .725 |
| Men | 572.0 | 519.5 | 583.3 | 714.6 | 701.4 | 547.5 | 789.3 | 688.6 | 515.6 | 410.5 | 525.4 | 554.4 | .233 |
| Age group, y | |||||||||||||
| 25-44 | 216.2 | 176.3 | 223.0 | 364.8 | 329.5 | 258.9 | 256.8 | 158.5 | 234.2 | 234.0 | 203.8 | … | .082 |
| 45-54 | 363.7 | … | … | 495.5 | 594.3 | 387.3 | … | 409.5 | 323.7 | 228.4 | 488.0 | … | .033 |
| 55-64 | 987.5 | … | … | 960.0 | 614.4 | 843.8 | 799.8 | 1,009.1 | 589.7 | 619.7 | 873.5 | 600.7 | .826 |
| 65-74 | 1,603.7 | 1,224.9 | 1,417.7 | 2,150.8 | 1,586.8 | 1,371.6 | 1,820.3 | 1,830.4 | 1,670.3 | 953.4 | 1,120.6 | 1,505.7 | .264 |
| ≥ 75 | 1,464.0 | 1,393.7 | 1,867.6 | 2,309.7 | 1,636.7 | 1,716.1 | 2,102.2 | 1,946.0 | 1,257.2 | 1,573.2 | 2,189.8 | 1,936.1 | .380 |
| Totala | 609.2 | 466.6 | 604.8 | 836.2 | 673.5 | 614.2 | 691.6 | 663.1 | 543.0 | 483.3 | 632.3 | 494.8 | .541 |
| Totalc | 596.4 | 456.2 | 594.5 | 824.5 | 668.0 | 614.2 | 689.9 | 674.1 | 545.8 | 490.1 | 654.6 | 516.1 | .848 |
Annual rate per 10,000 US civilian population. COPD includes ICD-9-CM codes 490-492 or 496. Ellipses indicate unreliable estimate (relative SE > 30% and/or number of records < 30). See Table 5 legend for expansion of abbreviation.
Age-adjusted to the 2000 US standard population aged ≥ 25 y.
Data not available for other specific race groups.
Unadjusted rate.
ED Visits (NHAMCS)
In 2010, there were an estimated 1.5 million (unadjusted rate, 73.6 per 10,000 US civilian population; age-adjusted rate, 72.0 per 10,000 US civilian population) ED visits with a first-listed diagnosis of COPD among adults aged ≥ 25 years. The age-adjusted rate of ED visits for COPD was higher among women than men in 2010 (Fig 3) and among blacks than whites during 2009 to 2010 (Fig 4). The estimated annual number of ED visits for COPD fluctuated (Table 7). There was a considerable increase each year in age-specific rates for ED visits with advancing age up to ages 65 years and older (Table 8), but there were no significant temporal trends during 1999 to 2010 in age-specific and age-adjusted rates for any group defined by age, race, or sex.
Table 7.
—Estimated Annual Numbers of ED Visits for COPD as the First-Listed Diagnosis Among Adults Aged ≥ 25 Years, by Race, Sex, and Age Group—United States, National Hospital Ambulatory Medical Care Survey, 1999-2010
| Variable | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 |
| Racea | ||||||||||||
| White | 1,205,000 | 1,278,000 | 1,039,000 | 1,046,000 | 1,230,000 | 957,000 | 1,112,000 | 973,000 | 1,067,000 | 1,295,000 | 1,452,000 | 1,179,000 |
| Black | 285,000 | 243,000 | 226,000 | 229,000 | 273,000 | 172,000 | 342,000 | 327,000 | 207,000 | 265,000 | 272,000 | 253,000 |
| Sex | ||||||||||||
| Women | 802,000 | 898,000 | 717,000 | 769,000 | 907,000 | 619,000 | 841,000 | 729,000 | 842,000 | 861,000 | 1,029,000 | 945,000 |
| Men | 730,000 | 651,000 | 582,000 | 523,000 | 648,000 | 528,000 | 647,000 | 587,000 | 455,000 | 726,000 | 734,000 | 523,000 |
| Age group, y | ||||||||||||
| 25-44 | 448,000 | 481,000 | 488,000 | 418,000 | 372,000 | 356,000 | 492,000 | 314,000 | 397,000 | 358,000 | 446,000 | 388,000 |
| 45-54 | 270,000 | 194,000 | 193,000 | 183,000 | 294,000 | 151,000 | 215,000 | 293,000 | 255,000 | 277,000 | 297,000 | 284,000 |
| 55-64 | 269,000 | 315,000 | 197,000 | 226,000 | 256,000 | 184,000 | 268,000 | 254,000 | 212,000 | 321,000 | 293,000 | 290,000 |
| 65-74 | 233,000 | 267,000 | 207,000 | 219,000 | 317,000 | 253,000 | 201,000 | 251,000 | 234,000 | 321,000 | 388,000 | 286,000 |
| ≥ 75 | 312,000 | 292,000 | 212,000 | 246,000 | 315,000 | 202,000 | 311,000 | 204,000 | 198,000 | 311,000 | 340,000 | 221,000 |
| Total | 1,532,000 | 1,549,000 | 1,299,000 | 1,292,000 | 1,555,000 | 1,147,000 | 1,488,000 | 1,316,000 | 1,297,000 | 1,588,000 | 1,763,000 | 1,468,000 |
Annual rate per 10,000 US civilian population. COPD includes ICD-9-CM codes 490-492 or 496. See Table 5 legend for expansion of abbreviation.
Data not available for other specific race groups.
Table 8.
—Estimated Annual Rate of ED Visits for COPD as the First-Listed Diagnosis Among Adults Aged ≥ 25 Years, by Race, Sex, and Age Group—United States, National Hospital Ambulatory Medical Care Survey, 1999-2010
| Variable | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | P for Linear Trend |
| Racea,b | |||||||||||||
| White | 82.7 | 86.7 | 69.0 | 68.4 | 78.9 | 61.4 | 70.6 | 60.4 | 66.0 | 77.8 | 86.9 | 70.6 | .541 |
| Black | 160.8 | 133.0 | 120.8 | 120.0 | 143.4 | 87.7 | 166.9 | 153.2 | 94.4 | 121.1 | 123.4 | 112.6 | .411 |
| Sexa | |||||||||||||
| Women | 87.7 | 96.9 | 75.0 | 79.0 | 91.5 | 62.5 | 83.5 | 71.3 | 82.1 | 82.4 | 97.9 | 88.0 | .769 |
| Men | 95.2 | 82.4 | 70.4 | 62.4 | 77.0 | 62.5 | 74.3 | 64.9 | 49.1 | 78.4 | 79.3 | 54.5 | .072 |
| Age group, y | |||||||||||||
| 25-44 | 54.3 | 58.6 | 58.9 | 50.4 | 45.2 | 43.4 | 60.0 | 38.2 | 48.7 | 44.1 | 55.0 | 48.2 | .166 |
| 45-54 | 75.8 | 52.5 | 49.7 | 46.0 | 72.5 | 36.5 | 51.1 | 68.2 | 58.7 | 62.8 | 67.1 | 64.4 | .281 |
| 55-64 | 116.8 | 133.5 | 78.4 | 85.4 | 92.4 | 63.8 | 88.8 | 80.9 | 65.1 | 95.8 | 84.7 | 80.8 | .478 |
| 65-74 | 130.9 | 150.3 | 114.7 | 121.6 | 175.4 | 139.1 | 109.2 | 134.7 | 122.2 | 161.3 | 188.6 | 135.0 | .505 |
| ≥ 75 | 212.9 | 195.2 | 135.8 | 154.6 | 194.9 | 123.0 | 185.8 | 120.4 | 115.8 | 179.2 | 195.5 | 124.5 | .142 |
| Totala | 89.8 | 89.6 | 72.5 | 71.2 | 84.6 | 61.9 | 78.8 | 67.8 | 66.8 | 79.5 | 88.3 | 72.0 | .432 |
| Totalc | 88.3 | 88.4 | 71.9 | 70.6 | 84.2 | 61.3 | 78.5 | 68.5 | 66.9 | 81.0 | 89.2 | 73.6 | .428 |
Annual rate per 10,000 US civilian population. COPD includes ICD-9-CM codes 490-492 or 496. All relative SEs are ≤ 30%. See Table 5 legend for expansion of abbreviation.
Age-adjusted to the 2000 US standard population aged ≥ 25 y.
Data not available for other specific race groups.
Unadjusted rate.
Hospitalizations (NHDS)
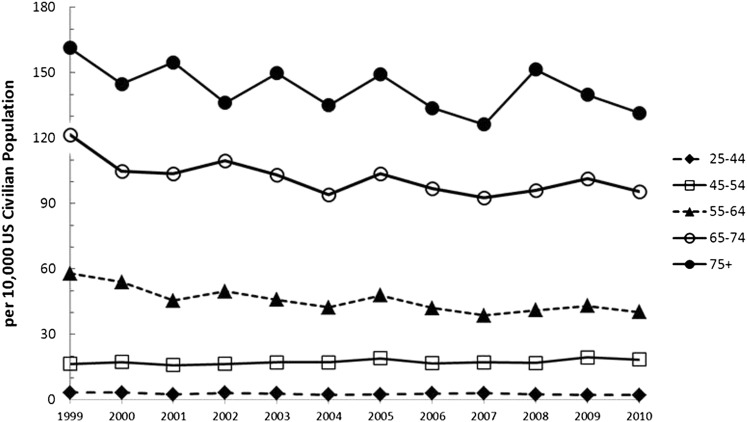
In 2010, there were an estimated 699,000 hospitalizations (unadjusted rate, 34.4 per 10,000 US civilian population; age-adjusted rate, 32.2 per 10,000 US civilian population) for COPD as the first-listed diagnosis among adults aged ≥ 25 years. Age-adjusted rates of hospitalizations for COPD varied little between men and women in 2010 (Fig 3) or between blacks and whites during 2009 to 2010 (Fig 4). The annual number of hospitalizations for COPD fluctuated between 1999 and 2010 (Table 9). The age-specific hospital rates for COPD increased with advancing age each year (Fig 5), and there was a decline in age-specific rates during 1999 to 2010 among adults aged 25 to 44 years (P = .039), adults aged 55 to 64 years (P = .001), adults aged 65 to 74 years (P = .005), and adults aged ≥ 75 years (P = .018) (Table 10). Declining trends for age-adjusted rates for COPD hospitalization during 1999 to 2010 were observed among all adults (P = .001), men (P < .001), and women (P = .022) (Table 10).
Table 9.
—Estimated Annual Number of Hospitalizations for COPD as the First-Listed Discharge Diagnosis Among Adults Aged ≥ 25 Years, by Race, Sex, and Age Group—United States, National Hospital Discharge Survey, 1999-2010
| Variable | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 |
| Racea | ||||||||||||
| White | 500,000 | 441,000 | 457,000 | 462,000 | 460,000 | 429,000 | 505,000 | 452,000 | 440,000 | 493,000 | 573,000 | 543,000 |
| Black | 59,000 | 47,000 | 54,000 | 53,000 | 49,000 | 45,000 | 50,000 | 55,000 | 52,000 | 59,000 | 62,000 | 80,000 |
| Sex | ||||||||||||
| Women | 402,000 | 350,000 | 362,000 | 368,000 | 369,000 | 336,000 | 387,000 | 344,000 | 345,000 | 414,000 | 416,000 | 398,000 |
| Men | 300,000 | 297,000 | 288,000 | 293,000 | 304,000 | 291,000 | 324,000 | 312,000 | 294,000 | 296,000 | 312,000 | 301,000 |
| Age group, y | ||||||||||||
| 25-44 | 28,000 | 28,000 | 21,000 | 27,000 | 24,000 | 19,000 | 21,000 | 23,000 | 25,000 | 20,000 | 18,000 | 17,000 |
| 45-54 | 59,000 | 64,000 | 62,000 | 66,000 | 70,000 | 72,000 | 81,000 | 72,000 | 75,000 | 75,000 | 86,000 | 81,000 |
| 55-64 | 134,000 | 129,000 | 115,000 | 132,000 | 128,000 | 123,000 | 145,000 | 133,000 | 126,000 | 138,000 | 150,000 | 145,000 |
| 65-74 | 219,000 | 188,000 | 190,000 | 200,000 | 189,000 | 173,000 | 193,000 | 183,000 | 179,000 | 193,000 | 211,000 | 205,000 |
| ≥ 75 | 261,000 | 239,000 | 263,000 | 236,000 | 263,000 | 241,000 | 271,000 | 245,000 | 234,000 | 284,000 | 262,000 | 251,000 |
| Total | 702,000 | 647,000 | 650,000 | 662,000 | 673,000 | 628,000 | 711,000 | 657,000 | 639,000 | 710,000 | 728,000 | 699,000 |
Numbers for each variable may not add to total because of rounding. COPD includes ICD-9-CM codes 490-492 or 496. See Table 5 legend for expansion of abbreviation.
Data not available for other specific race groups. Race was not imputed. Percent missing data for race are shown in e-Table 5 (647.6KB, pdf) .
Figure 5.
Age-specific rates (per 10,000 US civilian population) of hospitalizations for COPD as the first-listed discharge diagnosis among adults aged ≥ 25 years, by year—United States, National Hospital Discharge Survey, 1999-2010.
Table 10.
—Estimated Annual Rates of Hospitalizations for COPD as the First-Listed Discharge Diagnosis Among Adults Aged ≥ 25 Years, by Race, Sex, and Age Group—United States, National Hospital Discharge Survey, 1999-2010
| Variable | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | P for Linear Trend |
| Racea,b | |||||||||||||
| White | 32.7 | 28.5 | 28.5 | 28.6 | 28.0 | 25.8 | 29.8 | 26.3 | 25.3 | 27.6 | 31.6 | 29.5 | .104 |
| Black | 37.6 | 29.2 | 29.2 | 30.4 | 28.5 | 24.9 | 26.9 | 29.9 | 26.2 | 28.8 | 30.2 | 39.5 | .563 |
| Sexa | |||||||||||||
| Women | 40.8 | 35.3 | 35.3 | 35.3 | 34.5 | 31.1 | 35.2 | 30.9 | 30.4 | 35.6 | 35.3 | 33.4 | .022 |
| Men | 39.9 | 39.0 | 39.0 | 36.7 | 37.4 | 35.3 | 38.4 | 36.4 | 33.1 | 32.9 | 33.9 | 31.6 | < .001 |
| Age group, y | |||||||||||||
| 25-44 | 3.3 | 3.3 | 2.4 | 3.2 | 2.9 | 2.3 | 2.5 | 2.8 | 3.0 | 2.4 | 2.2 | 2.1 | .039 |
| 45-54 | 16.5 | 17.3 | 15.9 | 16.5 | 17.1 | 17.2 | 19.0 | 16.7 | 17.1 | 16.9 | 19.4 | 18.4 | .102 |
| 55-64 | 57.9 | 54.0 | 45.5 | 49.7 | 45.8 | 42.3 | 47.8 | 42.1 | 38.6 | 41.0 | 43.1 | 40.2 | .001 |
| 65-74 | 121.6 | 104.7 | 103.6 | 109.7 | 103.0 | 93.9 | 103.7 | 96.8 | 92.7 | 96.0 | 101.5 | 95.5 | .005 |
| ≥ 75 | 161.3 | 144.8 | 154.7 | 136.1 | 149.7 | 135.0 | 149.1 | 133.7 | 126.2 | 151.4 | 139.8 | 131.4 | .018 |
| Totala | 40.2 | 36.6 | 36.6 | 35.5 | 35.5 | 32.5 | 36.1 | 32.8 | 31.4 | 34.1 | 34.3 | 32.2 | .001 |
| Totalc | 39.7 | 36.2 | 35.4 | 35.5 | 35.8 | 33.0 | 36.8 | 33.6 | 32.4 | 35.6 | 36.2 | 34.4 | .018 |
Annual rate per 10,000 US civilian population. COPD includes ICD-9-CM codes 490-492 or 496. All relative SEs are ≤ 30%. See Table 5 legend for expansion of abbreviation.
Age-adjusted to the 2000 US standard population aged ≥ 25 y.
Data not available for other specific race groups. Race was not imputed. Percent missing data for race are shown in e-Table 5 (647.6KB, pdf) .
Unadjusted rate.
Medicare Hospitalizations (Medicare Part A Hospital Claims)
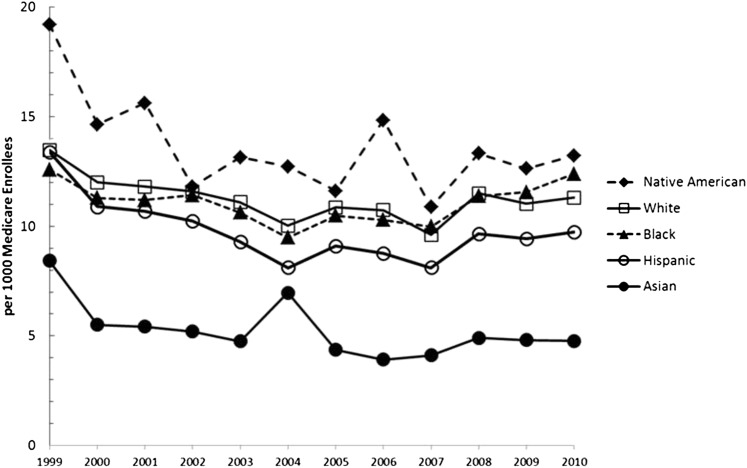
In 2010, there were 312,654 (unadjusted rate, 11.11 per 1,000 Medicare enrollees aged ≥ 65 years; age-adjusted rate, 11.18 per 1,000 Medicare enrollees aged ≥ 65 years) hospital discharge claims for COPD as the first-listed diagnosis. The annual number of Medicare hospitalizations for COPD fluctuated during 1999 to 2010 (Table 11). Age-specific rates for those aged 65 to 74 years declined significantly (P = .033) (Table 12). Age-adjusted rates were highest among Native American enrollees and lowest among Asian enrollees in most years (Fig 6). Age-adjusted rates for Medicare hospitalizations for COPD declined during 1999 to 2010 for all enrollees overall (P = .045) and men (P = .022), but the decline was not significant for women (P = .138) or for specific race groups (Table 12).
Table 11.
—Annual Number of Medicare Hospitalizations for COPD as the First-Listed Discharge Diagnosis Among Medicare Beneficiaries Aged ≥ 65 Years, by Race/Ethnicity, Sex, and Age Group—United States, Medicare Part A Hospital Claims, 1999-2010
| Variable | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 |
| Race/ethnicity | ||||||||||||
| White, non-Hispanic | 311,551 | 282,944 | 286,225 | 288,338 | 280,631 | 255,896 | 277,529 | 266,810 | 234,796 | 277,693 | 265,149 | 273,918 |
| Black, non-Hispanic | 25,468 | 23,545 | 24,280 | 25,530 | 24,313 | 22,003 | 24,312 | 22,740 | 21,344 | 23,893 | 24,611 | 27,106 |
| Hispanic | 4,422 | 4,030 | 4,256 | 4,347 | 4,183 | 3,945 | 4,505 | 4,196 | 3,892 | 4,531 | 4,517 | 4,770 |
| Native American | 581 | 519 | 577 | 1,018 | 1,210 | 1,229 | 1,228 | 1,553 | 1,176 | 1,468 | 1,432 | 1,547 |
| Asian | 1,818 | 1,553 | 1,683 | 1,772 | 1,750 | 2,865 | 1,901 | 1,719 | 1,879 | 2,327 | 2,369 | 2,442 |
| Sex | ||||||||||||
| Women | 194,756 | 177,658 | 179,941 | 181,588 | 176,902 | 162,180 | 174,986 | 167,743 | 149,181 | 174,940 | 168,625 | 175,597 |
| Men | 154,141 | 139,843 | 141,875 | 143,795 | 139,164 | 126,169 | 138,283 | 132,445 | 116,711 | 138,212 | 132,266 | 137,057 |
| Age group, y | ||||||||||||
| 65-74 | 152,179 | 136,721 | 138,118 | 137,777 | 136,354 | 122,701 | 131,321 | 125,471 | 111,455 | 130,057 | 128,891 | 134,072 |
| ≥ 75 | 196,718 | 180,780 | 183,698 | 187,606 | 179,802 | 165,648 | 181,948 | 174,717 | 154,437 | 183,095 | 172,000 | 178,582 |
| Total | 348,897 | 317,501 | 321,816 | 325,383 | 316,156 | 288,349 | 313,269 | 300,188 | 265,892 | 313,152 | 300891 | 312,654 |
COPD includes ICD-9-CM codes 490-492 or 496. See Table 5 legend for expansion of abbreviation.
Table 12.
—Annual Rates of Medicare Hospitalizations for COPD Among Medicare Beneficiaries Aged ≥ 65 Years, by Race/Ethnicity, Sex, and Age Group—United States, Medicare Part A Hospital Claims, 1999-2010
| Variable | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | P for Linear Trend |
| Racea | |||||||||||||
| White, non-Hispanic | 13.47 | 12.00 | 11.80 | 11.58 | 11.09 | 10.02 | 10.86 | 10.73 | 9.61 | 11.50 | 11.03 | 11.31 | .052 |
| Black, non-Hispanic | 12.59 | 11.29 | 11.19 | 11.42 | 10.63 | 9.48 | 10.49 | 10.29 | 9.98 | 11.37 | 11.55 | 12.39 | .831 |
| Hispanic | 13.39 | 10.89 | 10.68 | 10.24 | 9.30 | 8.12 | 9.09 | 8.77 | 8.14 | 9.66 | 9.44 | 9.73 | .081 |
| Native American | 19.21 | 14.65 | 15.62 | 11.80 | 13.14 | 12.73 | 11.61 | 14.84 | 10.88 | 13.32 | 12.62 | 13.23 | .394 |
| Asian | 8.42 | 5.50 | 5.42 | 5.20 | 4.75 | 6.96 | 4.36 | 3.92 | 4.11 | 4.91 | 4.81 | 4.77 | .108 |
| Sexa | |||||||||||||
| Women | 12.41 | 11.22 | 11.08 | 10.90 | 10.50 | 9.52 | 10.28 | 10.17 | 9.22 | 10.97 | 10.64 | 10.99 | .138 |
| Men | 14.81 | 13.14 | 12.83 | 12.53 | 11.81 | 10.54 | 11.47 | 11.23 | 9.99 | 11.91 | 11.34 | 11.56 | .022 |
| Age group, y | |||||||||||||
| 65-74 | 11.26 | 10.01 | 9.81 | 9.51 | 9.24 | 8.19 | 8.75 | 8.58 | 7.70 | 8.90 | 8.72 | 8.88 | .033 |
| ≥ 75 | 15.49 | 13.98 | 13.79 | 13.67 | 12.87 | 11.72 | 12.86 | 12.69 | 11.47 | 13.94 | 13.24 | 13.69 | .175 |
| Totala | 13.28 | 11.91 | 11.71 | 11.49 | 10.97 | 9.88 | 10.71 | 10.55 | 9.50 | 11.31 | 10.87 | 11.18 | .045 |
| Totalb | 13.31 | 11.94 | 11.74 | 11.53 | 11.00 | 9.91 | 10.74 | 10.58 | 9.51 | 11.29 | 10.83 | 11.11 | .034 |
Annual rate per 1,000 Medicare beneficiaries, aged ≥ 65 y, alive, entitled to Medicare Part A, and not in a managed care plan on July 1 of the given year. COPD includes ICD-9-CM codes 490-492 or 496. See Table 5 legend for expansion of abbreviation.
Age-adjusted to the 2000 US standard population aged ≥ 65 y.
Unadjusted rate.
Figure 6.
Race-specific age-adjusted rates (per 1,000 Medicare enrollees) of Medicare hospitalizations for COPD as the first-listed discharge diagnosis among Medicare enrollees aged ≥ 65 years, by year—United States, Medicare Part A hospital claims, 1999-2010.
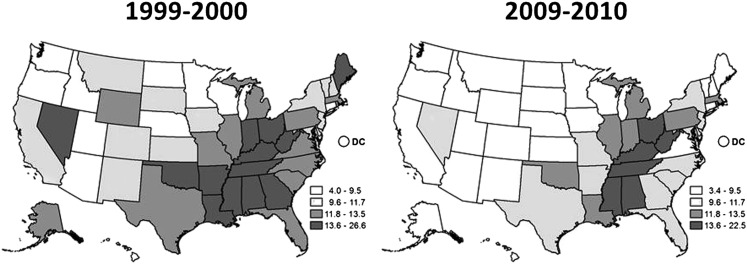
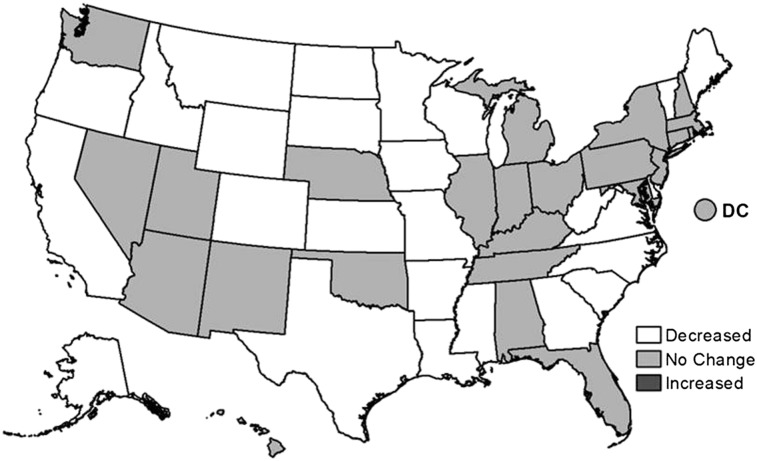
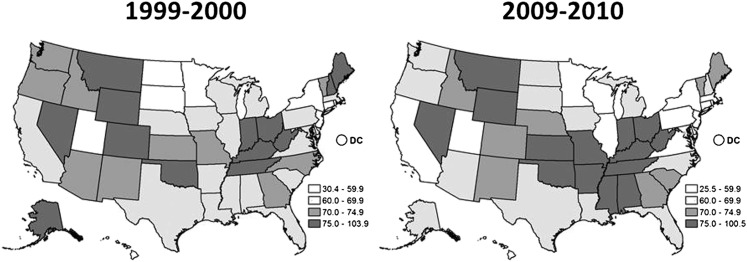
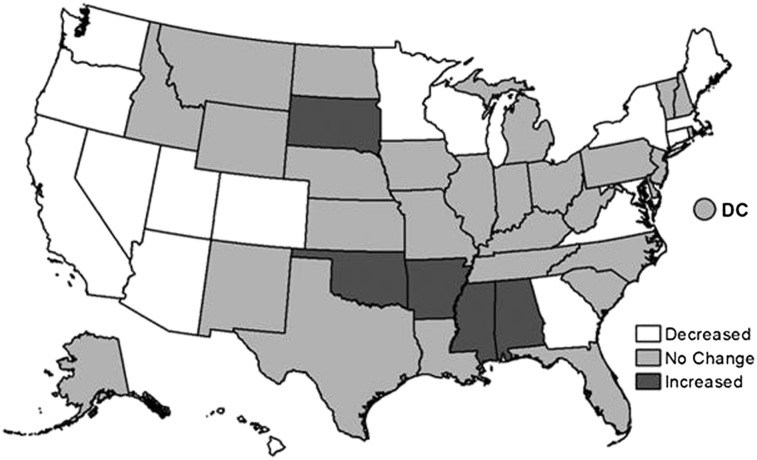
Medicare hospital claims data provide an opportunity to obtain state-specific estimates (Table 13). Changes in age-adjusted rates during 1999 to 2010 varied between states (Table 14). A comparison of state-specific Medicare hospital rates in 1999 to 2000 to those in 2009 to 2010 (Fig 7) demonstrates geographic clustering of the 10 states in 1999 to 2000, with the highest hospitalization rates (14.0-26.6 per 1,000 Medicare enrollees) along the Mississippi River and Ohio River valleys. By 2009 to 2010, there was a marked improvement in rates in many of those states. States with the highest age-adjusted Medicare hospitalization rates in 2009 to 2010 in Figure 7 are similar to those states in Figure 1, with the highest age-adjusted prevalence of COPD in 2011. Figure 8 shows that there were no significant increases in age-adjusted Medicare hospitalization rates in any state during 1999 to 2010 and identifies those states which have experienced no significant change or a significant decline (P < .05) during the past decade.
Table 13.
—Annual Number of Medicare Hospitalizations for COPD as the First-Listed Discharge Diagnosis Among Medicare Beneficiaries Aged ≥ 65 Years, by State—United States, Medicare Part A Hospital Claims, 1999-2010
| State | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 |
| Alabama | 8,996 | 8,172 | 8,751 | 8,779 | 8,442 | 7,216 | 7,842 | 7,098 | 6,805 | 8,132 | 7,686 | 7,704 |
| Alaska | 391 | 404 | 414 | 378 | 387 | 341 | 320 | 408 | 290 | 355 | 335 | 373 |
| Arizona | 3,317 | 2,890 | 2,914 | 3,152 | 3,101 | 3,006 | 3,638 | 2,967 | 2,652 | 3,543 | 3,482 | 4,082 |
| Arkansas | 5,444 | 5,033 | 4,991 | 5,202 | 4,798 | 4,148 | 4,563 | 4,598 | 3,651 | 3,957 | 3,858 | 3,956 |
| California | 20,181 | 17,174 | 17,142 | 17,382 | 17,045 | 14,601 | 15,331 | 14,392 | 14,367 | 17,093 | 17,302 | 18,743 |
| Colorado | 2,830 | 2,264 | 2,332 | 2,317 | 2,350 | 2,013 | 2,337 | 2,406 | 1,954 | 2,535 | 2,117 | 2,397 |
| Connecticut | 3,032 | 2,964 | 3,125 | 3,315 | 3,276 | 3,227 | 3,487 | 3,359 | 3,300 | 3,886 | 3,698 | 3,768 |
| Delaware | 983 | 1,038 | 992 | 1,028 | 1,047 | 1,088 | 1,188 | 1,052 | 1,069 | 1,105 | 1,066 | 1,257 |
| District of Columbia | 463 | 458 | 443 | 418 | 391 | 343 | 438 | 363 | 336 | 445 | 404 | 451 |
| Florida | 23,513 | 21,200 | 22,448 | 23,194 | 22,096 | 22,210 | 22,732 | 21,121 | 19,590 | 23,592 | 23,926 | 24,952 |
| Georgia | 9,983 | 9,269 | 9,434 | 9,591 | 9,089 | 8,215 | 9,146 | 9,092 | 7,491 | 8,617 | 8,660 | 8,517 |
| Hawaii | 470 | 412 | 421 | 406 | 379 | 377 | 386 | 369 | 373 | 424 | 410 | 424 |
| Idaho | 1,249 | 1,001 | 994 | 930 | 852 | 659 | 729 | 884 | 567 | 609 | 616 | 603 |
| Illinois | 16,794 | 14,861 | 15,180 | 15,556 | 14,669 | 13,354 | 14,618 | 14,566 | 13,146 | 16,660 | 16,089 | 16,021 |
| Indiana | 10,357 | 9,831 | 9,774 | 9,551 | 9,109 | 8,178 | 9,334 | 9,334 | 7,543 | 9,624 | 8,835 | 8,682 |
| Iowa | 5,008 | 4,308 | 4,234 | 3,734 | 3,369 | 2,977 | 2,940 | 3,736 | 2,424 | 2,774 | 2,546 | 2,645 |
| Kansas | 3,822 | 3,321 | 3,247 | 3,205 | 3,282 | 2,759 | 3,066 | 3,542 | 2,440 | 2,749 | 2,450 | 2,441 |
| Kentucky | 10,655 | 9,496 | 9,959 | 9,839 | 9,730 | 8,546 | 9,544 | 9,752 | 7,731 | 9,423 | 9,188 | 8,986 |
| Louisiana | 6,520 | 6,031 | 6,373 | 6,418 | 6,228 | 5,258 | 5,887 | 5,155 | 4,490 | 5,389 | 5,150 | 5,287 |
| Maine | 2,380 | 2,477 | 2,056 | 1,863 | 1,837 | 1,635 | 1,761 | 1,938 | 1,438 | 1,625 | 1,712 | 1,588 |
| Maryland | 5,437 | 5,283 | 5,631 | 5,746 | 5,695 | 5,211 | 5,898 | 6,221 | 6,223 | 7,086 | 6,470 | 6,522 |
| Massachusetts | 7,890 | 7,447 | 7,117 | 7,053 | 7,170 | 6,754 | 7,277 | 7,108 | 6,828 | 8,437 | 8,185 | 8,689 |
| Michigan | 14,207 | 12,606 | 12,377 | 13,285 | 12,984 | 12,892 | 13,915 | 13,152 | 11,491 | 13,053 | 12,627 | 14,282 |
| Minnesota | 4,764 | 4,130 | 4,291 | 4,061 | 3,745 | 3,560 | 3,667 | 3,354 | 2,513 | 3,097 | 2,862 | 2,930 |
| Mississippi | 6,361 | 6,017 | 6,191 | 6,117 | 5,851 | 5,128 | 5,666 | 5,090 | 4,164 | 4,858 | 5,005 | 4,983 |
| Missouri | 8,527 | 7,535 | 8,037 | 7,709 | 7,455 | 7,023 | 7,909 | 7,254 | 6,082 | 7,451 | 6,884 | 6,932 |
| Montana | 1,306 | 1,142 | 1,203 | 1,072 | 1,015 | 874 | 867 | 1,100 | 704 | 759 | 718 | 717 |
| Nebraska | 2,108 | 1,713 | 1,542 | 1,452 | 1,443 | 1,208 | 1,590 | 1,981 | 1,337 | 1,693 | 1,516 | 1,705 |
| Nevada | 1,969 | 1,551 | 1,488 | 1,576 | 1,529 | 1,332 | 1,544 | 1,547 | 1,346 | 1,754 | 1,890 | 2,062 |
| New Hampshire | 1,329 | 1,450 | 1,361 | 1,305 | 1,335 | 1,452 | 1,318 | 1,640 | 1,358 | 1,626 | 1,541 | 1,499 |
| New Jersey | 10,193 | 9,420 | 9,584 | 10,325 | 10,742 | 10,172 | 11,049 | 10,265 | 9,882 | 11,328 | 10,836 | 11,166 |
| New Mexico | 1,569 | 1,309 | 1,342 | 1,400 | 1,356 | 1,138 | 1,430 | 1,214 | 1,116 | 1,348 | 1,316 | 1,418 |
| New York | 20,526 | 18,680 | 17,835 | 17,878 | 17,360 | 16,983 | 18,046 | 17,177 | 15,787 | 17,987 | 17,643 | 19,369 |
| North Carolina | 12,146 | 11,326 | 11,079 | 10,940 | 11,079 | 9,511 | 10,610 | 9,911 | 8,819 | 10,097 | 9,655 | 9,530 |
| North Dakota | 970 | 770 | 742 | 633 | 576 | 548 | 631 | 838 | 553 | 495 | 393 | 410 |
| Ohio | 18,466 | 16,823 | 17,282 | 17,601 | 17,255 | 15,239 | 16,863 | 16,229 | 14,217 | 16,242 | 14,712 | 15,278 |
| Oklahoma | 5,558 | 5,057 | 5,456 | 5,392 | 5,256 | 4,779 | 5,186 | 5,055 | 4,973 | 5,587 | 5,227 | 5,574 |
| Oregon | 2,329 | 1,925 | 2,073 | 2,201 | 2,029 | 1,672 | 1,646 | 1,768 | 1,354 | 1,469 | 1,544 | 1,551 |
| Pennsylvania | 19,100 | 17,406 | 16,841 | 17,294 | 16,401 | 15,426 | 16,677 | 14,169 | 12,866 | 14,900 | 13,724 | 15,694 |
| Rhode Island | 1,178 | 1,167 | 1,063 | 1,014 | 1,054 | 954 | 1,021 | 972 | 969 | 1,140 | 1,115 | 1,288 |
| South Carolina | 5,427 | 5,104 | 5,054 | 5,327 | 5,277 | 4,815 | 5,333 | 4,689 | 4,444 | 5,153 | 4,910 | 5,002 |
| South Dakota | 1,219 | 1,052 | 938 | 890 | 860 | 649 | 751 | 1,104 | 534 | 653 | 668 | 605 |
| Tennessee | 10,251 | 9,771 | 9,989 | 10,025 | 10,101 | 9,285 | 9,799 | 9,102 | 8,215 | 10,032 | 9,587 | 9,188 |
| Texas | 21,794 | 20,395 | 22,665 | 23,830 | 23,043 | 20,590 | 22,387 | 20,379 | 19,180 | 22,262 | 21,264 | 22,557 |
| Utah | 750 | 623 | 718 | 692 | 645 | 521 | 628 | 547 | 425 | 528 | 498 | 551 |
| Vermont | 719 | 774 | 632 | 629 | 601 | 618 | 568 | 615 | 458 | 499 | 549 | 548 |
| Virginia | 9,254 | 8,672 | 8,793 | 8,712 | 8,561 | 7,331 | 8,008 | 7,356 | 6,865 | 8,030 | 7,579 | 7,306 |
| Washington | 3,660 | 3,303 | 3,459 | 3,403 | 3,180 | 2,852 | 3,516 | 3,562 | 2,925 | 3,516 | 3,478 | 3,540 |
| West Virginia | 6,678 | 6,295 | 5,889 | 5,880 | 5,830 | 4,979 | 5,249 | 5,541 | 4,474 | 4,859 | 4,611 | 4,706 |
| Wisconsin | 6,064 | 5,573 | 5,353 | 5,143 | 4,747 | 4,290 | 4,441 | 4,548 | 3,639 | 4,088 | 3,828 | 3,735 |
| Wyoming | 760 | 578 | 567 | 540 | 504 | 412 | 492 | 568 | 494 | 588 | 526 | 440 |
| Total | 348,897 | 317,501 | 321,816 | 288,338 | 316,156 | 288,349 | 313,269 | 300,188 | 265,892 | 313,152 | 300,891 | 312,654 |
COPD includes ICD-9-CM codes 490-492 or 496. See Table 5 legend for expansion of abbreviation.
Table 14.
—Age-Adjusted Annual Rates for Medicare Hospitalizations With COPD as the First-Listed Discharge Diagnosis Among Medicare Beneficiaries Aged ≥ 65 Years, by State—United States, Medicare Part A Hospital Claims, 1999-2010
| Statea | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | P for Linear Trend |
| Alabama | 18.10 | 16.42 | 17.33 | 17.04 | 16.17 | 13.84 | 15.11 | 13.99 | 13.56 | 16.73 | 16.15 | 15.68 | .121 |
| Alaska | 12.62 | 12.31 | 12.26 | 10.89 | 10.60 | 9.05 | 8.01 | 9.85 | 6.59 | 7.76 | 6.88 | 7.49 | < .001 |
| Arizona | 9.88 | 7.97 | 7.61 | 7.63 | 7.14 | 6.64 | 7.83 | 6.89 | 6.05 | 8.01 | 7.66 | 8.62 | .541 |
| Arkansas | 16.14 | 14.84 | 14.70 | 14.67 | 13.44 | 11.53 | 12.54 | 13.02 | 10.70 | 11.67 | 11.36 | 11.53 | < .001 |
| California | 11.33 | 9.44 | 9.06 | 8.51 | 7.98 | 6.71 | 6.95 | 6.56 | 6.49 | 7.57 | 7.54 | 8.04 | .027 |
| Colorado | 11.93 | 9.22 | 8.96 | 8.35 | 8.17 | 6.79 | 7.71 | 8.01 | 6.44 | 8.27 | 6.80 | 7.49 | .015 |
| Connecticut | 8.52 | 8.21 | 8.02 | 7.70 | 7.56 | 7.41 | 8.01 | 7.81 | 7.90 | 9.55 | 9.30 | 9.48 | .057 |
| Delaware | 10.97 | 11.34 | 10.48 | 10.52 | 10.44 | 10.61 | 11.33 | 9.87 | 9.89 | 10.06 | 9.53 | 10.79 | .060 |
| District of Columbia | 8.17 | 8.00 | 7.60 | 7.21 | 6.87 | 6.11 | 7.89 | 6.66 | 6.22 | 8.33 | 7.41 | 8.08 | .736 |
| Florida | 13.32 | 11.69 | 11.77 | 11.52 | 10.65 | 10.57 | 10.88 | 10.58 | 9.88 | 12.02 | 12.15 | 12.55 | .747 |
| Georgia | 14.76 | 13.50 | 13.29 | 13.28 | 12.35 | 10.70 | 11.67 | 11.98 | 10.00 | 11.25 | 11.25 | 11.63 | .004 |
| Hawaii | 5.18 | 4.34 | 4.50 | 4.29 | 3.92 | 3.80 | 3.81 | 3.72 | 3.70 | 4.17 | 4.05 | 4.22 | .078 |
| Idaho | 9.87 | 7.81 | 7.57 | 6.93 | 6.23 | 4.72 | 5.13 | 6.50 | 4.28 | 4.65 | 4.78 | 4.62 | < .001 |
| Illinois | 13.49 | 11.91 | 11.91 | 11.72 | 10.89 | 9.88 | 10.79 | 10.94 | 9.95 | 12.53 | 11.94 | 11.71 | .439 |
| Indiana | 14.92 | 14.09 | 13.85 | 13.38 | 12.57 | 11.21 | 12.73 | 13.09 | 10.88 | 14.05 | 13.11 | 12.83 | .202 |
| Iowa | 12.18 | 10.46 | 10.28 | 9.04 | 8.16 | 7.26 | 7.24 | 9.54 | 6.31 | 7.18 | 6.65 | 6.91 | < .001 |
| Kansas | 11.95 | 10.41 | 10.21 | 9.91 | 9.93 | 8.29 | 9.21 | 10.81 | 7.53 | 8.54 | 7.67 | 7.57 | .001 |
| Kentucky | 23.83 | 21.10 | 21.76 | 21.07 | 20.58 | 17.87 | 19.67 | 20.45 | 16.93 | 20.80 | 20.34 | 19.77 | .080 |
| Louisiana | 16.95 | 15.23 | 15.38 | 15.02 | 14.35 | 12.03 | 13.93 | 12.43 | 11.12 | 13.62 | 13.23 | 13.52 | .015 |
| Maine | 13.60 | 14.05 | 11.48 | 10.28 | 10.05 | 8.83 | 9.44 | 10.31 | 7.65 | 8.75 | 9.67 | 9.03 | .005 |
| Maryland | 11.52 | 10.63 | 10.26 | 10.35 | 10.17 | 9.23 | 10.36 | 11.10 | 11.06 | 12.40 | 10.91 | 10.80 | .338 |
| Massachusetts | 13.15 | 12.28 | 11.53 | 11.28 | 10.85 | 10.14 | 10.95 | 10.66 | 10.31 | 12.72 | 12.30 | 12.93 | .908 |
| Michigan | 12.71 | 11.24 | 11.00 | 11.32 | 10.93 | 10.74 | 11.53 | 11.24 | 10.99 | 13.38 | 13.43 | 13.05 | .139 |
| Minnesota | 9.83 | 8.41 | 8.60 | 8.08 | 7.42 | 7.08 | 7.46 | 7.62 | 5.97 | 7.69 | 7.37 | 8.10 | .036 |
| Mississippi | 19.86 | 18.74 | 19.27 | 18.73 | 17.72 | 15.34 | 16.89 | 16.06 | 13.05 | 15.16 | 15.51 | 15.19 | < .001 |
| Missouri | 13.92 | 12.41 | 13.12 | 12.53 | 11.82 | 11.05 | 12.40 | 11.52 | 9.76 | 12.06 | 11.24 | 11.31 | .014 |
| Montana | 11.44 | 9.73 | 10.13 | 8.95 | 8.36 | 7.10 | 6.98 | 9.27 | 6.10 | 6.63 | 6.34 | 6.26 | < .001 |
| Nebraska | 9.92 | 7.90 | 7.11 | 6.66 | 6.64 | 5.54 | 7.32 | 9.32 | 6.38 | 8.14 | 7.26 | 8.09 | .882 |
| Nevada | 15.60 | 11.66 | 10.85 | 10.78 | 9.79 | 8.31 | 9.31 | 9.20 | 7.83 | 9.83 | 10.37 | 10.85 | .177 |
| New Hampshire | 10.37 | 10.12 | 9.35 | 8.84 | 8.83 | 9.41 | 8.40 | 10.25 | 8.42 | 10.01 | 9.48 | 9.08 | .504 |
| New Jersey | 11.69 | 10.45 | 10.42 | 10.73 | 11.02 | 10.40 | 11.34 | 10.56 | 10.11 | 11.55 | 11.13 | 11.36 | .576 |
| New Mexico | 10.62 | 8.60 | 8.26 | 8.52 | 8.10 | 6.73 | 8.29 | 7.24 | 6.59 | 7.89 | 7.68 | 8.09 | .071 |
| New York | 11.64 | 10.52 | 9.94 | 9.92 | 9.64 | 9.09 | 9.79 | 9.62 | 9.05 | 10.52 | 10.46 | 11.56 | .933 |
| North Carolina | 13.92 | 12.78 | 12.33 | 12.02 | 11.91 | 10.11 | 11.22 | 10.76 | 9.75 | 11.07 | 10.49 | 10.08 | < .001 |
| North Dakota | 10.51 | 8.34 | 8.04 | 6.91 | 6.27 | 5.98 | 6.88 | 9.44 | 6.31 | 5.72 | 4.53 | 4.71 | .003 |
| Ohio | 15.65 | 14.13 | 14.11 | 14.24 | 13.77 | 12.06 | 13.36 | 13.13 | 11.71 | 14.78 | 13.59 | 15.60 | .494 |
| Oklahoma | 14.40 | 13.13 | 14.07 | 13.60 | 13.09 | 11.83 | 12.79 | 12.95 | 12.46 | 14.01 | 13.03 | 13.77 | .524 |
| Oregon | 9.23 | 7.52 | 7.83 | 8.11 | 7.33 | 5.89 | 5.72 | 6.38 | 4.99 | 5.34 | 5.67 | 5.52 | < .001 |
| Pennsylvania | 14.25 | 13.18 | 12.16 | 12.41 | 11.86 | 11.21 | 12.28 | 11.15 | 10.46 | 12.82 | 12.00 | 13.65 | .289 |
| Rhode Island | 12.72 | 12.46 | 11.56 | 10.93 | 11.66 | 10.60 | 11.63 | 11.13 | 11.26 | 13.29 | 13.03 | 14.62 | .223 |
| South Carolina | 12.28 | 11.30 | 10.98 | 11.38 | 11.06 | 9.88 | 10.73 | 9.62 | 9.24 | 10.73 | 10.11 | 10.04 | .008 |
| South Dakota | 11.49 | 9.86 | 8.81 | 8.39 | 7.92 | 5.94 | 6.84 | 10.06 | 5.04 | 6.28 | 6.19 | 5.55 | .004 |
| Tennessee | 16.34 | 15.49 | 15.54 | 15.68 | 15.75 | 14.43 | 15.28 | 14.82 | 13.66 | 16.73 | 15.82 | 15.12 | .442 |
| Texas | 13.94 | 12.81 | 13.11 | 13.11 | 12.29 | 10.82 | 11.68 | 10.79 | 10.23 | 11.87 | 11.23 | 11.69 | .009 |
| Utah | 4.44 | 3.60 | 4.07 | 3.85 | 3.50 | 2.76 | 3.31 | 3.22 | 2.61 | 3.37 | 3.29 | 3.62 | .073 |
| Vermont | 9.92 | 10.33 | 8.37 | 8.24 | 7.79 | 7.89 | 7.18 | 7.62 | 5.65 | 6.08 | 6.61 | 6.48 | < .001 |
| Virginia | 13.44 | 12.15 | 11.90 | 11.62 | 11.20 | 9.44 | 10.13 | 9.54 | 8.98 | 10.47 | 9.82 | 9.27 | < .001 |
| Washington | 8.19 | 7.13 | 6.96 | 6.51 | 5.93 | 5.14 | 6.19 | 6.26 | 5.16 | 6.20 | 6.13 | 6.09 | .065 |
| West Virginia | 27.38 | 25.81 | 24.10 | 23.95 | 23.62 | 20.11 | 21.06 | 22.62 | 21.20 | 23.50 | 22.52 | 22.50 | .033 |
| Wisconsin | 9.32 | 8.56 | 8.16 | 7.60 | 7.04 | 6.43 | 6.84 | 7.54 | 6.35 | 7.41 | 7.20 | 7.12 | .022 |
| Wyoming | 14.19 | 10.65 | 10.22 | 9.67 | 8.83 | 7.12 | 8.31 | 9.66 | 8.28 | 9.72 | 8.58 | 7.02 | .023 |
| Totala | 13.28 | 11.91 | 11.71 | 11.49 | 10.97 | 9.88 | 10.71 | 10.55 | 9.50 | 11.31 | 10.87 | 11.18 | .045 |
Annual rate per 1,000 Medicare enrollees aged ≥ 65 y, alive, entitled to Medicare Part A, and not in a managed care plan on July 1 of the given year. COPD includes ICD-9-CM codes 490-492 or 496. See Table 5 legend for expansion of abbreviation.
Age-adjusted to the 2000 US standard population aged ≥ 65 y.
Figure 7.
Age-adjusted rates (per 1,000 Medicare enrollees) of Medicare hospitalizations for COPD as the first-listed discharge diagnosis among Medicare enrollees aged ≥ 65 years—United States, Medicare Part A hospital claims, 1999-2000 and 2009-2010.
Figure 8.
Significant linear change (P < .05) in state-specific age-adjusted rates (per 1,000 Medicare enrollees) of Medicare hospitalizations for COPD as the first-listed discharge diagnosis among Medicare enrollees aged ≥ 65 years—United States, Medicare Part A hospital claims, 1999-2010.
Deaths (Death Certificates)
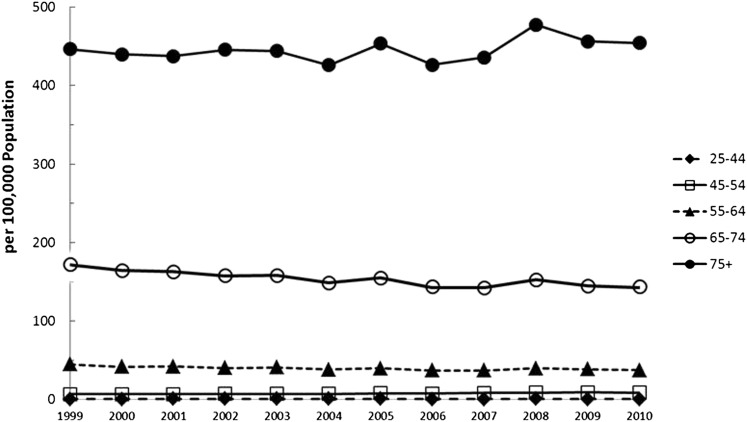
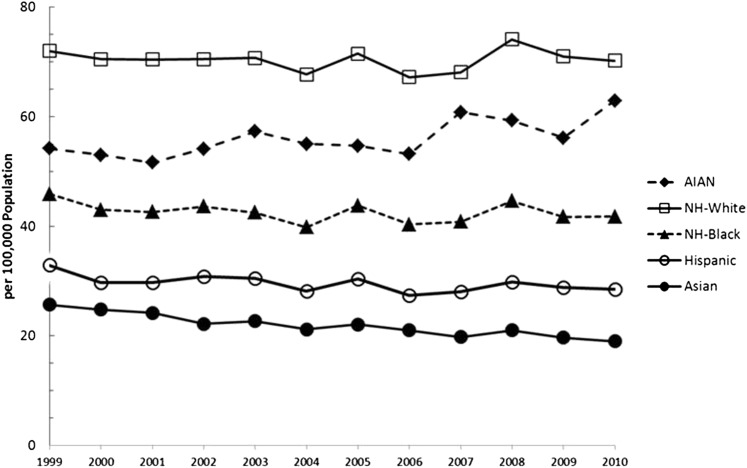
In 2010, there were 133,575 deaths (crude rate, 65.5 per 100,000 US population; age-adjusted rate, 63.1 per 100,000 population) among adults aged ≥ 25 years. Although the annual number of deaths increased somewhat during 1999 to 2010 (Table 15), the age-adjusted death rate for COPD declined during 1999 to 2010 among men (P = .001) but did not change significantly in women (P = .127) or overall (P = .163) (Table 16). Age-specific rates increased among adults aged 45 to 54 years (P < .001) but declined among those aged 55 to 64 years (P = .002) and 65 to 74 years (P < .001). The age-specific rates each year were highest among those aged ≥ 75 years and 65 to 74 years (Fig 9). Age-adjusted rates were highest among non-Hispanic whites followed by American Indian/Alaska Natives, non-Hispanic blacks, Hispanics, and Asian/Pacific Islanders (Fig 10). During 1999 to 2010, age-adjusted rates increased among American Indian/Alaska Natives (P = .008) and declined among Hispanics (P = .038) and Asian/Pacific Islanders (P < .001) but did not change significantly among non-Hispanic whites or non-Hispanic blacks.
Table 15.
—Annual Number of Adults Aged ≥ 25 Years With COPD as the Underlying Cause of Death, by Race, Sex, and Age Group—United States, Mortality Component of the National Vital Statistics System, 1999-2010
| Variable | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 |
| Race/ethnicitya | ||||||||||||
| White, non-Hispanic | 107,706 | 106,198 | 107,145 | 108,481 | 110,088 | 106,393 | 113,939 | 108,435 | 111,477 | 123,171 | 119,715 | 119,894 |
| Black, non-Hispanic | 6,640 | 6,327 | 6,355 | 6,585 | 6,565 | 6,274 | 7,086 | 6,660 | 6,896 | 7,743 | 7,489 | 7,700 |
| Hispanic | 2,488 | 2,341 | 2,512 | 2,724 | 2,827 | 2,779 | 3,166 | 2,994 | 3,238 | 3,623 | 3,672 | 3,817 |
| AIAN | 360 | 381 | 378 | 413 | 455 | 457 | 467 | 468 | 559 | 579 | 555 | 643 |
| API | 923 | 925 | 985 | 969 | 1,037 | 1,013 | 1,136 | 1,144 | 1,146 | 1,288 | 1,265 | 1,265 |
| Sex | ||||||||||||
| Women | 58,040 | 58,436 | 59,789 | 60,673 | 62,363 | 60,194 | 65,193 | 62,290 | 63,813 | 71,031 | 69,334 | 69,797 |
| Men | 60,416 | 58,058 | 57,908 | 58,807 | 58,904 | 56,940 | 60,812 | 57,633 | 59,678 | 65,606 | 63,583 | 63,778 |
| Age group, y | ||||||||||||
| 25-44 | 494 | 500 | 554 | 586 | 573 | 554 | 558 | 519 | 521 | 566 | 506 | 453 |
| 45-54 | 2,472 | 2,618 | 2,695 | 2,842 | 2,883 | 2,920 | 3,356 | 3,326 | 3,596 | 3869 | 4,083 | 3,861 |
| 55-64 | 10,643 | 10,130 | 10,545 | 10,670 | 11,451 | 11,183 | 12,173 | 11,823 | 12,273 | 13518 | 13,636 | 13,674 |
| 65-74 | 31,699 | 30,249 | 29,942 | 29,040 | 29,241 | 27,740 | 29,296 | 27,640 | 28,100 | 31390 | 30,762 | 31,254 |
| ≥ 75 | 73,148 | 72,997 | 73,961 | 76,342 | 77,119 | 74,737 | 80,622 | 76,615 | 79,001 | 87,294 | 83,930 | 84,333 |
| Total | 118,456 | 116,494 | 117,697 | 119,480 | 121,267 | 117,134 | 126,005 | 119,923 | 123,491 | 136,637 | 132,917 | 133,575 |
COPD includes ICD-10 codes J40–J44 from the WHO. AIAN = non-Hispanic American Indian/Alaska Natives; API = non-Hispanic Asian/Pacific Islanders; ICD-10 = International Classification of Diseases, tenth revision; WHO = World Health Organization.
A summation of the annual numbers will not equal the total annual number because of small numbers of death in other race/ethnicity or unknown categories.
Table 16.
—Annual Rates for Deaths With COPD as the Underlying Cause Of Death Among Adults Aged ≥ 25 Years, by Race, Sex, and Age Group—United States, Mortality Component of the National Vital Statistics System, 1999-2010
| Variable | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | P for Linear Trend |
| Race/ethnicitya | |||||||||||||
| White, non-Hispanic | 72.0 | 70.5 | 70.4 | 70.5 | 70.7 | 67.7 | 71.5 | 67.2 | 68.1 | 74.1 | 71.0 | 70.2 | .870 |
| Black, non-Hispanic | 45.9 | 43.0 | 42.6 | 43.6 | 42.5 | 39.8 | 43.8 | 40.3 | 40.8 | 44.6 | 41.7 | 41.8 | .240 |
| Hispanic | 32.9 | 29.7 | 29.7 | 30.8 | 30.5 | 28.2 | 30.4 | 27.4 | 28.1 | 29.8 | 28.8 | 28.5 | .038 |
| AIAN | 54.2 | 53.0 | 51.6 | 54.1 | 57.3 | 55.0 | 54.7 | 53.2 | 60.8 | 59.3 | 56.1 | 62.9 | .008 |
| API | 25.7 | 24.8 | 24.2 | 22.2 | 22.7 | 21.2 | 22.1 | 21.0 | 19.8 | 21.0 | 19.7 | 19.0 | < .001 |
| Sexd | |||||||||||||
| Women | 54.6 | 54.4 | 54.9 | 55.0 | 55.9 | 53.3 | 56.8 | 53.6 | 54.0 | 59.1 | 56.8 | 56.3 | .127 |
| Men | 88.2 | 83.8 | 81.8 | 81.7 | 79.9 | 75.7 | 78.8 | 73.0 | 73.7 | 79.2 | 74.8 | 73.6 | .001 |
| Age group, y | |||||||||||||
| 25-44 | 0.6 | 0.6 | 0.7 | 0.7 | 0.7 | 0.7 | 0.7 | 0.6 | 0.6 | 0.7 | 0.6 | 0.6 | … |
| 45-54 | 6.8 | 6.9 | 6.8 | 7.1 | 7.1 | 7.0 | 7.9 | 7.7 | 8.2 | 8.7 | 9.1 | 8.6 | < .001 |
| 55-64 | 44.8 | 41.7 | 42.0 | 40.0 | 40.9 | 38.2 | 39.7 | 37.0 | 37.0 | 39.6 | 38.5 | 37.5 | .002 |
| 65-74 | 172.1 | 164.5 | 162.9 | 157.9 | 158.1 | 148.6 | 155.2 | 143.9 | 142.6 | 153.1 | 144.9 | 143.9 | < .001 |
| ≥ 75 | 446.6 | 439.7 | 437.5 | 445.6 | 444.2 | 426.2 | 453.7 | 426.6 | 435.8 | 477.7 | 456.4 | 454.5 | .212 |
| Totala | 67.0 | 65.2 | 64.9 | 65.0 | 64.9 | 61.8 | 65.3 | 61.1 | 61.7 | 66.9 | 63.8 | 63.1 | .163 |
| Totalb | 65.7 | 64.0 | 63.9 | 64.2 | 64.5 | 61.6 | 65.4 | 61.5 | 62.6 | 68.4 | 65.8 | 65.5 | .515 |
Annual rate per 100,000 US population. COPD includes ICD-10 codes J40–J44 from the WHO. Death rates for 2001-2009 will differ from previous reports because 2001-2009 population denominators have been revised In CDC Wonder (Oct 2012). See Table 15 legend for expansion of abbreviations.
Age-adjusted to the 2000 US standard population aged ≥ 25 y.
Unadjusted rate.
Figure 9.
Age-specific death rates (per 100,000) for COPD as the underlying cause of death among adults aged ≥ 25 years, by year—United States, Mortality Component of the National Vital Statistics System, 1999-2010.
Figure 10.
Race-specific age-adjusted death rates (per 100,000) for COPD as the underlying cause of death among adults aged ≥ 25 years, by year—United States, Mortality Component of the National Vital Statistics System, 1999-2010.
Numbers of deaths (Table 17) and age-adjusted death rates varied during 1999 to 2010 in most states (Table 18). Figure 11 compares aggregated age-adjusted state-specific death rates for COPD in 1999 to 2000 to those for 2009 to 2010. In 1999 to 2000, states with the highest death rates (75.0-103.9 per 100,000) were along the Ohio River valley and in multiple western states. Geographic clustering of COPD death rates aggregated for 2009 to 2010 was observed in states along the Ohio River Valley and in several western states and also in several southern states (Fig 11). Although death rates for COPD declined in many states during 1999 to 2010, five states (Alabama, Mississippi, Arkansas, Oklahoma, and South Dakota) experienced significant increases in deaths from COPD (Fig 12).
Table 17.
—Annual Number of Adults Aged ≥ 25 Years With COPD as the Underlying Cause of Death, by State—United States, Mortality Component of the National Vital Statistics System, 1999-2010
| State | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 |
| Alabama | 2,095 | 1,964 | 2,125 | 2,245 | 2,347 | 2,256 | 2,318 | 2,239 | 2,463 | 2,655 | 2,693 | 2,784 |
| Alaska | 133 | 125 | 134 | 132 | 132 | 128 | 145 | 129 | 164 | 176 | 187 | 165 |
| Arizona | 2,414 | 2,410 | 2,382 | 2,462 | 2,448 | 2,328 | 2,723 | 2,695 | 2,605 | 2,860 | 2,773 | 2,836 |
| Arkansas | 1,296 | 1,328 | 1,297 | 1,383 | 1,439 | 1,375 | 1,508 | 1437 | 1,587 | 1,833 | 1,772 | 1,732 |
| California | 12,488 | 12,092 | 12,356 | 12,088 | 12,833 | 11,971 | 12,608 | 12,223 | 11,995 | 12,870 | 12,393 | 12,455 |
| Colorado | 1,791 | 1,715 | 1,762 | 1,773 | 1,864 | 1,823 | 1,864 | 1,873 | 1,948 | 2,128 | 2,012 | 2,143 |
| Connecticut | 1,366 | 1,469 | 1,429 | 1,385 | 1,395 | 1,375 | 1,421 | 1,400 | 1,310 | 1,461 | 1,389 | 1,237 |
| Delaware | 316 | 322 | 286 | 335 | 333 | 334 | 398 | 338 | 370 | 460 | 421 | 427 |
| District of Columbia | 150 | 160 | 138 | 125 | 126 | 144 | 123 | 114 | 122 | 133 | 127 | 139 |
| Florida | 8,815 | 8,345 | 8,621 | 8,738 | 8,778 | 8,703 | 9,173 | 8,668 | 9,092 | 9,957 | 9,891 | 10,076 |
| Georgia | 2,903 | 2,914 | 2,950 | 3,032 | 3,105 | 2,980 | 3,262 | 3,241 | 3,269 | 3,426 | 3,615 | 3,694 |
| Hawaii | 250 | 233 | 243 | 234 | 249 | 270 | 260 | 258 | 260 | 266 | 269 | 265 |
| Idaho | 542 | 549 | 562 | 574 | 575 | 544 | 691 | 624 | 639 | 682 | 699 | 701 |
| Illinois | 4,851 | 4,486 | 4,499 | 4,539 | 4,601 | 4,493 | 4,817 | 4,521 | 4,552 | 5,384 | 5,093 | 4,998 |
| Indiana | 2,915 | 2,948 | 3,053 | 3,032 | 3,167 | 3,030 | 3,365 | 3,193 | 3,130 | 3,768 | 3,649 | 3,697 |
| Iowa | 1,574 | 1,454 | 1,482 | 1,521 | 1,620 | 1,492 | 1,650 | 1,603 | 1,605 | 1,803 | 1,777 | 1,633 |
| Kansas | 1,323 | 1,351 | 1,393 | 1,328 | 1,407 | 1,272 | 1,529 | 1,447 | 1,437 | 1,581 | 1,537 | 1,532 |
| Kentucky | 2,260 | 2,090 | 2,204 | 2,339 | 2,327 | 2,202 | 2,507 | 2,331 | 2,577 | 2,874 | 2,791 | 2,721 |
| Louisiana | 1,525 | 1,591 | 1,684 | 1,598 | 1,660 | 1,547 | 1,830 | 1,630 | 1,633 | 1,831 | 1,826 | 1,895 |
| Maine | 730 | 755 | 773 | 769 | 762 | 744 | 813 | 763 | 717 | 774 | 801 | 788 |
| Maryland | 1,836 | 1,828 | 1,813 | 1,838 | 1,887 | 1,808 | 1,823 | 1,761 | 1,813 | 1,916 | 1,980 | 1,955 |
| Massachusetts | 2,729 | 2,799 | 2,699 | 2,630 | 2,668 | 2,466 | 2,529 | 2,457 | 2,260 | 2,510 | 2,481 | 2,306 |
| Michigan | 4,130 | 4,150 | 3,974 | 4,251 | 4,316 | 4,099 | 4,304 | 4,334 | 4,466 | 5,050 | 4,814 | 4,943 |
| Minnesota | 1,880 | 1,794 | 1,816 | 1,864 | 1,742 | 1,762 | 1,883 | 1,706 | 1,686 | 2,023 | 1,879 | 1,923 |
| Mississippi | 1,217 | 1,189 | 1,275 | 1,320 | 1,352 | 1,295 | 1,416 | 1,324 | 1,363 | 1,464 | 1,505 | 1,602 |
| Missouri | 2,949 | 2,692 | 2,781 | 2,765 | 2,836 | 2,628 | 3,002 | 2,922 | 2,990 | 3,663 | 3,354 | 3,453 |
| Montana | 538 | 499 | 559 | 554 | 568 | 563 | 569 | 561 | 595 | 681 | 588 | 586 |
| Nebraska | 893 | 794 | 831 | 885 | 851 | 774 | 897 | 845 | 882 | 1,009 | 945 | 976 |
| Nevada | 987 | 959 | 1,108 | 1,149 | 1,155 | 1,097 | 1,209 | 1,046 | 1,027 | 1,233 | 1,215 | 1,155 |
| New Hampshire | 578 | 560 | 596 | 553 | 509 | 581 | 611 | 589 | 593 | 676 | 640 | 594 |
| New Jersey | 2,993 | 2,874 | 2,761 | 2,737 | 2,775 | 2,895 | 3,009 | 2,732 | 2,881 | 3,159 | 3,010 | 2,998 |
| New Mexico | 810 | 725 | 734 | 815 | 893 | 722 | 824 | 857 | 852 | 973 | 955 | 996 |
| New York | 6,653 | 6,419 | 6,514 | 6,581 | 6,336 | 6,430 | 6,472 | 6,047 | 6,281 | 6,619 | 6,440 | 6,509 |
| North Carolina | 3,412 | 3,533 | 3,343 | 3,531 | 3,725 | 3,474 | 4,005 | 3,858 | 4,071 | 4,413 | 4,196 | 4,357 |
| North Dakota | 256 | 280 | 298 | 306 | 284 | 260 | 260 | 274 | 255 | 341 | 330 | 341 |
| Ohio | 5,656 | 5,773 | 5,686 | 5,840 | 5,739 | 5,727 | 6,406 | 5,871 | 6,263 | 6,771 | 6,479 | 6,520 |
| Oklahoma | 1,683 | 1,906 | 1,853 | 1,920 | 2,093 | 1,923 | 2,296 | 2,133 | 2,333 | 2,645 | 2,539 | 2,679 |
| Oregon | 1,664 | 1,599 | 1,646 | 1,754 | 1,738 | 1,711 | 1,767 | 1,730 | 1,816 | 1,868 | 1,847 | 1,888 |
| Pennsylvania | 5,922 | 5,837 | 5,646 | 5,797 | 5,816 | 5,774 | 5,935 | 5,420 | 5,871 | 6,531 | 6,254 | 6,025 |
| Rhode Island | 478 | 493 | 494 | 509 | 474 | 447 | 502 | 467 | 406 | 462 | 500 | 498 |
| South Carolina | 1,675 | 1,645 | 1,640 | 1,805 | 1,819 | 1,699 | 1,879 | 1,854 | 1,949 | 2,176 | 2,245 | 2,175 |
| South Dakota | 315 | 364 | 335 | 364 | 365 | 375 | 424 | 363 | 437 | 474 | 431 | 430 |
| Tennessee | 2,655 | 2,765 | 2,826 | 2,874 | 2,939 | 2,885 | 3,076 | 2,875 | 3,064 | 3,462 | 3,408 | 3,460 |
| Texas | 7,139 | 6,960 | 7,404 | 7,400 | 7,264 | 7,110 | 7,666 | 7,334 | 7,814 | 8,605 | 8,365 | 8,667 |
| Utah | 523 | 482 | 483 | 555 | 525 | 549 | 559 | 548 | 589 | 604 | 547 | 637 |
| Vermont | 288 | 295 | 298 | 267 | 295 | 286 | 370 | 308 | 307 | 330 | 353 | 322 |
| Virginia | 2,549 | 2,667 | 2,607 | 2,620 | 2,840 | 2,607 | 2,770 | 2,592 | 2,656 | 2,899 | 2,901 | 2,865 |
| Washington | 2,604 | 2,533 | 2,520 | 2,604 | 2,545 | 2,448 | 2,591 | 2,553 | 2,597 | 2,832 | 2,835 | 2,634 |
| West Virginia | 1,208 | 1,300 | 1,242 | 1,195 | 1,257 | 1,207 | 1,315 | 1,233 | 1,289 | 1,567 | 1,462 | 1,455 |
| Wisconsin | 2,172 | 2,202 | 2,286 | 2,246 | 2,223 | 2,220 | 2,352 | 2,273 | 2,325 | 2,455 | 2,397 | 2,384 |
| Wyoming | 327 | 277 | 256 | 319 | 270 | 301 | 279 | 329 | 285 | 304 | 307 | 324 |
| Total | 118,456 | 116,494 | 117,697 | 119,480 | 121,267 | 117,134 | 126,005 | 119,923 | 123,491 | 136,637 | 132,917 | 133,575 |
COPD includes ICD-10 Codes J40–J44 from the WHO. See Table 15 legend for expansion of abbreviations.
Table 18.
—Age-Adjusted Annual Rates for Deaths With COPD as the Underlying Cause of Death Among Adults Aged ≥ 25 Years, by State—United States, Mortality Component of the National Vital Statistics System, 1999-2010
| Statea | 1999 | 2000 | 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | P for Linear Trend |
| Alabama | 72.2 | 67.1 | 72.0 | 75.5 | 78.1 | 74.2 | 75.4 | 71.3 | 77.2 | 81.4 | 81.5 | 83.2 | .002 |
| Alaska | 81.1 | 71.0 | 74.3 | 69.2 | 67.0 | 57.7 | 62.3 | 55.2 | 67.6 | 67.2 | 73.6 | 60.6 | .202 |
| Arizona | 74.9 | 73.2 | 70.3 | 71.4 | 68.9 | 63.8 | 71.6 | 68.5 | 64.4 | 68.5 | 64.5 | 64.5 | .003 |
| Arkansas | 68.9 | 70.0 | 68.0 | 72.0 | 74.3 | 70.3 | 76.3 | 71.2 | 77.8 | 88.1 | 83.9 | 80.8 | .001 |
| California | 68.9 | 65.6 | 65.5 | 63.0 | 65.4 | 60.2 | 61.9 | 59.2 | 56.8 | 59.3 | 55.7 | 54.9 | < .001 |
| Colorado | 85.4 | 80.4 | 80.3 | 78.9 | 80.8 | 77.0 | 76.8 | 74.1 | 74.4 | 79.1 | 71.8 | 75.0 | .002 |
| Connecticut | 55.5 | 59.3 | 56.7 | 54.3 | 53.8 | 52.5 | 53.7 | 51.9 | 48.3 | 53.0 | 49.6 | 43.6 | < .001 |
| Delaware | 63.8 | 64.3 | 55.4 | 64.0 | 61.6 | 60.4 | 70.0 | 57.5 | 61.0 | 73.5 | 65.9 | 65.8 | .236 |
| District of Columbia | 41.7 | 44.2 | 38.3 | 34.5 | 35.1 | 40.3 | 34.7 | 32.4 | 34.2 | 37.4 | 35.2 | 37.7 | .099 |
| Florida | 64.0 | 60.0 | 61.1 | 60.7 | 60.1 | 58.4 | 60.3 | 56.3 | 57.8 | 61.9 | 60.3 | 60.3 | .338 |
| Georgia | 72.5 | 72.0 | 71.4 | 71.6 | 72.3 | 67.7 | 71.9 | 68.8 | 67.7 | 68.1 | 70.1 | 70.0 | .030 |
| Hawaii | 31.9 | 29.0 | 29.4 | 27.4 | 28.4 | 29.9 | 27.7 | 27.1 | 26.7 | 27.0 | 26.1 | 24.8 | < .001 |
| Idaho | 73.1 | 72.9 | 72.7 | 72.7 | 70.9 | 65.6 | 80.6 | 70.4 | 69.9 | 72.4 | 71.8 | 70.1 | .597 |
| Illinois | 63.0 | 57.9 | 57.6 | 57.6 | 57.9 | 56.1 | 59.4 | 55.3 | 55.0 | 64.2 | 59.9 | 58.2 | .908 |
| Indiana | 76.2 | 76.6 | 78.4 | 77.0 | 79.2 | 75.1 | 82.1 | 76.6 | 73.9 | 87.2 | 83.6 | 83.3 | .060 |
| Iowa | 69.3 | 63.6 | 64.2 | 66.0 | 69.6 | 63.6 | 70.3 | 67.6 | 66.4 | 74.3 | 73.0 | 66.2 | .157 |
| Kansas | 71.8 | 72.6 | 74.7 | 70.8 | 74.6 | 67.1 | 79.4 | 74.4 | 73.1 | 79.4 | 76.0 | 75.0 | .155 |
| Kentucky | 88.6 | 81.5 | 85.2 | 89.4 | 87.9 | 82.3 | 91.6 | 83.3 | 90.7 | 99.0 | 94.1 | 90.7 | .050 |
| Louisiana | 59.0 | 61.0 | 63.9 | 60.1 | 61.4 | 56.9 | 66.3 | 61.0 | 60.1 | 65.8 | 64.1 | 65.9 | .072 |
| Maine | 79.0 | 80.5 | 81.1 | 79.5 | 77.2 | 74.5 | 80.5 | 73.9 | 67.7 | 72.0 | 73.3 | 71.3 | .002 |
| Maryland | 61.0 | 60.1 | 58.2 | 57.9 | 58.2 | 54.8 | 54.0 | 51.3 | 52.0 | 53.5 | 53.8 | 52.0 | < .001 |
| Massachusetts | 61.3 | 62.3 | 59.6 | 57.6 | 58.0 | 53.2 | 54.0 | 52.1 | 47.4 | 51.8 | 50.6 | 46.5 | < .001 |
| Michigan | 67.0 | 66.8 | 63.1 | 66.5 | 66.5 | 62.3 | 64.6 | 64.1 | 64.8 | 72.0 | 67.4 | 68.6 | .271 |
| Minnesota | 60.2 | 56.9 | 57.1 | 57.4 | 52.8 | 52.9 | 55.6 | 49.6 | 48.3 | 56.5 | 51.6 | 51.9 | .015 |
| Mississippi | 70.1 | 68.1 | 72.6 | 74.7 | 76.1 | 71.8 | 77.4 | 71.9 | 73.0 | 76.7 | 78.7 | 82.3 | .004 |
| Missouri | 76.7 | 69.7 | 71.2 | 70.2 | 71.4 | 65.5 | 74.0 | 70.9 | 71.3 | 86.3 | 77.8 | 78.8 | .097 |
| Montana | 87.3 | 80.0 | 87.9 | 85.9 | 86.9 | 84.1 | 83.1 | 79.9 | 83.2 | 92.9 | 78.5 | 77.2 | .218 |
| Nebraska | 73.8 | 66.1 | 67.8 | 71.8 | 69.2 | 62.0 | 71.3 | 66.0 | 68.2 | 76.9 | 71.5 | 73.1 | .389 |
| Nevada | 96.5 | 92.1 | 99.2 | 100.0 | 95.9 | 86.7 | 92.2 | 76.5 | 74.0 | 85.7 | 80.6 | 74.9 | .001 |
| New Hampshire | 77.0 | 73.6 | 77.0 | 70.3 | 63.4 | 69.9 | 72.3 | 67.7 | 66.4 | 74.2 | 69.2 | 62.9 | .053 |
| New Jersey | 53.0 | 50.4 | 47.9 | 46.9 | 47.1 | 48.7 | 50.1 | 44.9 | 46.7 | 50.4 | 47.3 | 46.8 | .186 |
| New Mexico | 78.2 | 68.6 | 67.3 | 73.1 | 78.8 | 62.2 | 68.8 | 69.4 | 67.3 | 74.7 | 70.7 | 71.8 | .816 |
| New York | 53.6 | 51.0 | 51.1 | 50.9 | 48.5 | 48.8 | 48.6 | 45.1 | 46.3 | 48.1 | 46.4 | 46.2 | < .001 |
| North Carolina | 70.6 | 72.3 | 67.1 | 69.3 | 71.5 | 65.1 | 73.4 | 68.0 | 69.8 | 73.5 | 68.0 | 69.1 | .897 |
| North Dakota | 51.9 | 56.6 | 59.1 | 61.4 | 56.5 | 51.1 | 50.8 | 51.7 | 48.7 | 64.3 | 62.2 | 63.8 | .383 |
| Ohio | 74.4 | 75.5 | 73.7 | 74.8 | 72.6 | 71.8 | 79.4 | 71.8 | 75.5 | 80.5 | 75.9 | 75.7 | .291 |
| Oklahoma | 73.2 | 82.2 | 79.5 | 81.7 | 88.4 | 80.7 | 95.3 | 86.6 | 93.8 | 104.4 | 98.3 | 102.6 | < .001 |
| Oregon | 73.5 | 70.0 | 70.7 | 73.8 | 71.7 | 69.5 | 70.0 | 66.8 | 68.4 | 68.9 | 66.6 | 67.1 | .001 |
| Pennsylvania | 61.1 | 59.7 | 57.4 | 58.5 | 58.1 | 57.6 | 58.5 | 52.9 | 56.7 | 62.4 | 59.4 | 56.8 | .463 |
| Rhode Island | 60.5 | 61.5 | 61.7 | 62.6 | 57.5 | 54.2 | 60.2 | 56.8 | 48.4 | 55.8 | 60.2 | 58.4 | .147 |
| South Carolina | 69.5 | 67.4 | 65.7 | 71.2 | 69.7 | 63.7 | 68.6 | 65.2 | 66.5 | 72.0 | 72.2 | 68.6 | .478 |
| South Dakota | 55.9 | 64.0 | 59.5 | 63.6 | 63.7 | 63.5 | 71.5 | 59.8 | 70.9 | 75.5 | 68.0 | 67.8 | .012 |
| Tennessee | 74.6 | 77.1 | 77.6 | 77.8 | 78.3 | 75.7 | 79.0 | 71.7 | 74.8 | 82.6 | 79.5 | 79.3 | .298 |
| Texas | 69.0 | 66.3 | 69.2 | 68.0 | 65.2 | 62.5 | 65.6 | 60.8 | 63.1 | 67.8 | 63.8 | 64.8 | .105 |
| Utah | 54.4 | 49.4 | 48.2 | 54.3 | 50.1 | 50.8 | 50.3 | 47.3 | 49.0 | 48.9 | 43.1 | 48.8 | .031 |
| Vermont | 73.2 | 73.9 | 73.3 | 64.4 | 70.0 | 67.1 | 85.7 | 69.2 | 67.5 | 71.2 | 74.0 | 67.3 | .729 |
| Virginia | 64.2 | 66.2 | 63.5 | 62.3 | 66.5 | 59.8 | 61.9 | 56.5 | 56.8 | 60.3 | 59.0 | 56.9 | .002 |
| Washington | 76.2 | 73.1 | 71.2 | 72.1 | 69.2 | 65.1 | 67.4 | 64.6 | 64.1 | 68.1 | 66.4 | 60.3 | < .001 |
| West Virginia | 87.4 | 93.8 | 89.3 | 85.1 | 88.5 | 84.6 | 91.1 | 84.6 | 87.0 | 104.9 | 96.8 | 95.1 | .138 |
| Wisconsin | 59.8 | 60.3 | 61.8 | 59.8 | 58.5 | 57.8 | 60.4 | 57.5 | 57.8 | 59.7 | 58.0 | 56.5 | .019 |
| Wyoming | 113.4 | 94.6 | 85.1 | 104.6 | 86.7 | 94.8 | 85.4 | 99.4 | 84.6 | 88.4 | 87.8 | 89.6 | .119 |
| Totala | 67.0 | 65.2 | 64.9 | 65.0 | 64.9 | 61.8 | 65.3 | 61.1 | 61.7 | 66.9 | 63.8 | 63.1 | .163 |
Annual rate per 100,000 US population. COPD includes ICD-10 codes J40–J44 from the WHO. Death rates for 2001-2009 will differ from previous reports because 2001-2009 population denominators have been revised in CDC Wonder (Oct 2012). See Table 15 legend for expansion of abbreviations.
Age-adjusted to the 2000 US population aged ≥ 25 y.
Figure 11.
Age-adjusted state-specific death rates (per 100,000) for COPD as the underlying cause of death among adults aged ≥ 25 years, by state—United States, Mortality Component of the National Vital Statistics System, 1999-2000 and 2009-2010.
Figure 12.
Significant linear change (P < .05) in state-specific age-adjusted death rates for COPD as the underlying cause of death among adults aged ≥ 25 years, by state—United States, Mortality Component of the National Vital Statistics System, 1999-2010.
Discussion
The previous COPD surveillance report noted that rates of hospitalizations and mortality for COPD had increased from 1980 to 2000.13 However, the mortality rate in men and some age groups and hospitalization rates in both men and women have declined since 1999. Rates of physician-based office visits and ED visits for COPD from 1999 to 2010 demonstrated substantial interyear variability and showed no particular trend; however, it is encouraging that there were no increases in office visit rates or ED rates for COPD.
Because smoking is the most important etiologic driver of COPD,22 trends in the prevalence of smoking impacted many of the metrics examined in this surveillance report, although the exact temporal relationship between changes in the smoking prevalence and changes in health-care use and mortality for COPD are not well defined. Since 1965, the prevalence of smoking has decreased considerably. In 1965, 42.4% (unadjusted percentage) of adults aged ≥ 18 years were current smokers compared with 19.3% in 2010.23 The crude prevalence of smoking in 2010 was one-half that in 1965 for both men (21.5% vs 51.9%, respectively) and women (17.3% vs 33.9%, respectively). In 1999 to 2001, American Indian/Alaska Native adults had a higher age-adjusted prevalence of current smoking (30.3% in men and 34.7% in women) compared with white adults (25.1% in men and 22.2% in women),23 which may explain the increase in COPD mortality during 1999 to 2010 in that population. The prevalence of current smoking among American Indian/Alaska Native adults has since declined to 25.1% in men and 21.0% in women for 2008 to 201023; therefore, a decline in mortality from COPD may be expected for that population in the future. However, a recent report observed that almost 39% of 15 million adults with self-reported COPD in 2011 in the United States continued to smoke.12 This large population represents an important opportunity for physician counseling and referral to smoking cessation interventions such as 1-800-QUIT-NOW.
Two broad currents influence mortality rates estimated from death certificate data: changes in the prevalence of COPD and changes in the case-fatality rate among people with COPD. Although the estimates of the prevalence of self-reported COPD from the NHIS suggest that the prevalence may have declined since 1999, the rates since 2002 have remained fairly stable. A number of treatment strategies have been shown to have the potential to reduce mortality in patients with COPD and include newer medications and evolving guidelines to treat COPD, oxygen therapy, respiratory management, pulmonary rehabilitation, and influenza vaccinations.24,25 The lag times between changes in the prevalence of COPD and the uptake of treatments and COPD mortality rates may differ. The balance of these temporal changes is likely to have a substantial impact on the trajectory of the mortality rate. With continued declines in the smoking prevalence and improved management of patients with COPD, mortality rates can be expected to decline in future years.
The generally small reduction in the age-adjusted mortality rate was limited to men. It is unclear why the mortality rate in women did not fall as well, given the decline in smoking prevalence in women since 1965. If the estimates are valid, these results suggest that research will be needed to address possible explanations for the poor progress among women. These data are consistent with the results of a study showing that the mortality rate among women with an obstructive impairment changed little in contrast to the mortality rate among men with an obstructive impairment.26
The use of spirometry is critical to establishing the diagnosis and severity of COPD. Additional tests that can help in the diagnosis include lung diffusion capacity test, chest radiograph, and arterial blood gas test. GOLD (Global Initiative for Chronic Obstructive Lung Disease) established four levels of COPD on the basis of spirometric measurements: mild, moderate, severe, and very severe.27 The results reported here should be considered in the context of several limitations. Depending on the spirometric criteria used, estimates of prevalence of COPD based on spirometry tests may be as much as double the estimates derived from self-reported information.13,28,29 Consequently, the estimates of self-reported prevalence of COPD in the current surveillance report almost certainly underestimate the true prevalence of this condition. Furthermore, not accounting for the undiagnosed percentage of adults with COPD can also potentially distort demographic comparisons. As shown in the previous surveillance report, men had a higher prevalence than women when the presence of COPD was based on spirometric criteria.13 When self-reported data were used to estimate the prevalence of COPD, however, women had a higher prevalence than men, as was also observed in the present report.
If COPD is underdiagnosed, then the mortality rates presented in the present report likely underestimate the true mortality rates from COPD.30‐32 Another factor that may contribute to underestimating COPD mortality rates is the possibility that comorbidities may displace COPD as the underlying cause of death that is reported on the death certificate.33 Assuming that underestimates of the COPD mortality rates were approximately constant during the study period, the interpretation of the direction of the trends is valid.
Race was self-reported by participants of the BRFSS and NHIS but was recorded by medical or other personnel in the other data systems. The comparability of race designations among surveys is unknown. For some data systems, such as the NAMCS, NHAMCS, and NHDS, race was missing for a large proportion of records. For example, 16% of the NHDS discharges for 2010 and 23% of NAMCS records in 2010 lacked information about the racial status of the patient. Medicare and death certificate data represented the only data that allowed trend analyses for American Indian/Alaska Natives, Hispanics, and Asian populations. Because race and ethnicity designations are subject to misclassification,34 caution is urged in interpreting racial- and ethnic-specific disparities. In the future, the BRFSS, with its large annual sample size of almost one-half million respondents, will allow trend analyses of prevalence of self-reported COPD among those racial/ethnic groups.
Since 1997, GOLD has striven to increase awareness of COPD as a major public health problem across the globe, to spur efforts to prevent this disease, and to develop guidelines to improve the diagnosis and treatment of COPD. In 2013, it released updated versions of Global Strategy for Diagnosis, Management, and Prevention of COPD.24 Several studies have reported imperfect implementation of the GOLD guidelines in clinical practice.35 Additional efforts may be needed to educate physicians about the management of this condition.
Healthy People objectives provide science-based, 10-year national objectives for improving the health of all Americans; identify nationwide health improvement priorities; and strive to engage multiple sectors (public health agencies, communities, organizations, academia, and medicine) to take actions to strengthen policies and improve practices that are driven by the best available evidence and knowledge. The Healthy People 2010 objective for COPD called for a 50% reduction in the mortality rate from COPD among adults aged ≥ 45 years at baseline in 1999 (123.9 per 100,000)36; however, that objective was not met by 2010 (116.6 per 100,000)—possibly for many reasons described above. The new Healthy People 2020 effort37 has been expanded to include the following objectives that pertain to the evaluation and management of COPD among adults aged ≥ 45 years:
• Reduce activity limitations among adults with COPD.
• Reduce deaths from COPD.
• Reduce hospitalizations for COPD.
• Reduce hospital ED visits for COPD
• Increase the proportion of adults with abnormal lung function whose underlying obstructive disease has been diagnosed.
The CDC and the National Heart Lung Blood Institute (NHLBI) have a formal collaboration to increase public awareness and identify critical communication, research, evaluation, and data collection needs to prevent and manage COPD. This collaboration has resulted in the annual BRFSS collection since 2011 of COPD prevalence data at state and local levels, which will enhance the COPD Learn More Breathe Better Campaign supported by the NHLBI. Such state-level and county-level data as the BRFSS, Medicare, and vital statistics can identify geographic clustering of, as well as racial/ethnic disparities in, COPD indicators to provide guidance to public health agencies in leveraging and targeting resources to those geographic areas and local populations with the greatest burden of COPD. These data will also be critical in identifying communities that will likely benefit best from awareness and outreach campaigns and in evaluating the effectiveness of public health efforts to prevent, treat, and control COPD.
COPD remains a significant source of morbidity and mortality in the United States. In 2007, chronic lower respiratory diseases constituted the fourth leading cause of death and rose to the third leading cause of death in 2008 primarily because cerebrovascular disease deaths continued a consistent decline and to a lesser extent as a result of adjustments to coding and classification.1 The data examined in this surveillance report testify to the heavy public health burden that COPD continues to levy in the United States. Prior to 1999, rates of mortality and hospitalizations had shown worrisome increases. Thus, the apparent leveling of the mortality rate and a decrease in the rate of hospitalization represent cause for cautious optimism. Future surveillance efforts will be critical to tracking the course of COPD in the United States.
Supplementary Material
Online Supplement
Acknowledgments
Financial/nonfinancial disclosures: The authors have reported to CHEST the following conflicts of interest: Dr Mannino has received honoraria/consulting fees and served on speaker bureaus for GlaxoSmithKline; Novartis AG; Pfizer, Inc; AstraZeneca; Forest Laboratories, Inc; and Creative Educational Concepts. Furthermore, he has received royalties from UptoDate, Inc. Drs Ford, Croft, Wheaton, Zhang, and Giles have reported that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Other contributions: Work was performed at the Centers for Disease Control and Prevention, Atlanta, Georgia. The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Additional information: The e-Tables can be found in the “Supplemental Materials” area of the online article.
Abbreviations
- BRFSS
Behavioral Risk Factor Surveillance System
- CDC
Centers for Disease Control and Prevention
- CHC
Community Health Center
- GOLD
Global Initiative for Chronic Obstructive Lung Disease
- ICD-9-CM
International Classification of Diseases, Ninth Revision, Clinical Modification
- ICD-10
International Classification of Diseases, 10th Revision
- NAMCS
National Ambulatory Medical Care Survey
- NHAMCS
National Hospital Ambulatory Medical Care Survey
- NHDS
National Hospital Discharge Survey
- NHIS
National Health Interview Survey
- NHLBI
National Heart, Lung, and Blood Institute
- NVSS
National Vital Statistics System
- PSU
primary sampling unit
References
- 1. Miniño AM, Xu J, Kochanek KD, Division of Vital Statistics.Deaths: preliminary data for 2008. Natl Vital Stat Rep. 2010;59(2):1-52. [PubMed]
- 2.Centers for Disease Control and Prevention (CDC) Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000-2004. MMWR Morb Mortal Wkly Rep. 2008;57(45):1226-1228 [PubMed] [Google Scholar]
- 3.Engström CP, Persson LO, Larsson S, Sullivan M. Health-related quality of life in COPD: why both disease-specific and generic measures should be used. Eur Respir J. 2001;18(1):69-76 [DOI] [PubMed] [Google Scholar]
- 4.Viegi G, Pistelli F, Sherrill DL, Maio S, Baldacci S, Carrozzi L. Definition, epidemiology and natural history of COPD. Eur Respir J. 2007;30(5):993-1013 [DOI] [PubMed] [Google Scholar]
- 5.Maurer J, Rebbapragada V, Borson S, et al. ; ACCP Workshop Panel on Anxiety and Depression in COPD Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest. 2008;134(suppl 4):43S-56S [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.National Institutes of Health, National Heart, Lung, and Blood Institute. Morbidity & mortality: 2012 chartbook on cardiovascular, lung, and blood diseases. National Heart, Lung and Blood Institute website. http://www.nhlbi.nih.gov/resources/docs/2012_ChartBook_508.pdf. Accessed March 15, 2013.
- 7.Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J. 2009;33(5):1165-1185 [DOI] [PubMed] [Google Scholar]
- 8.Stockley RA. Progression of chronic obstructive pulmonary disease: impact of inflammation, comorbidities and therapeutic intervention. Curr Med Res Opin. 2009;25(5):1235-1245 [DOI] [PubMed] [Google Scholar]
- 9.Mannino DM. Epidemiology and global impact of chronic obstructive pulmonary disease. Semin Respir Crit Care Med. 2005;26(2):204-210 [DOI] [PubMed] [Google Scholar]
- 10.Salvi SS, Barnes PJ. Chronic obstructive pulmonary disease in non-smokers. Lancet. 2009;374(9691):733-743 [DOI] [PubMed] [Google Scholar]
- 11.Lamprecht B, McBurnie MA, Vollmer WM, et al. ; BOLD Collaborative Research Group COPD in never smokers: results from the population-based burden of obstructive lung disease study. Chest. 2011;139(4):752-763 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC) Chronic obstructive pulmonary disease among adults—United States, 2011. MMWR Morb Mortal Wkly Rep. 2012;61(46):938-943 [PubMed] [Google Scholar]
- 13.Mannino DM, Homa DM, Akinbami LJ, Ford ES, Redd SC. Chronic obstructive pulmonary disease surveillance—United States, 1971-2000. MMWR Surveill Summ. 2002;51(6):1-16 [PubMed] [Google Scholar]
- 14.Ford ES, Mannino DM, Wheaton AG, Giles WH, Presley-Cantrell L, Croft JB. Trends in the prevalence of obstructive and restrictive lung function among adults in the United States: findings from the National Health and Nutrition Examination Surveys from 1988-1994 to 2007-2010. Chest. 2013;143(5):1395-1406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Behavioral risk factor surveillance system: survey data and documentation. Centers for Disease Control and Prevention website. http://www.cdc.gov/brfss/data_documentation.htm. Accessed March 15, 2013.
- 16.Centers for Disease Control and Prevention. National Health Interview Survey. Centers for Disease Control and Prevention website. http://www.cdc.gov/nchs/nhis.htm. Accessed October 3, 2011.
- 17.Centers for Disease Control and Prevention. Ambulatory health care data. Centers for Disease Control and Prevention website. http://www.cdc.gov/nchs/ahcd.htm. Accessed October 3, 2011.
- 18.Centers for Disease Control and Prevention. National Hospital Discharge Survey. Centers for Disease Control and Prevention website. http://www.cdc.gov/nchs/nhds.htm. Accessed October 3, 2011.
- 19.Centers for Disease Control and Prevention. Compressed mortality file 1979-1998 and 1999-2007. Centers for Disease Control and Prevention website. http://wonder.cdc.gov/wonder/help/cmf.html#. Accessed October 3, 2011.
- 20.Centers for Disease Control and Prevention. Compressed mortality file. Centers for Disease Control and Prevention website. http://www.cdc.gov/nchs/data_access/cmf.htm. Accessed October 3, 2011.
- 21.Klein RJ, Schoenborn CA. Age adjustment using the 2000 projected U.S. population. Healthy People 2010 Stat Notes. 2001;Jan(20):1-10 [PubMed] [Google Scholar]
- 22.Forey BA, Thornton AJ, Lee PN. Systematic review with meta-analysis of the epidemiological evidence relating smoking to COPD, chronic bronchitis and emphysema. BMC Pulm Med. 2011;11:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics. Health, United States, 2011: with special feature on socioeconomic status and health. Centers for Disease Control and Prevention website http://www.cdc.gov/nchs/data/hus/hus11.pdf. Accessed March 15, 2013.
- 24.Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (updated 2013).GOLD website. http://www.goldcopd.org/guidelines-global-strategy-for-diagnosis-management.html. Accessed March 15, 2013.
- 25.Qaseem A, Wilt TJ, Weinberger SE, et al. ; American College of Physicians; American College of Chest Physicians; American Thoracic Society; European Respiratory Society Diagnosis and management of stable chronic obstructive pulmonary disease: a clinical practice guideline update from the American College of Physicians, American College of Chest Physicians, American Thoracic Society, and European Respiratory Society. Ann Intern Med. 2011;155(3):179-191 [DOI] [PubMed] [Google Scholar]
- 26.Ford ES, Mannino DM, Zhao G, Li C, Croft JB. Changes in mortality among US adults with COPD in two national cohorts recruited from 1971-1975 and 1988-1994. Chest. 2012;141(1):101-110 [DOI] [PubMed] [Google Scholar]
- 27.Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. GOLD website. http://www.goldcopd.org/uploads/users/files/GOLDWkshp2001.pdf. Accessed August 24, 2012.
- 28.Celli BR, Halbert RJ, Isonaka S, Schau B. Population impact of different definitions of airway obstruction. Eur Respir J. 2003;22(2):268-273 [DOI] [PubMed] [Google Scholar]
- 29.Halbert RJ, Natoli JL, Gano A, Badamgarav E, Buist AS, Mannino DM. Global burden of COPD: systematic review and meta-analysis. Eur Respir J. 2006;28(3):523-532 [DOI] [PubMed] [Google Scholar]
- 30.Hansell AL, Walk JA, Soriano JB. What do chronic obstructive pulmonary disease patients die from? A multiple cause coding analysis. Eur Respir J. 2003;22(5):809-814 [DOI] [PubMed] [Google Scholar]
- 31.Jensen HH, Godtfredsen NS, Lange P, Vestbo J. Potential misclassification of causes of death from COPD. Eur Respir J. 2006;28(4):781-785 [DOI] [PubMed] [Google Scholar]
- 32.Hughes TS, Muldoon SB, Tollerud DJ. Underestimation of mortality due to chronic obstructive pulmonary disease (COPD) in Kentucky. J Ky Med Assoc. 2006;104(8):331-339 [PubMed] [Google Scholar]
- 33.Sin DD, Anthonisen NR, Soriano JB, Agusti AG. Mortality in COPD: role of comorbidities. Eur Respir J. 2006;28(6):1245-1257 [DOI] [PubMed] [Google Scholar]
- 34.Arias E, Schauman WS, Eschbach K, Sorlie PD, Backlund E. The validity of race and Hispanic origin reporting on death certificates in the United States. Vital Health Stat 2. 2008;Oct(148):1-23 [PubMed] [Google Scholar]
- 35.Chavez PC, Shokar NK. Diagnosis and management of chronic obstructive pulmonary disease (COPD) in a primary care clinic. COPD. 2009;6(6):446-451 [DOI] [PubMed] [Google Scholar]
- 36.U.S. Department of Health and Human Services. Tracking Healthy People 2010. Washington, DC: US Government Printing Office; 2000. [Google Scholar]
- 37.U.S. Department of Health and Human Services. doi: 10.3109/15360288.2015.1037530. Respiratory diseases. Healthy People website. http://healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=36. Accessed October 3, 2011. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Online Supplement