Abstract
Objectives
To test the hypotheses that, in comparison with a Control group that received standard care, users of manual wheelchairs who also received the French-Canadian version of the Wheelchair Skills Training Program (WSTP) would significantly improve their wheelchair-skills capacity and that these improvements would be retained at 3 months.
Design
Multi-center, single-blind randomized controlled trial (RCT).
Participants
39 manual wheelchair users, a sample of convenience.
Setting
3 rehabilitation centers in Montreal, Quebec, Canada.
Intervention
Participants were randomly allocated to the WSTP or Control groups. Participants in both groups received standard care. Participants in the WSTP group also received a mean of 5.9 training sessions (mean total duration of 5 hours and 36 minutes).
Main Outcome Measures
The French-Canadian version of the Wheelchair Skills Test (WST) (Version 3.2) was administered at baseline (T1), post-training (T2, a mean of 47 days after T1) and at follow-up (T3, a mean of 101 days after T2).
Results
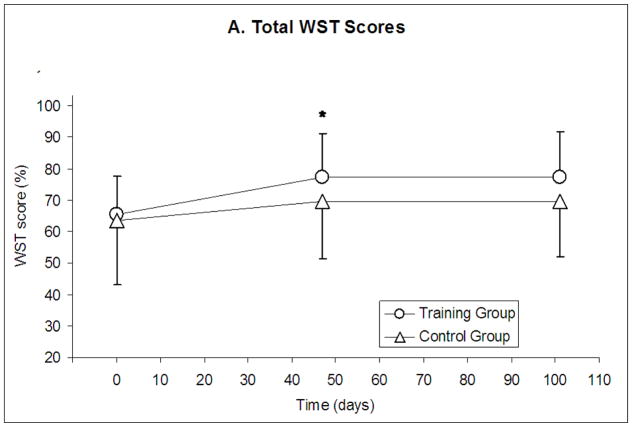
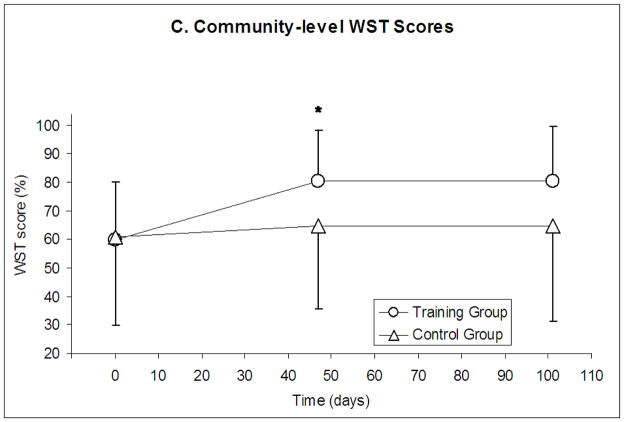
At T2, the mean ± SD total percentage WST capacity scores were 77.4 ± 13.8% for the WSTP group and 69.8 ± 18.4% for the Control group (p = 0.0296). Most of this difference was due to the Community-level skills (p=0.0018). The total and subtotal WST scores at T3 decreased by ≤ 0.5% from the T2 values, but differences between groups at T3, adjusting for T1, did not reach statistical significance (p ≥ 0.017 at a Bonferroni-adjusted α level of 0.005).
Conclusion
WSTP training improves wheelchair skills immediately after training, particularly at the Community-skills level, but this study did not show statistically significant differences between the groups at 3 months.
Keywords: Wheelchair, Training, Rehabilitation, Motor skills
Wheelchairs can have a highly positive impact on their users’ lives1 but they are not without problems, including their frequent need for repairs,2 their role in overuse injuries3,4 and acute injuries that can occur during use.5–9 One important aspect of the wheelchair-provision process that has become increasingly well recognized is training in wheelchair use.10 There is growing evidence that manual wheelchair skills capacity improves with training11–16 and for an association between manual wheelchair skills capacity and participation.16–18 However, formal wheelchair skills training is still relatively uncommon.19–21 Although there are a variety of possible reasons for this (e.g. time constraints, limited funding, short lengths of stay), one of the reasons may have been the lack of standardized and readily available training resources.
In an attempt to address this perceived difficulty, the Wheelchair Skills Program (WSP) was developed in 1996.22 The WSP consists of an evidence-based set of assessment and training protocols, the Wheelchair Skills Test (WST) and the Wheelchair Skills Training Program (WSTP). The WSTP represents an attempt to combine the best available evidence on motor-skills learning with the best evidence on how to perform specific wheelchair skills. The WSTP for manual wheelchairs has been found to be safe and more efficacious than standard care in both rehabilitation-center and community settings.13,14 Despite these promising results, when this study began, published evidence regarding the WSTP had come from only a single center. Since then, Ozturk and Ucsular15 found similar short-term improvements in Turkey. However, the retention of benefits beyond a few days has not been reported in any of the earlier WSTP studies.
Our primary objective was to test the hypothesis that, in comparison with a Control group that received standard care, users of manual wheelchairs who received the French-Canadian version of the WSTP23 would significantly improve their wheelchair-skills capacity (as represented by total percentage WST scores). Our secondary objectives were to test the hypothesis that these improvements would be retained at 3 months, to assess differences in subgroups of skills (Indoor, Community and Advanced levels), to describe differences in individual skills and to determine if the WSTP is safe.
METHODS
Participants
We studied 39 manual wheelchair users, a sample of convenience. The sample-size estimate for the primary objective was based on a power analysis using data from earlier studies.13,14 A sample size of 12 in each group was estimated to have 80% power to detect a main-effect difference in mean WST scores of 14.8% assuming that the common standard deviation (SD) was 12.2%, if using a two-group t-test with a 0.05 two-sided significance level. We over-sampled in anticipation of drop-outs and to provide greater power to meet our secondary objectives.
Setting
The study was conducted in 3 rehabilitations centers located in Montréal. These centers were the Institut de réadaptation Gingras-Lindsay-de-Montréal (IRGLM), the Centre de réadaptation Lucie-Bruneau (CRLB) and the Institut universitaire de gériatrie de Montréal (IUGM). Coordination among the sites was provided by the principal investigator. These sites were different with respect to the wheelchair-provision models of care, funding arrangements and language from the sites where the earlier studies13–15 had been performed. The wheelchair-provision process at these 3 centers was similar in that the assessment, prescription and set-up were performed by occupational therapists and wheelchairs were available free of charge from the Province of Quebec.
Study Design
This was a multi-center, single-blind, randomized controlled trial (RCT). Blinding was carried out by isolating the personnel and processes for randomization, testing, training and data analysis. Due to the nature of the intervention, it was not possible to blind participants about whether they received training.
Ethical Issues
Ethical approvals for this study were obtained from the research ethics boards of the recruitment sites. Each participant provided his/her informed consent.
Recruitment and Screening
Potential participants were approached by clinicians at the rehabilitation centers or hospitals who were made aware of the inclusion and exclusion criteria for the study. If a potential participant agreed, he/she was then formally screened by a member of the research team regarding the inclusion and exclusion criteria. Eligibility to participate was based on the following criteria: was 18 years of age or older; used a manual wheelchair daily; was receiving therapy at one of the recruitment sites; was willing and able to take part in the study (as evidenced by participating in at least the baseline assessments); was fluently French-speaking; was competent to give informed consent (or had a proxy with power of attorney); had the permission of the clinical occupational therapist working with the participant to participate (so the study would not be in conflict with other studies or care directions); had enough ability to develop skills included in the WSTP, in the subjective opinion of the occupational therapist; did not have an unstable medical condition (e.g. angina, seizures, as confirmed by the clinician who referred the participant); and did not have an emotional or psychiatric problem of a type or extent that might make participation unpleasant.
Demographic and Clinical Data
To describe the sample, we recorded demographic and clinical data at baseline, specifically age (years), sex (male/female), height (cm), weight (kg), rehabilitation-center site, clinical status (inpatient/outpatient), diagnosis accounting for wheelchair use and date of onset of diagnosis.
Wheelchair-Usage and Wheelchair Data
At baseline we recorded wheelchair-usage data by self-report, specifically, the extent of experience with any wheelchair (years), the extent of experience with the current wheelchair (weeks), the frequency of wheelchair use (hours/day), the method of wheelchair propulsion (combinations of hands and feet used) and the location of wheelchair use (home, work, school, community and/or recreation/sports). Wheelchair specifications were recorded at baseline using the Wheelchair Specification Form.22 We also recorded whether any changes in the wheelchair were noted at the following testing sessions, but we did not record the reason for or nature of any such changes.
Group Allocation
Participants were randomly allocated to the WSTP or Control groups by the principal investigator using a table of random numbers.24 For the purpose of having approximately equal representations of musculoskeletal and neurological impairments in the two groups, we used this diagnostic-group criterion (musculoskeletal vs neurological) to stratify the groups.
Intervention – Wheelchair Skills Training Program (WSTP)
Routhier et al have previously reported on the process used to translate WSP materials from English to French-Canadian.25–27 The French-Canadian version of the WSTP was used, following the procedures in the 113-page WSP Manual.23 Each participant was trained by 1 of 3 occupational therapists, each of whom had received trainer training. Participants received a target of 4–8 training sessions, each 45–60 minutes long, during a period of 2–4 weeks. The actual number of sessions and their duration were recorded. Training was stopped after 8 sessions or when no improvement was noted by the trainer.
Outcome Measures
Wheelchair Skills Test (WST)
A variety of tools have been used to assess wheelchair skills. We elected to use the WST because it has been highly ranked in independent surveys of such tests,28,29 because it has been well studied with respect to measurement properties30–33 and because it corresponds well with the skills trained during the WSTP. Wheelchair skills were tested according to the WST procedures outlined in the French-Canadian version of the WSP (Version 3.2) Manual.23 WST 3.2 consists of 57 skills (listed later), including 30 at the Indoor level, 13 at the Community level and 14 at the Advanced level. Each skill was scored (pass/fail) on the basis of defined criteria. For the small number of participants who were unable to complete the objective WST assessments post-training or at follow-up due to transportation difficulties, the questionnaire version of the WST (WST-Q)34–36 was administered to minimize what would otherwise have resulted in missing data due to drop-outs. For the purposes of this study, the WST and WST-Q results were considered equivalent because of the high correlations between total scores.34–36 Testers were two occupational therapists, each of whom had been trained in WST administration.
The numerator for the total percentage WST score was the total raw score (the number of skills passed). The denominator was the total possible score (i.e. 57 minus the number of skills that were not applicable because the wheelchair did not have the part [e.g. footrests that could not be removed]). Subtotal WST percentage scores were similarly calculated for the Indoor, Community and Advanced skill levels.
Safety
The tester served as a spotter during WST testing and the trainer served as a spotter during training, following the principles described in the WSP Spotter Manual (16 pages).22 Testers and trainers recorded any adverse wheelchair-related incidents (e.g. actual injuries or tips/falls with the potential for injury) during testing or training.
Procedure
Prior to the first testing session (T1), we conducted screening, obtained informed consent and allocated participants to group. At T1, we collected baseline demographic, clinical, wheelchair-usage, wheelchair and WST data. Those in the WSTP group then received WSTP training in addition to standard care. Participants in the Control group received only standard care. Details about standard care were not recorded for either group. (Estimates from an earlier study by MacPhee et al13 suggest that inpatient rehabilitation in a Canadian rehabilitation center might include about 15 hours of training that is variable in format.) Within 1 week after completing training, participants in the WSTP group were retested (T2). The T2 evaluations for the Control group were carried out at a target latency of 3–5 weeks after T1. Retention tests (T3) were administered to all participants at a target latency of 3 months after T2. Participants were permitted to have the testers or trainers remove or reposition their rear anti-tip devices for testing or training.
Data analysis
Data were recorded in a spreadsheeta on a personal computer. The statistical software used was SAS (version 9.2).b Total WST percentage scores and subtotal percentage scores (for Indoor, Community and Advanced levels) were calculated for each participant. Group success rates were calculated for each skill.
Descriptive statistics were determined for all data. The choice of statistical tests was based on the nature and distribution of the data. The comparability of the WSTP and Control groups was evaluated for selected baseline and study-process data. Specifically, we used the Fisher exact test for clinical setting, wheelchair use at work, wheelchair use at school and wheelchair changes during the course of the study. We used the Chi-square test for sex, wheelchair use at home, wheelchair use in the community and wheelchair use for recreation/sports. We used the Wilcoxon rank-sum test for age, height, weight, length of time from onset of diagnosis to T1, duration of experience with any wheelchair, duration of experience with the current wheelchair, amount of time between T1 and T2 and amount of time between T2 and T3. We used logistic regression for propulsion method (3 levels of categorical variable). Variables with more than two categories and insufficient data in each category (specifically diagnosis accounting for wheelchair use, rehabilitation center and frequency of wheelchair use) were not compared using statistical tests. For the group comparability assessments, we used a Bonferroni-adjusted α level of 0.004 (0.05/14) to control for multiple comparisons.
Regarding outcomes, we compared the total and subtotal percentage WST scores at T2 using Analyses of Covariance, adjusting for the T1 values. An α level of 0.05 was used for the primary outcome measure (total percentage WST scores for the between-group comparisons at T2). When looking at retention from T2 to T3, paired t tests were used to make within-group comparisons. To assess whether any differences between the groups could be seen at T3, we also used an ANCOVA model for T3 total and subtotal WST scores, adjusting for T1 values. For the secondary comparisons, the α level was Bonferroni-adjusted to 0.005 (0.05/11).
We dealt with missing data due to drop-outs by using intention-to-treat (ITT) procedures, qualitatively comparing the drop-outs in each group from the perspective of demographic, clinical and wheelchair data. We performed sensitivity analyses in two ways to investigate the impact of missing WST values on the T2 comparisons. First, we carried forward T1 WST scores for those without T2 values and second, we used the mean within-group T1 values for T2 values. For the T2-T3 sensitivity analysis, for those subjects with missing values at T2 or T3, we only used the latter method, to avoid forcing there to be no change for the missing participants and thereby biasing results toward non-significance (our hypothesis).
For wheelchair components and individual skills, we did not conduct statistical comparisons between the groups because our sample size would not have provided adequate power. For the individual skills, we used descriptive comparisons, using a difference of ≥25% in the success rates between the 2 groups and the 3 time periods as our threshold for a clinically meaningful difference. We reported the mean of left-and right-side scores for this purpose.
RESULTS
Participants
Figure 1 shows the participant flow.37 Two potential participants were eliminated prior to enrollment due to not meeting the inclusion and/or exclusion criteria. Because the participants were recruited from inpatient and outpatient populations at 3 sites, we do not have an accurate estimate of the size of the potential participant pool of manual wheelchair users from which our sample was drawn. As such, this was a sample of convenience. Overall, 8 (21%) of the 39 participants dropped out of the study, 1 (5%) of the 19 from the WSTP group (during the T1-T2 interval) and 7 of the 20 from the Control group (4 [20%] during the T1-T2 interval and 3 [15%] during the T2-T3 interval). The reasons for dropping out were loss of interest (4) and scheduling difficulties (4). Table 1 summarizes the demographic and clinical data at baseline. The WSTP and Control groups were not significantly different with respect to the baseline comparisons performed.
Figure 1.
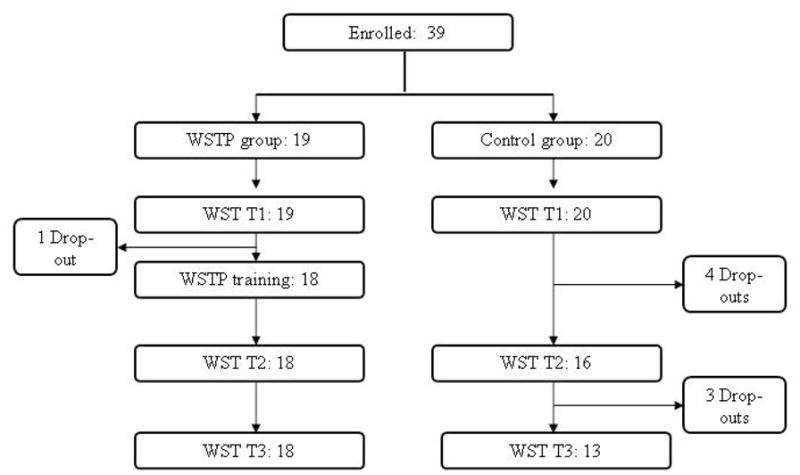
Flow diagram reflecting participant involvement.
Table 1.
Participant Demographic and Clinical Data at Baseline
| Characteristics | Parameter | WSTP Group (n = 19) | Control Group (n = 20) | P Value* |
|---|---|---|---|---|
|
| ||||
| Age (years) | Mean ± SD | 48.9 ± 18.9 | 43.1 ± 22.1 | 0.240 |
|
| ||||
| Sex (n [%]) | Women | 6 (31.6%) | 6 (30.0%) | 0.915 |
|
| ||||
| Height (cm) | Mean ± SD | 164.5 ± 10.9 | 163.5 ± 11.5 | 0.307 |
|
| ||||
| Weight (kg) | Mean ± SD | 83.7 ± 13.8 | 70.2 ± 17.0 | 0.025 |
|
| ||||
| Rehabilitation center site | CRLB | 9 (47%) | 6 (30%) | NA |
| IRGLM | 9 (47%) | 12 (60%) | ||
| IUGM | 1 (5%) | 2 (10%) | ||
|
| ||||
| Clinical status (n [%]) | Inpatient | 14 (73.7%) | 17 (85.0%) | 0.451 |
|
| ||||
| Diagnosis accounting for wheelchair use | Amputations | 5 (26%) | 4 (20%) | NA |
| MS | 6 (32%) | 2 (10%) | ||
| SCI | 7 (37%) | 12 (60%) | ||
| Other | 1 (5%) | 2 (10%) | ||
|
| ||||
| Time from diagnosis to T1 (years) | Median | 0.4 | 0.3 | 0.656 |
| Range | 0.1–10.3 | 0.1–11.7 | ||
The Bonferroni-adjusted α level is 0.004.
Abbreviations: CRLB = Centre de réadaptation Lucie-Bruneau, IRGLM = Institut de réadaptation Gingras-Lindsay-de-Montréal, IUGM = Institut universitaire de gériatrie de Montréal, MS = multiple sclerosis, NA = not applicable due to insufficient data in each category, SCI = spinal cord injury, SD = standard deviation.
Where the variance (the standard deviation as a percentage of the mean value) was high, we have reported the median value.
Wheelchair-Usage and Wheelchair Data
Wheelchair-usage data are shown in Table 2. Most participants had minimal prior wheelchair experience, propelled their wheelchairs with two hands, used their wheelchairs for over 4 hours each day and used their wheelchairs both indoors and in the community. There were no statistically significant differences between the groups at baseline. Table 3 summarizes the wheelchair-component data at baseline and shows that the wheelchairs used by the two groups were qualitatively similar. In the T1-T2 interval, the wheelchairs of 3 (14%) participants changed (2 in the Training group and 1 in the Control group), but there was no significant difference between the groups in the incidence of such changes (p = 1.000). In the T2-T3 interval, the wheelchairs of 11 (52%) participants changed (4 in the Training group and 7 in the Control group), but there was no significant difference between the groups in the incidence of such changes (p = 0.198).
Table 2.
Wheelchair-Usage Data at Baseline
| Characteristic | Parameter | WSTP Group (n = 19) | Control Group (n = 20) | P Value* |
|---|---|---|---|---|
|
| ||||
| Experience with any wheelchair (years) | Median | 0.3 | 0.2 | 0.436 |
| Range | 0.1–15.0 | 0.1–6.5 | ||
|
| ||||
| Experience with current wheelchair (weeks) | Median | 6.0 | 5.5 | 0.396 |
| Range | 0.1–771 | 1–52 | ||
|
| ||||
| Frequency of wheelchair use (hours/day) | <=2 | 1 (5%) | 1 (5%) | NA |
| 2–4 | 3 (16%) | 0 (0%) | ||
| 4–6 | 6 (32%) | 4 (20%) | ||
| 6–8 | 3 (16%) | 6 (30%) | ||
| >8 | 5 (26%) | 8 (40%) | ||
|
| ||||
| Method of wheelchair propulsion | 2 hands | 14 (73.7%) | 14 (70%) | 0.798* |
| Foot/feet only | 1 (5.3%) | 0 (0%) | ||
| 2 hands + 1–2 feet | 4 (21.1%) | 6 (30.0%) | ||
|
| ||||
| Location of wheelchair use | Home | 15 (79%) | 12 (60%) | 0.200 |
|
| ||||
| Work | 1 (5%) | 1 (5%) | 0.970 | |
|
| ||||
| School | 1 (5%) | 0 (0%) | 0.487 | |
|
| ||||
| Community | 13 (68%) | 13 (65%) | 0.821 | |
|
| ||||
| Recreation/Sports | 7 (37%) | 6 (30%) | 0.651 | |
The Bonferroni-adjusted α level is 0.004.
Abbreviation: NA = not applicable due to insufficient data in each category.
Where the variance (the standard deviation as a percentage of the mean value) was high, we have reported the median value.
The p value from the logistical regression reflects a global test for the 3 levels of categorical variable
Table 3.
Wheelchair Data at Baseline
| Characteristics | Parameter | WSTP Group (n = 19) | Control Group (n = 20) | ||
|---|---|---|---|---|---|
|
| |||||
| n | % | n | % | ||
|
| |||||
| Manufacturer | Quickie | 5 | 26 | 7 | 35 |
| Invacare | 9 | 47 | 10 | 50 | |
| Orthofab | 5 | 26 | 1 | 5 | |
| Everest & | 0 | 0 | 2 | 10 | |
| Jennings | |||||
|
| |||||
| Owner | Institution | 10 | 53 | 13 | 65 |
| Province | 1 | 5 | 0 | 0 | |
| User | 8 | 42 | 6 | 30 | |
| Other | 0 | 0 | 1 | 5 | |
|
| |||||
| Frame | Folding | 12 | 63 | 8 | 40 |
| Rigid | 7 | 37 | 12 | 60 | |
|
| |||||
| Seat type | Sling | 17 | 94 | 19 | 100 |
| Rigid | 1 | 6 | 0 | 0 | |
|
| |||||
| Seat height | Adult | 12 | 75 | 15 | 79 |
| Hemi | 4 | 25 | 4 | 21 | |
|
| |||||
| Seat belt | Yes | 1 | 5 | 2 | 10 |
|
| |||||
| Cushion | Yes | 19 | 100 | 20 | 100 |
|
| |||||
| Backrest | Sling | 16 | 89 | 18 | 90 |
| Rigid | 2 | 11 | 2 | 10 | |
|
| |||||
| Backrest height | Low | 1 | 6 | 1 | 5 |
| Scapula | 15 | 88 | 18 | 90 | |
| Shoulder top | 1 | 6 | 1 | 5 | |
|
| |||||
| Adjustable axles | Yes | 16 | 94 | 15 | 88 |
|
| |||||
| Tires | Pneumatic | 18 | 100 | 17 | 85 |
| Solid | 0 | 0 | 3 | 15 | |
|
| |||||
| Brakes | Scissor | 1 | 6 | 1 | 5 |
| Toggle | 17 | 94 | 18 | 95 | |
|
| |||||
| Brake extensions | Yes | 10 | 53 | 7 | 37 |
|
| |||||
| Rear anti-tip devices | Yes | 18 | 95 | 17 | 85 |
|
| |||||
| Footrests | One | 4 | 22 | 4 | 21 |
| Two | 11 | 61 | 9 | 47 | |
|
| |||||
| Removable armrests | Yes | 11 | 58 | 9 | 45 |
|
| |||||
| Backpack | Yes | 3 | 16 | 2 | 10 |
Training Data
The training log was lost from one participant. For the other 18 members of the WSTP group, the mean ± SD number of training sessions was 5.9 ± 1.8. The mean total duration of training was 336 ± 90 minutes spread over a mean of 27 ± 13 days.
Wheelchair Skills Tests
Of the 55 evaluations on participants in the WSTP group (including all T1, T2 and T3 evaluations), 53 (96%) were WSTs and 2 (4%) were WST-Qs. Of the 49 evaluations on participants in the Control group, 42 (86%) were WSTs and 7 (14%) were WST-Qs. The mean ± SD durations of the T1-T2 intervals for the WSTP and Control groups were 51 ± 23 days and 43 ± 17 days (p = 0.126). The mean durations of the T2-T3 intervals for the WSTP and Control groups were 99 ± 12 days and 103 ± 15 days (p = 0.152).
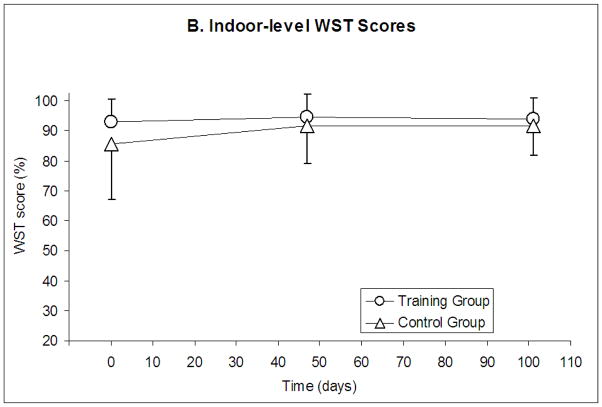
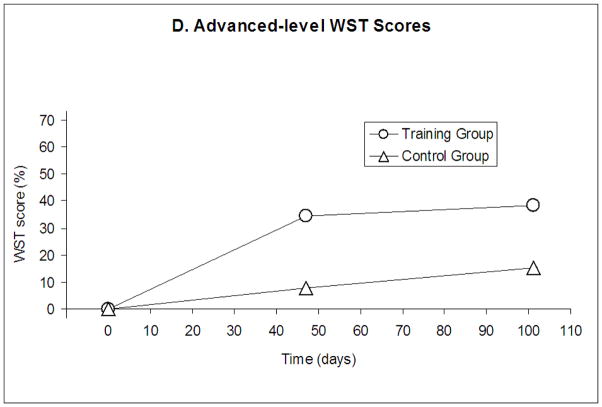
The WST data are shown in Table 4 and illustrated in Figures 2A–D. For the total percentage WST scores at T2 (adjusted for the T1 values), there was a statistically significant difference between the WSTP and Control groups (p = 0.0296). For the Community-level WST subtotal scores, there was also a significant difference between the groups (p = 0.0018). The differences in WST subtotal scores were not statistically significant for the Indoor or Advanced levels. There were no statistically significant changes for either group between T2 and T3 for the total WST scores or the subtotal scores at the Indoor, Community or the Advanced levels using paired t tests. For the ANCOVA models for T3 adjusting for T1, exploring if differences between the WSTP and Control groups were still apparent at T3, the p values were 0.217 for the total WST scores, 0.957 for the Indoor-level WST scores, 0.017 for the Community-level WST scores and 0.209 for the Advanced-level WST scores. None of these p values were statistically significant using the Bonferroni-adjusted α level of 0.005.
Figure 2.
Total and Subtotal WST Scores plotted against time. A. Total WST scores. B. Indoor-level WST scores. C. Community-level WST scores. D. Advanced-level WST scores. For 2A, 2B and 2C, the mean and standard deviation values are shown. For 2D, the median value is shown because the data were non-normal. T1 represents the baseline evaluation, T2 is the evaluation followed training (~47 days after T1). T3 is the follow-up evaluation (~101 days after T2). * indicates statistical significance (p = 0.0296 for Figure 2A and p = 0.0018 for Figure 2C).
Qualitatively there were no major differences in the demographic, clinical, wheelchair-usage or wheelchair data between the drop-outs from the WSTP and Control groups. When the sensitivity analysis was completed for the T2 total WST data, carrying the T1 values forward for T2, the difference between the WSTP and Control groups remained significant (p = 0.013). However, if average values were used for the drop-outs, the difference between the WSTP and Control groups was not significant (p = 0.080). With the T2-T3 sensitivity analysis, there was no statistically significant difference in total WST scores from T2 to T3 for the WSTP (p=0.995) or Control (p=0.688) groups.
The success rates for the individual skills are shown in Table 5. Of the 43 individual skills listed, 15 (35%) skills for the WSTP group and 0 (0%) skills for the Control group met the criterion of a ≥25% improvement between T1 and T2. For the T2-T3 interval, 0 (0%) skills for the WSTP group and 0 (0%) skills for the Control group met the criterion of ≥25% difference between the time periods.
Table 5.
Individual Skill Success Rates
| Skill | Skill Level | WSTP Group | Control Group | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| T1 (n = 19) | T2 (n = 18) | T3 (n = 18) | T1 (n = 20) | T2 (n = 16) | T3 (n = 13) | ||||||||
| n | % | n | % | n | % | n | % | n | % | n | % | ||
| Brakes, apply * | Indoor | 19 | 100 | 16.5 | 92 | 16.5 | 92 | 17 | 85 | 13.5 | 84 | 10.5 | 81 |
| Brakes, release* | Indoor | 19 | 100 | 17 | 94 | 17 | 94 | 17 | 85 | 15 | 94 | 11 | 85 |
| Armrests, move away * | Indoor | 13.5 | 71 | 11 | 61 | 9 | 50 | 12.5 | 63 | 10 | 63 | 6 | 46 |
| Armrests, restore* | Indoor | 11.5 | 61 | 10 | 56 | 8.5 | 47 | 12.5 | 63 | 10 | 63 | 6 | 46 |
| Footrests, move away * | Indoor | 9 | 47 | 7 | 39 | 7 | 39 | 5 | 25 | 2.5 | 16 | 3 | 23 |
| Footrests, restore * | Indoor | 9 | 47 | 7 | 39 | 7 | 39 | 4 | 20 | 2.5 | 16 | 3 | 23 |
| Rolling forward | Indoor | 19 | 100 | 17 | 94 | 18 | 100 | 20 | 100 | 16 | 100 | 13 | 100 |
| Rolling backwards | Indoor | 18 | 95 | 18 | 100 | 17 | 94 | 20 | 100 | 16 | 100 | 13 | 100 |
| Turn in place* | Indoor | 17.5 | 92 | 15.5 | 86 | 16.5 | 92 | 16.5 | 83 | 14 | 88 | 13 | 100 |
| Moving turn, forward* | Indoor | 19 | 100 | 18 | 100 | 18 | 100 | 20 | 100 | 15 | 94 | 13 | 100 |
| Moving turn, backward* | Indoor | 19 | 100 | 18 | 100 | 17.5 | 97 | 19.5 | 98 | 15 | 94 | 13 | 100 |
| Sideways maneuvering* | Indoor | 19 | 100 | 17 | 94 | 17 | 94 | 17 | 85 | 16 | 100 | 13 | 100 |
| Reaching, ground | Indoor | 17 | 90 | 18 | 100 | 18 | 100 | 18 | 90 | 15 | 94 | 13 | 100 |
| Reaching, high object | Indoor | 18 | 95 | 18 | 100 | 18 | 100 | 16 | 80 | 15 | 94 | 12 | 92 |
| Transfer out of wheelchair | Indoor | 17 | 90 | 17 | 94 | 17 | 94 | 16 | 80 | 15 | 94 | 12 | 92 |
| Transfer into wheelchair | Indoor | 15 | 79 | 16 | 89 | 17 | 94 | 15 | 75 | 14 | 88 | 10 | 77 |
| Door, open away | Indoor | 19 | 100 | 18 | 100 | 18 | 100 | 19 | 95 | 16 | 100 | 12 | 92 |
| Door, open toward | Indoor | 19 | 100 | 18 | 100 | 17 | 94 | 17 | 85 | 16 | 100 | 12 | 92 |
| Obstacle 2cm | Indoor | 16 | 84 | 17 | 94 | 17 | 94 | 17 | 85 | 14 | 88 | 11 | 85 |
| Increased rolling resistance, carpet | Indoor | 19 | 100 | 18 | 100 | 18 | 100 | 17 | 85 | 14 | 88 | 11 | 85 |
| Street crossing | Community | 19 | 100 | 17 | 94 | 18 | 100 | 18 | 90 | 13 | 81 | 11 | 85 |
| Fold wheelchair | Community | 3 | 16 | 9 | 50† | 11 | 61 | 6 | 30 | 6 | 38 | 5 | 39 |
| Unfold wheelchair | Community | 4 | 21 | 9 | 50† | 13 | 72 | 6 | 30 | 6 | 38 | 5 | 39 |
| Obstacle 13cm | Community | 3 | 16 | 8 | 44† | 5 | 28 | 3 | 15 | 2 | 13 | 2 | 15 |
| Cross slope* | Community | 19 | 100 | 17.5 | 97 | 17.5 | 100 | 17 | 85 | 13 | 81 | 11 | 85 |
| Increased rolling resistance, gravel | Community | 12 | 63 | 17 | 94† | 15 | 83 | 14 | 70 | 13 | 81 | 9 | 69 |
| Pothole, 15cm | Community | 13 | 68 | 18 | 100† | 17 | 94 | 14 | 70 | 13 | 81 | 10 | 77 |
| Pothole, 30cm | Community | 10 | 53 | 15 | 83† | 14 | 78 | 10 | 50 | 9 | 56 | 7 | 54 |
| Incline 5°, ascent | Community | 18 | 95 | 18 | 100 | 18 | 100 | 16 | 80 | 15 | 94 | 11 | 85 |
| Incline 5°, descent | Community | 18 | 95 | 17 | 94 | 18 | 100 | 16 | 80 | 15 | 94 | 11 | 85 |
| Level change 5cm, ascent | Community | 10 | 53 | 15 | 83† | 15 | 83 | 14 | 70 | 12 | 75 | 10 | 77 |
| Level change 5cm, descent | Community | 10 | 53 | 16 | 89† | 15 | 83 | 14 | 70 | 12 | 75 | 10 | 77 |
| Incline 7.5°, wheelie forwards descent | Advanced | 1 | 5 | 8 | 44† | 8 | 44 | 5 | 25 | 3 | 19 | 5 | 39 |
| Level change 15cm, ascent | Advanced | 0 | 0 | 3 | 17 | 2 | 11 | 2 | 10 | 1 | 6 | 1 | 8 |
| Level change 15cm, descent | Advanced | 0 | 0 | 3 | 17 | 1 | 6 | 2 | 10 | 1 | 6 | 1 | 8 |
| Level change 15cm, wheelie forwards descent | Advanced | 0 | 0 | 1 | 6 | 1 | 6 | 0 | 0 | 0 | 0 | 1 | 8 |
| Wheelie, no-hands rest | Advanced | 3 | 16 | 9 | 50† | 9 | 50 | 7 | 35 | 6 | 38 | 3 | 23 |
| Wheelie, stationary | Advanced | 4 | 21 | 10 | 56† | 10 | 56 | 6 | 30 | 7 | 44 | 6 | 46 |
| Wheelie, rolling forward | Advanced | 3 | 16 | 9 | 50† | 9 | 50 | 4 | 20 | 6 | 38 | 5 | 39 |
| Wheelie, rolling backward | Advanced | 3 | 16 | 8 | 44† | 8 | 44 | 5 | 25 | 6 | 38 | 4 | 31 |
| Wheelie, turn in place* | Advanced | 3 | 16 | 7 | 39 | 9.5 | 53 | 6 | 30 | 6 | 38 | 5 | 39 |
| Wheelie, moving turn forwards* | Advanced | 2.5 | 13 | 8.5 | 47† | 8.5 | 47 | 4 | 20 | 6 | 38 | 5 | 39 |
| Wheelie, moving turn backwards* | Advanced | 3 | 16 | 8 | 44† | 8 | 44 | 5 | 25 | 6 | 38 | 5 | 39 |
Although the left and right sides were scored separately, the mean values of the two are shown, which explains how a non-integer n value is possible.
These skills met the criterion of ≥25% difference in success rates between T1 and T2 in the same group. (No skills met the criterion of ≥25% difference in success rates between T2 and T3 in the same group.)
Safety
There were no adverse incidents during training. However, 3 potentially serious incidents were recorded during the 104 testing sessions (i.e. in 3% of sessions). In the first incident, while attempting to pass over the 30cm pothole, the casters of the participant’s wheelchair dropped into the pothole, the wheelchair tipped forward and the participant slid to the floor. In the second incident, while attempting the 13cm threshold skill, when the rear wheels were on top of the threshold, the participant’s wheelchair tipped forward and he slid to the floor. In the third incident, while she proceeded up a short incline to get onto the cross slope, the wheelchair tipped over backwards and the participant hit her head on the floor. In none of the three cases did any ill effects arise due to the incidents.
DISCUSSION
Our findings are consistent with the prior studies of wheelchair-skills training in general11,12,16 and the WSTP in particular.13–15 There was a 18% relative pre- vs post-training (T1 vs T2) improvement in total WST scores for the WSTP group in the current study, slightly lower than reported earlier.13–15 For the Community-level WST subtotal scores, the WSTP and Control groups improved by 34% and 7%. The differences between the groups were statistically significant for the total WST scores and Community-level subtotal scores, but not for the Indoor- and Advanced-level subtotal scores. The Indoor-level subtotal scores were high at T1, so a ceiling effect may have contributed to our failure to demonstrate a difference due to training. For the Advanced-level subtotal scores, the relatively low but not significant p value of 0.119 suggests that a Type 2 error may have played a role, due to the small sample size.
Whether the improvements in the Control group’s scores were due to good standard care (all were receiving therapy during the T1-T2 period), intrinsic learning or a combination of the two is unknown. Earlier studies of the WSTP13–15 have also shown improvements for control groups. In the interval between the current study and the earlier studies published in 200413 and 2005,14 there may have been an improvement in standard care due to the increased emphasis on wheelchair skills training in the Province of Quebec. Regarding the potential for an intrinsic training effect due to WST testing alone as an explanation for the Control group’s improvement, the questionnaire version of the WST34,35 might have been a better choice as an outcome measure.
The current study, the largest to date on the WSTP, provides a useful replication for the earlier work of MacPhee et al13 and Best et al.14 In addition, like the study by Ozturk and Ucsular15 in Turkey, the current study went beyond those earlier studies in that it was carried out in a different language, culture and health-care setting, and in a site other than that of the WSTP developers. Taken together with other manual wheelchair training studies,11,12,16 it seems reasonable to conclude that the evidence for manual wheelchair skills training is moving gradually beyond efficacy (positive results in an ideal setting) towards effectiveness (positive results in real-world settings).
The evidence in support of the retention of training benefits is a little less clear. As the data in Table 5 on the success rates for individual skills clearly show, there were no clinically significant differences between T2 and T3. Also, as shown in Table 4, the mean or median values at T3 did not decrease in comparison with the T2 values by more than 0.5% for either group. However, the ANCOVA models for T3 total and subtotal WST scores, adjusted for T1, assessing whether differences between the groups could still be seen at T3, showed no statistically significant differences between the 2 groups at 3 months. The p value of 0.017 for the Community-level WST scores was not statistically significant using the Bonferroni-adjusted a level of 0.005. This failure to reach the level of statistical significance, especially at the Community-level WST level, may be a Type 2 error accounted for by the drop-outs between T1 and T3, reducing the power of the analysis. A larger study and/or one with more complete follow-up of enrolled participants will be needed for definitive determination whether gains with this intervention are retained long-term. The trend found in our study for sustained improvements in performance is consistent with the 10-week follow-up used in the uncontrolled study in Afghanistan by Armstrong et al.12
Table 4.
Total and Subtotal WST Scores
| Score | Group | T1 (Baseline) | T2 (Post-training or equivalent) | P values (WSTP vs Control at T2) | T3 (Follow-up) | P values (T2 vs T3) |
|---|---|---|---|---|---|---|
|
| ||||||
| Total | WSTP | 65.4 ± 12.4 | 77.4 ± 13.8 | 0.0296* | 77.4 ± 14.3 | 0.990 |
|
|
|
|||||
| Control | 63.7 ± 20.7 | 69.8 ± 18.4 | 69.7 ± 17.6 | 0.641 | ||
|
| ||||||
| Indoor | WSTP | 92.9 ± 7.9 | 94.5 ± 7.8 | 0.575 | 94.0 ± 7.0 | 0.781 |
|
|
|
|||||
| Control | 85.6 ± 18.5 | 91.8 ± 12.5 | 91.6 ± 9.7 | 0.751 | ||
|
| ||||||
| Community | WSTP | 59.8 ± 20.1 | 80.2 ± 17.8 | 0.0018* | 80.2 ± 19.5 | 1.000 |
|
|
|
|||||
| Control | 60.7 ± 31.1 | 64.7 ± 28.9 | 64.8 ± 33.8 | 0.472 | ||
|
| ||||||
| Advanced | WSTP | Median 0 | Median 34.6 | 0.119 | Median 38.5 | 0.631 |
| Range 0–77 | Range 0–100 | Range 0–100 | ||||
|
|
|
|||||
| Control | Median 0 | Median 7.7 | Median 15.4 | 0.337 | ||
| Range 0–77 | Range 0–77 | Range 0–77 | ||||
Statistically significant at an α level of 0.05 for the primary outcome.
Statistically significant at a Bonferroni-adjusted α level of 0.005.
The mean ± standard deviation values are shown. Where the variance (the standard deviation as a percentage of the mean value) was high, we have reported the median value and the range.
The success rates for the individual skills support the suggestions from the analysis of subtotal WST scores that the improvements due to training were primarily related to skills at the Community and Advanced levels. The data on individual skills will be useful in the future refinement of the WSTP (e.g. by exploring the reasons why training was not effective in improving the success rates of some skills).
Regarding the safety of wheelchair-skills assessment and training, fortunately there were no injuries. However, the 3 incidents that occurred during testing suggest the need for caution. The 2 incidents in which the wheelchair users slid forward out of their wheelchairs suggest that it may be wise to use a seat belt or a second spotter during the assessment of skills that present the risk of forward tips and falls. The rear-tipping incident underlines the importance of caution while the person who is being tested is moving between skills. Using the questionnaire version of the WST34–36 as the outcome measure is preferable from the safety perspective.
Study Limitations
This study had a number of limitations, some of which have already been noted. The sample size was small and the drop-out rate was high, resulting in the study being under-powered for the analysis of subtotal WST scores at the Advanced-skill level and for the assessment of individual skills. There were more drop-outs in the Control group. This probably reflected the fact that they received no benefit (e.g. attention, training) from their participation. Although the results of the sensitivity analyses are reassuring, the differential loss to follow-up (more in the Control group) undermines definitive conclusions about the retention of gains long-term.
Given the nature of the study, it was not possible to blind those in the WSTP group to the training that they received. It is possible that they discussed their training with members of the Control group. This could have served to increase the scores for those in the Control group. Variations among recruitment sites with respect to the participants’ characteristics and the standard care received by participants (about which we should have collected more information) could have contributed to the low study power. However, heterogeneity among rehabilitation centers should be considered an asset with respect to the future generalizability of our findings. There was no placebo intervention, so the participants in the WSTP group may have improved in part due to the extra 5–6 hours of attention that they received in comparison with the Control group. However, the motor skills literature indicates that practice is generally needed to improve motor skills.22
The participants in both groups were not highly experienced in wheelchair use. The changes in the characteristics of some of their wheelchairs (probably to ones that were improvements on those in use at baseline) could have had positive effects on skill performance, but any such bias would have favored the Control group.16 A substantial number of participants acquired new wheelchairs in the T1-T2 and T2-T3 intervals. We do not have information on why the participants got new wheelchairs or in what ways they differed from the original wheelchairs. However, the acquisition of new wheelchairs in both intervals was fairly equally distributed between the WSTP and Control groups so there is no reason to believe that this affected the results. The retention period of 3 months was relatively short. The WST-Q was used instead of the WST for a small number of the assessments and this could have contributed to the variability in the WST scores. Also, WST-Q scores are known to provide slightly higher scores than the WST;34–36 however, any such bias would have favored the Control group.
The net effect of many of the limitations itemized above (e.g. variations in sites, drop-outs, wheelchair changes, Control-group participants potentially hearing about training, use of the WST-Q in some cases) would have been to increase the variability of the WST scores. This would have the effect of reducing the power of the study and thereby making it more difficult to corroborate our hypothesis.
Future studies are needed to address these study limitations and to extend this work. Examples of studies that we believe are needed include studies with a larger sample size, better documentation of standard care, better documentation of wheelchair changes, better blinding, a placebo intervention, more experienced wheelchair users, a longer retention period, better exploration of individual skills, assessment of training of caregivers and assessment of training of powered wheelchair users.
CONCLUSION
WSTP training improves wheelchair skills immediately after training, particularly at the Community-skills level.. Although data on participants who had follow-up at 3-months showed little decline in performance, there was substantive loss to follow-up with a resultant reduction in sample size and study power, such that differences between the WSTP and Control groups were no longer statistically significant. This study provides replication of earlier studies and it provides new data on the important issue of retention.
Acknowledgments
We thank Isabelle Pervieux, OT, MSc, Louise DeSerres, OT, BSc, Frédéric Loiselle, OT, BSc, and Annie Pinsonneault, OT, BSc, for assistance with training and testing, Arthur Goussanou, MSc, for statistical assistance, and the occupational therapists in the sites for assistance with recruitment. We thank Chris Theriault, BEng for his help in setting up the database.
Funding: Supported by the Institute of Aging of the Canadian Institutes of Health Research (grant no SIB-72099), the Quebec Rehabilitation Research Network (grant no 04-05N2-13) and the Fondation pour la recherche sur la moelle epiniere.
LIST OF ABBREVIATIONS
- CRLB
Centre de réadaptation Lucie-Bruneau
- IRGLM
Institut de réadaptation Gingras-Lindsay-de-Montréal
- ITT
Intention to treat
- IUGM
Institut universitaire de gériatrie de Montréal
- RCT
Randomized controlled trial
- SD
Standard deviation
- T1
Evaluation at 1st time period (baseline)
- T2
Evaluation at 2nd time period (post-training)
- T3
Evaluation at 3rd time period (follow-up)
- WSP
Wheelchair Skills Program
- WST
Wheelchair Skills Test, objective version
- WST-Q
Wheelchair Skills Test, questionnaire version
- WSTP
Wheelchair Skills Training Program
Footnotes
Spreadsheet. Excel Version 2003. Microsoft Corporation, 320 Matheson Blvd W, Mississauga, ON, Canada L5R 3R1.
Statistical software. SAS Version 9.2. SAS Institute Inc., 00 SAS Campus Drive Cary, NC, USA 27513-2414.
Presented in part at: 9th European Conference for the Advancement of Assistive Technology, San Sebastian, Spain, October 3–5 2007.
Reprints: Not available from the authors.
Clinical Trials Registry Number: NCT00400244 (clinicaltrials.gov).
Authors’ financial disclosure: No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the author(s) or upon any organization with which the author(s) is/are associated.
List of SuppliersaSpreadsheet. Excel Version 2003. Microsoft Corporation, 320 Matheson Blvd W, Mississauga, ON, Canada L5R 3R1. bStatistical software. SAS Version 9.2. SAS Institute Inc., 00 SAS Campus Drive Cary, NC, USA 27513-2414
References
- 1.Rousseau-Harrison K, Rochette A, Routhier F, Dessureault D, Thibault F, Cote O. Perceived impacts of a first wheelchair on social participation. Disabil Rehabil Assist Technol. 2011:1–8. doi: 10.3109/17483107.2011.562957. Early Online. [DOI] [PubMed] [Google Scholar]
- 2.McClure LA, Boninger ML, Oyster ML, Williams S, Houlihan B, Lieberman JA, Cooper RA. Wheelchair repairs, breakdown, and adverse consequences for people with traumatic spinal cord injury. Arch Phys Med Rehabil. 2009;90:2034–8. doi: 10.1016/j.apmr.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 3.Collinger JL, Impink BG, Ozawa H, Boninger ML. Effect of an intense wheelchair propulsion task on quantitative ultrasound of shoulder tendons. PM&R. 2010;2:920–5. doi: 10.1016/j.pmrj.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 4.Akbar M, Balean G, Brunner M, Seyler TM, Bruckner T, Munzinger J, Grieser T, Gerner HJ, Loew M. Prevalence of rotator cuff tear in paraplegic patients compared with controls. J Bone Joint Surg Am. 2010;92:23–30. doi: 10.2106/JBJS.H.01373. [DOI] [PubMed] [Google Scholar]
- 5.Calder CJ, Kirby RL. Fatal wheelchair-related accidents in the USA. Amer J Phys Med Rehabil. 1990;69:184–90. doi: 10.1097/00002060-199008000-00003. [DOI] [PubMed] [Google Scholar]
- 6.Kirby RL, Ackroyd-Stolarz SA, Brown MG, Kirkland SA. Wheelchair-related accidents caused by tips and falls among non institutionalized users of manually propelled wheelchairs in Nova Scotia. Amer J Phys Med Rehabil. 1994;73:319–30. doi: 10.1097/00002060-199409000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Xiang H, Chany A-M, Smith GA. Wheelchair related injuries treated in US emergency departments. Injury Prevention. 2006;12:8–11. doi: 10.1136/ip.2005.010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nelson AL, Groer S, Palacios P, Mitchell D, Sabharwal S, Kirby RL, Gavin-Dreschnack D, Powell-Cope G. Wheelchair-related falls in veterans with spinal cord injury residing in the community: a prospective cohort study. Arch Phys Med Rehabil. 2010;91:1166–73. doi: 10.1016/j.apmr.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 9.Berg K, Hines M, Allen S. Wheelchair users at home: few home modifications and many injurious falls. Am J Public Health. 2002;92:48. doi: 10.2105/ajph.92.1.48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.World Health Organization. [Accessed December 14, 2011];Guidelines on the provision of wheelchairs in less resourced settings. 2008 Aug; http://www.who.int/disabilities/publications/technology/wheelchairguidelines/en. [PubMed]
- 11.Bullard S, Miller SE. Comparison of teaching methods to learn a tilt and balance wheelchair skill. Precept Mot Skills. 2001;93:131–8. doi: 10.2466/pms.2001.93.1.131. [DOI] [PubMed] [Google Scholar]
- 12.Armstrong W, Reisinger KD, Smith WK. Evaluation of CIR-Whirlwind wheelchair and service provision in Afghanistan. Disabil Rehabil. 2007;29:935–48. doi: 10.1080/09638280701240615. [DOI] [PubMed] [Google Scholar]
- 13.MacPhee AH, Kirby RL, Coolen AL, Smith C, MacLeod DA, Dupuis DJ. Wheelchair skills training program: a randomized clinical trial on wheelchair users undergoing initial rehabilitation. Arch Phys Med Rehabil. 2004;85:41–50. doi: 10.1016/s0003-9993(03)00364-2. [DOI] [PubMed] [Google Scholar]
- 14.Best KL, Kirby RL, Smith C, MacLeod DA. Wheelchair skills training for community-based manual wheelchair users: a randomized controlled trial. Arch Phys Med Rehabil. 2005;86:2316–23. doi: 10.1016/j.apmr.2005.07.300. [DOI] [PubMed] [Google Scholar]
- 15.Ozturk A, Ucsular FD. Effectiveness of a wheelchair skills training programme for community-living users of manual wheelchairs in Turkey: a randomized controlled trial. Clin Rehabil. 2011;25:416–24. doi: 10.1177/0269215510386979. [DOI] [PubMed] [Google Scholar]
- 16.Hoenig H, Landerman LR, Shipp KM, Pieper C, Pieper C, Richardson M, Pahel N, George L. A clinical trial of rehabilitation expert clinician versus usual care for providing manual wheelchairs. J Am Geriatr Soc. 2005;53:1712–20. doi: 10.1111/j.1532-5415.2005.53502.x. [DOI] [PubMed] [Google Scholar]
- 17.Kilkens OJE, Post MWM, Dallmeijer AJ, van Asbeck FWA, van der Woude LHV. Relationship between manual wheelchair skill performance and participation of persons with spinal cord injuries 1 year after discharge from inpatient rehabilitation. J Rehab Res Dev. 2005;42:65–74. doi: 10.1682/jrrd.2004.08.0093. [DOI] [PubMed] [Google Scholar]
- 18.van Zeltzen JM, de Groot S, Post MWM, Slootman JR, van Bennekom CAM, van der Woude LHV. Return to work after spinal cord injury. Am J Phys Med Rehabil. 2009;88:47–56. doi: 10.1097/PHM.0b013e31818e6140. [DOI] [PubMed] [Google Scholar]
- 19.Jenkins S. Wheelchair training provision by NHS wheelchair services. London, UK: Whizz-Kidz; 2002. [Google Scholar]
- 20.Karmarkar AM, Collins DM, Wichman T, Franklin A, Fitzgerald SG, Dicianno BE, Pasquina PF, Cooper RA. Prosthesis and wheelchair use in veterans with lower-limb amputation. JRRD. 2009;46:567–76. doi: 10.1682/jrrd.2008.08.0102. [DOI] [PubMed] [Google Scholar]
- 21.Salatin B, Rice I, Teodorski E, Ding D, Cooper RA. A survey of outdoor powered wheelchair driving. Proc Annual Conf RESNA; Las Vegas. June 26–30, 2010. [Google Scholar]
- 22.Dalhousie University. [Accessed December 14, 2011];The Wheelchair Skills Program. 2011 Available from: www.wheelchairskillsprogram.ca.
- 23. [Accessed December 14, 2011];Guide de la version canadienne-française du Wheelchair Skills Program (WSP) Version 3.2. Available at: http://www.wheelchairskillsprogram.ca/fre/manual.htm.
- 24. [Accessed December 14, 2011];Randomization table. Available at www.randomization.com.
- 25.Routhier F, Kirby RL, Demers L, Vincent C, Westwood D. Translation of the Wheelchair Skills Program into French: an iterative methodology. RESNA 2005; 28th International Conference on Technology & Disability: Research, Design and Practice; Atlanta, GA, USA. June 23–27, 2005. [Google Scholar]
- 26.Routhier F, Kirby RL, Demers L. Translation of the Wheelchair Skills Program into Canadian-French: an internationalization experience. 21st World Congress of Rehabilitation International; Québec City, Québec, Canada. August 25–28, 2008; p. 130. Abstract 44.3. [Google Scholar]
- 27.Routhier F, Kirby RL. Linguistic and cultural validation with an Acadian population of a French-Canadian version the Wheelchair Skills Program: an observational and descriptive study. RESNA 2009; 32th International Conference on Technology and Disability: Research, Design and Practice; New Orleans, Louisiana, USA. June 23–27, 2009. [Google Scholar]
- 28.Kilkens OJ, Post MW, Dallmaijer AJ, Seelen HA, van der Woude LH. Wheelchair skills tests: a systematic review. Clin Rehabil. 2003;17:418–30. doi: 10.1191/0269215503cr633oa. [DOI] [PubMed] [Google Scholar]
- 29.Fliess-Douer O, Vanlandewijck YC, Manor GL, van der Woude LH. A systematic review of wheelchair skills tests for manual wheelchair users with a spinal cord injury: towards a standardized outcome measure. Clin Rehabil. 2010;24:867–86. doi: 10.1177/0269215510367981. [DOI] [PubMed] [Google Scholar]
- 30.Kirby RL, Swuste J, Dupuis DJ, MacLeod DA, Monroe R. Wheelchair Skills Test: pilot study of a new outcome measure. Arch Phys Med Rehabil. 2002;83:10–18. doi: 10.1053/apmr.2002.26823. [DOI] [PubMed] [Google Scholar]
- 31.Kirby RL, Dupuis DJ, MacPhee AH, Coolen AL, Smith C, Best KL, Newton AM, Mountain AM, MacLeod DA, Bonaparte JP. The Wheelchair Skills Test (version 2. 4): measurement properties. Arch Phys Med Rehabil. 2004;85:794–804. doi: 10.1016/j.apmr.2003.07.007. [DOI] [PubMed] [Google Scholar]
- 32.Routhier F, Demers L, Kirby RL, Pervieux I, Depa M, De Serres L, Loiselle F, Dessureault D. Inter-rater and test-retest reliability of the French-Canadian Wheelchair Skills Test (Version 3.2): preliminary findings. Proc Ann Meeting RESNA; Phoenix, AZ. June 15–19; 2007. [Google Scholar]
- 33.Lindquist NJ, Loudon PE, Magis TF, Rispin JE, Kirby RL, Manns PJ. Reliability of the performance and safety scores of the Wheelchair Skills Test Version 4. 1 for manual wheelchair users. Arch Phys Med Rehabil. 2010;91:1752–7. doi: 10.1016/j.apmr.2010.07.226. [DOI] [PubMed] [Google Scholar]
- 34.Newton AM, Kirby RL, MacPhee AH, Dupuis DJ, MacLeod DA. Evaluation of manual wheelchair skills: is objective testing necessary or would subjective estimates suffice? Arch Phys Med Rehabil. 2002;83:1295–9. doi: 10.1053/apmr.2002.33071. [DOI] [PubMed] [Google Scholar]
- 35.Mountain AD, Kirby RL, Smith C. The Wheelchair Skills Test: validity of an algorithm-based questionnaire version. Arch Phys Med Rehabil. 2004;85:416–23. doi: 10.1016/s0003-9993(03)00427-1. [DOI] [PubMed] [Google Scholar]
- 36.Rushton P, Kirby RL, Miller WC. Wheelchair Skills Test Version 4.1: Comparison of total percentage scores for the objective and questionnaire versions. Proceedings of the Annual Meeting of RESNA, Toronto; June 5–8, 2011; Toronto, ON, Canada. (Abstract #69561) [Google Scholar]
- 37.Schulz KF, Altman DG, Moher D for the CONSORT Group. CONSORT 2010 Statement: Updated guidelines for reporting parallel group randomized trials. Ann Int Med. 2010;152:1–7. [PMC free article] [PubMed] [Google Scholar]