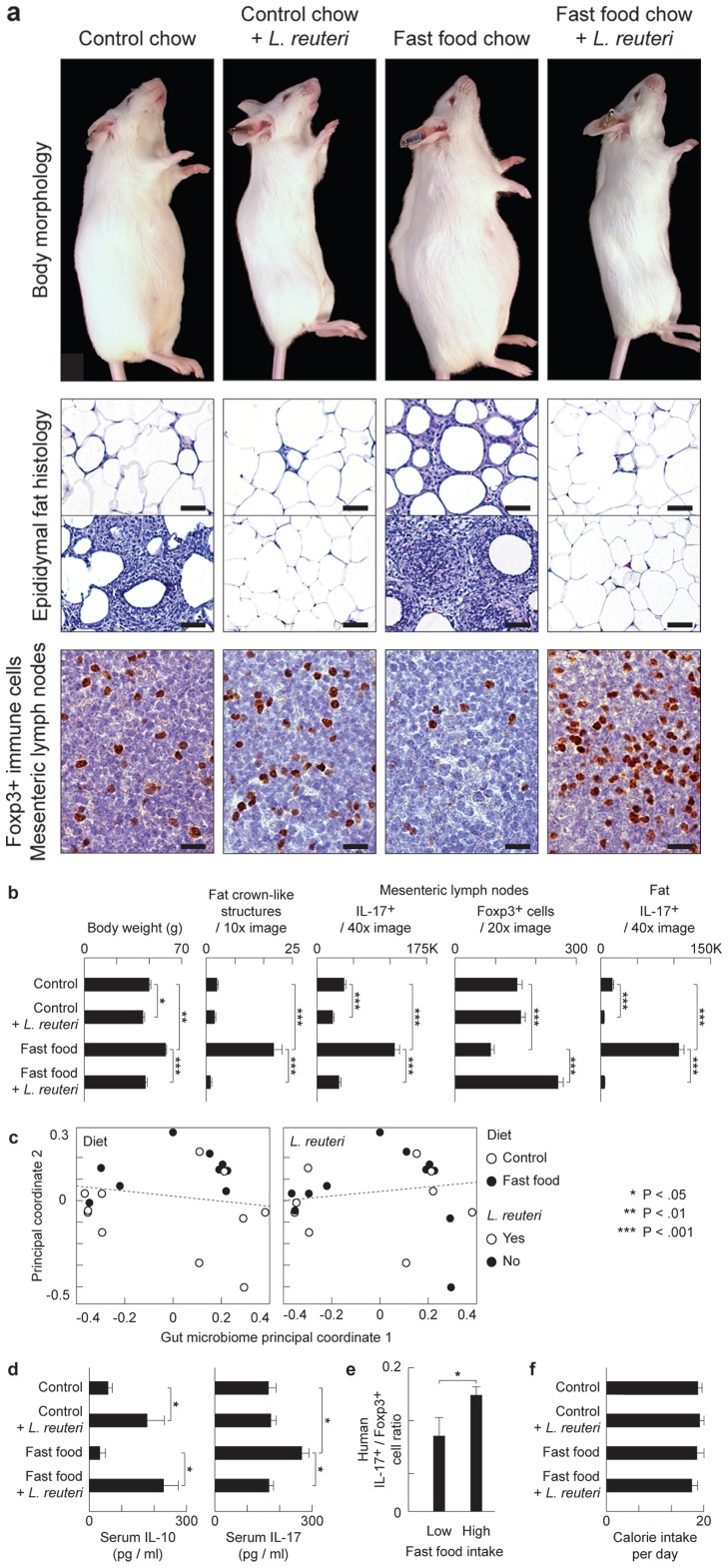
Figure 1. Eating probiotics blocks a gut microbiota-immunity-obesity axis.
L. reuteri protects mice from Western diet-associated obesity. Data are shown in male outbred Swiss mice at the age of 5 months. Numerous crown-like structures (CLS) caused by adipocyte death-related inflammation, and focal pyogranulomatous inflammation (PGI) arise in abdominal fat of ‘fast food’-fed but not probiotic-fed animals. Probiotics increase anti-inflammatory Foxp3+ regulatory (Treg) cells and reduce pro-inflammatory Il17 protein to restore immune balance coinciding with a slender physique (a and b), without restructuring GI microbial communities (c). In the same mice, serum cytokine analysis shows that the pro-inflammatory Il-17-associated effect of obesity is systemic, and that L. reuteri negates this effect up-regulating the anti-inflammatory cytokine Il-10 (d). Humans frequently eating ‘fast food’ also show an elevated ratio of pro-inflammatory IL17+/anti-inflammatory Foxp3+ Treg in peripheral blood cells compared to subjects never eating ‘fast food’ (e). Probiotic-consuming slim mice chose similar calories when compared with obese animals, regardless of baseline diet, highlighting potential for translational medicine (f). Fat histology: Hematoxylin and eosin, Bars = 50 µm; MLN Immunohistochemistry: Diaminobenzidine chromogen, hematoxylin counterstain, Bars = 8.3 µm.