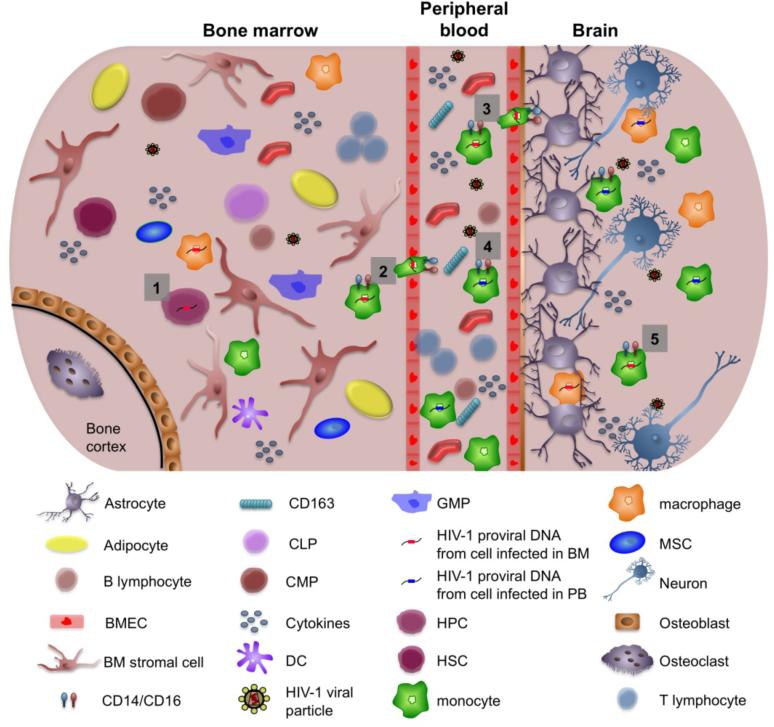
Fig (2).
Migration of human immunodeficiency virus 1 (HIV-1)-infected cells from the bone marrow (BM) to the central nervous system (CNS). (1) Hematopoietic progenitor cells (HPCs) expressing CD4 and CXCR4/CCR5 can be infected in the BM of HIV-1-infected patients. (2) HIV-1-infected monocytes and macrophages from the bone marrow reseed the peripheral blood (PB). (3) HIV-1-infected cells from the BM that have reseeded the peripheral blood traverse the blood-brain barrier as well as (4) monocytic cells infected within the peripheral blood compartment. These cells have been shown to be more CD14+/16+ and associated with increased neurological disease. (5) Both monocytic cells that were infected in the BM and cells infected in the peripheral blood contribute to carrying HIV into the CNS, thereby spreading infection to cells found within the CNS such as perivascular macrophages, microglial cells, and astrocytes. Changes in cytokine profiles brought about by HIV-1 infection can also affect the migration of HIV-1-infected cells, thus helping to enhance the progression of HIV-1 infection. In addition, soluble CD163 found within the peripheral blood has been associated with HIV-1-associated neurological disease. BMEC, bone marrow microvascular endothelial cell; CLP, committed lymphoid progenitors; CMP, committed myeloid progenitors; DC, dendritic cells; GMP, granuloctye-macrophage progenitors; HSC, hematopoietic stem cells; MSC, mesenchymal stem cells.