Abstract
We present a spectrum of findings with transthoracic echocardiography, coronary angiography, and open surgical exploration in a 54-year-old man who presented with an acute ST segment elevation myocardial infarction and was diagnosed with impending paradoxical emboli. He underwent successful surgical removal of the thrombus.
<Learning objective: Impending paradoxical embolism, a biatrial thromboembolus in transit across a patent foramen ovale, is associated with a 20% mortality rate. Very rarely does it present as a ST segment elevation myocardial infarction. The optimal management (medical or surgical) for those who present with it remains a subject of debate, although surgery has been associated with less systemic embolization.>
Keywords: Paradoxical emboli, Myocardial infarction
Introduction
Impending paradoxical embolism is a biatrial thromboembolus in transit across a patent foramen ovale. It is rare for this entity to present clinically as a myocardial infarction, and the optimal management (medical or surgical) for those who present with it remains a subject of debate. We report a case of impending paradoxical embolism presenting as a ST segment elevation myocardial infarction. The patient ultimately underwent open surgical exploration and removal of the clot.
Case report
A 54-year-old man with a past medical history of hypertension, hyperlipidemia, and diabetes mellitus was hospitalized following a motor vehicle accident in July 2010. While being treated for his traumatic injuries he sustained a pulmonary embolism and was initiated on systemic anticoagulation with warfarin. More than one year later in October 2011, the warfarin was discontinued and he underwent a successful elective ventral hernia repair. He was maintained on prophylactic doses of low molecular weight heparin during a brief hospital stay and was discharged with instructions not to restart the warfarin. One month later he presented to the emergency department with complaints of new onset chest pain and shortness of breath. A 12-lead electrocardiogram showed anterolateral ST segment elevation (Fig. 1). Emergent coronary angiography revealed thrombolysis in myocardial infarction (TIMI) 1 flow in the left anterior descending coronary artery with evidence of a large intracoronary filling defect consistent with thrombus (Fig. 2, panel A). After initial thrombectomy of the left anterior descending coronary artery, abrupt closure of the vessel occurred due to the presence of a coronary dissection, a common occurrence following balloon inflation that did not respond to multiple balloon inflations. Deployment of an intracoronary stent, therefore, was performed in order to maintain vessel patency. Following stenting of the left anterior descending coronary artery, TIMI 3 flow was restored (Fig. 2, panel B), he became chest pain free and was transferred to the coronary care unit. Upon arrival at the coronary care unit, immediately following the cardiac catheterization, a bedside transthoracic echocardiogram was performed to assess left ventricular systolic function. The echocardiogram revealed a large mobile mass originating in the right atrium, crossing the interatrial septum into the left atrium, and prolapsing into the left ventricle during diastole (Fig. 3, panels A and B and Videos 1 and 2). These images were consistent with a thrombus caught in transit across a patent foramen ovale. Thus, impending paradoxical embolism was diagnosed and intravenous heparin was started immediately. Ultrasound examination of all four extremities was performed and revealed the presence of a non-occlusive deep vein thrombosis in the left lower extremity (Fig. 4). Cardiothoracic surgery was consulted for consideration of surgery due to the size of the clot and risk of further embolization. Due to the extensive anterior ST elevation myocardial infarction on presentation and subsequent stenting of the left anterior descending coronary artery, it was decided that he would be at high risk for emergent cardiothoracic surgery that same day and should first be systemically anticoagulated with intravenous heparin and undergo placement of an inferior vena cava filter prior to surgical removal of the clot. Due to evidence of acute renal insufficiency on admission, a computed tomography-pulmonary angiogram was not performed in order to decrease the risk of contrast-induced renal failure prior to surgery. After 48 h of systemic anticoagulation and placement of the inferior vena cava filter, the patient was transferred to the operating room where, under cardioplegic arrest, a right atriotomy was performed and the clot was successfully removed in its entirety (Fig. 5, panel A), and the patent foramen ovale was surgically closed. The clot was approximately 14 cm in length (Fig. 5, panel B). The patient had an uncomplicated post-operative course. On admission, the patient's activated partial thromboplastin time, prothrombin time, and international normalized ratio were all within normal range. An extensive hypercoagulability work-up was performed during his hospitalization, including the following panel of tests: beta-2 globulin, anticardiolipin antibody, Russell's viper venom time, silica clotting time, factor V Leiden, factor II, prothrombin gene mutation, protein C, protein S, and antithrombin III. All tests were negative for a hypercoaguable state. Lastly, the patient did not have any other known co-existing conditions that would predispose him to be hypercoaguable. He was discharged home on warfarin, aspirin, and clopidogrel. Three weeks later he was working in his garden.
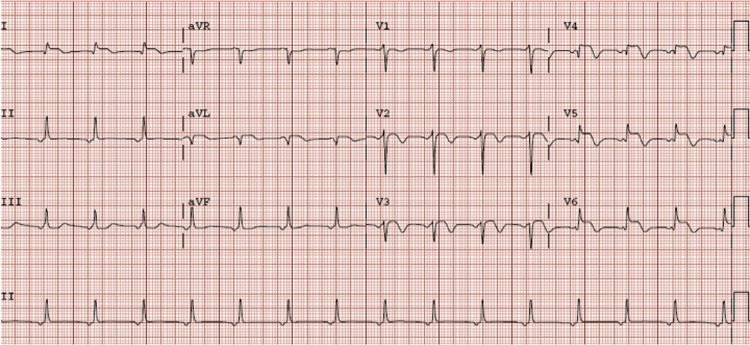
Fig. 1.
12-Lead electrocardiogram showing ST segment elevation in the anterior and lateral leads.
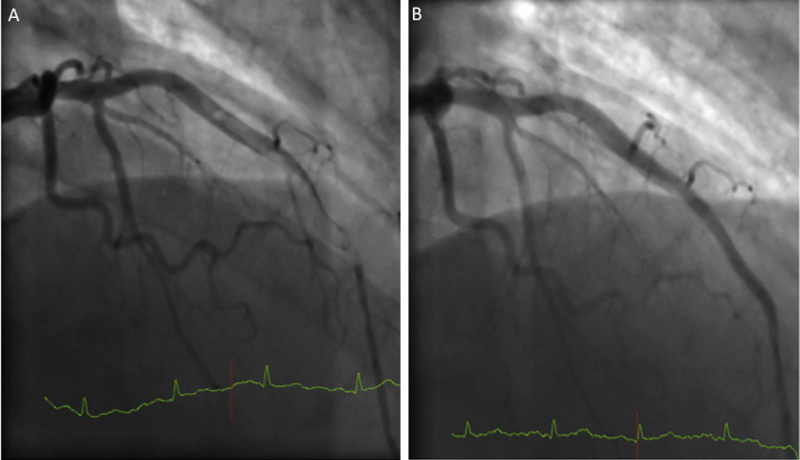
Fig. 2.
Coronary angiography revealing large filling defect consistent with thrombus in the mid and distal left anterior descending coronary artery (panel A). Coronary angiography of left anterior descending coronary artery following thrombus aspiration, balloon angioplasty and stenting (panel B).
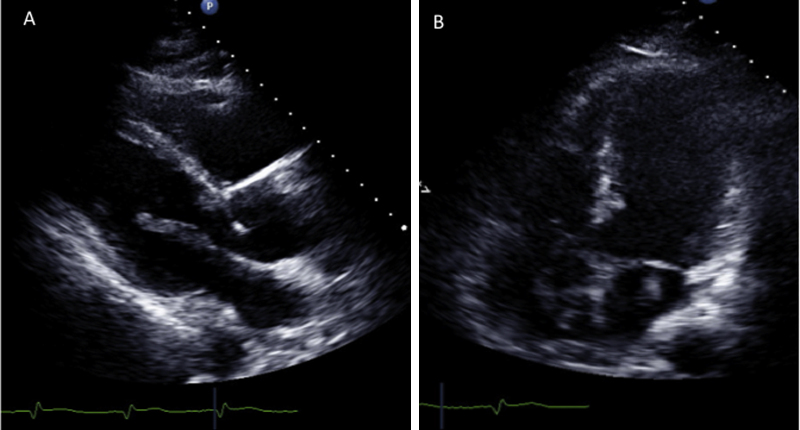
Fig. 3.
Parasternal long-axis image on transthoracic echocardiography showing a mobile linear density originating in the left atrium, prolapsing into the left ventricle during diastole. Also noted is anterior septal akinesis (panel A, Video 1). Apical four-chamber image on transthoracic echocardiography showing mobile left and right atrial densities connected through the atrial septum. Also noted is extensive antero-apical left ventricular akinesis (panel B, Video 2).
Fig. 4.

Lower extremity ultrasound demonstrating a non-occlusive thrombus of the left femoral vein.
Fig. 5.
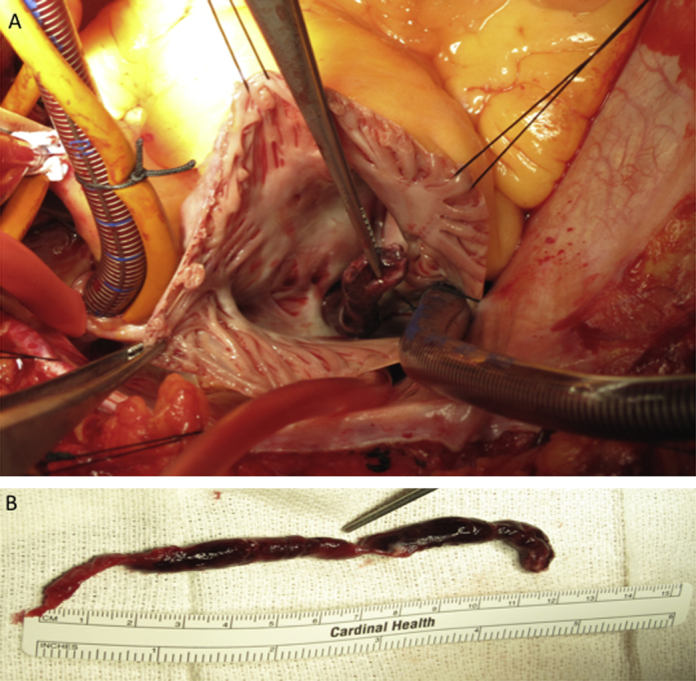
Intra-operative photograph of clot removal through the patent foramen ovale via a right atriotomy under cardioplegic arrest (panel A). The septum was opened to allow safe removal of the entire clot and to prevent fragmentation, and the patent foramen ovale and atriotomy were then closed primarily. Entire extracted thrombus shown (panel B).
Discussion
Impending paradoxical embolism, a biatrial thromboembolus in transit across a patent foramen ovale, was first described on echocardiography nearly 30 years ago [1]. In the setting of a pulmonary embolism and acutely elevated pulmonary arterial pressures, a foramen ovale can become patent and allow thrombus to migrate toward the left atrium. If very large, the thrombus can become trapped during its passage producing an impending paradoxical embolus that is associated with high morbidity and mortality.
Determining the appropriate treatment strategy, however, is a subject of debate and is predicated on clinical presentation, hemodynamic stability, medical comorbidities, size of the thrombus, risk of bleeding, and importantly, the risk of a devastating systemic embolic event. Based on a small number of case reports such as ours, some authors have recommended surgical thromboembolectomy and closure of the patent foramen ovale because of the high risk of thromboembolism during treatment with thrombolytic therapy or anticoagulation alone. Others, however, suggest that thrombolysis should be the preferred treatment since it can act on clot present in multiple sites throughout the body simultaneously. A recent systematic review of the literature evaluated predictors of both systemic embolization as well as mortality in 174 patients and is the most complete review on this subject to date [2]. They found that despite optimal management, impending paradoxical emboli was associated with nearly a 20% mortality rate and that two-thirds of the deaths occurred within the first 24 h after the diagnosis was made. Thrombolytic therapy was associated with systemic embolization in about one-quarter of the patients. While multivariate analysis did not identify independent predictors of mortality, systemic embolization during treatment and the combined endpoint of mortality and systemic embolization were both significantly decreased in the patients who were treated surgically [2]. In the systematic review of the literature, 91% of the patients presented with a pulmonary embolism and only 5% presented with a myocardial infarction. Our patient had a prior history of pulmonary embolism and evidence on admission of a left lower extremity deep vein thrombosis. Although we cannot prove it, we hypothesize that a portion of the deep vein thrombosis traveled to the heart, lodged across the patent foramen ovale and embolized smaller pieces down the left anterior descending coronary artery causing an acute myocardial infarction.
Acknowledgment
This work was supported by the National Institutes of Health (HL97074 to E.C.K.).
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jccase.2013.01.003.
Appendix A. Supplementary data
The following are Supplementary data to this article:
References
- 1.Nellessen U., Daniel W.G., Matheis G., Oelert H., Depping K., Lichtlen P.R. Impending paradoxical embolism from atrial thrombus: correct diagnosis by transesophageal echocardiography and prevention by surgery. J Am Coll Cardiol. 1985;5:1002–1004. doi: 10.1016/s0735-1097(85)80449-6. [DOI] [PubMed] [Google Scholar]
- 2.Myers P.O., Bounameaux H., Panos A., Lerch R., Kalangos A. Impending paradoxical embolism: systematic review of prognostic factors and treatment. Chest. 2010;137:164–170. doi: 10.1378/chest.09-0961. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.