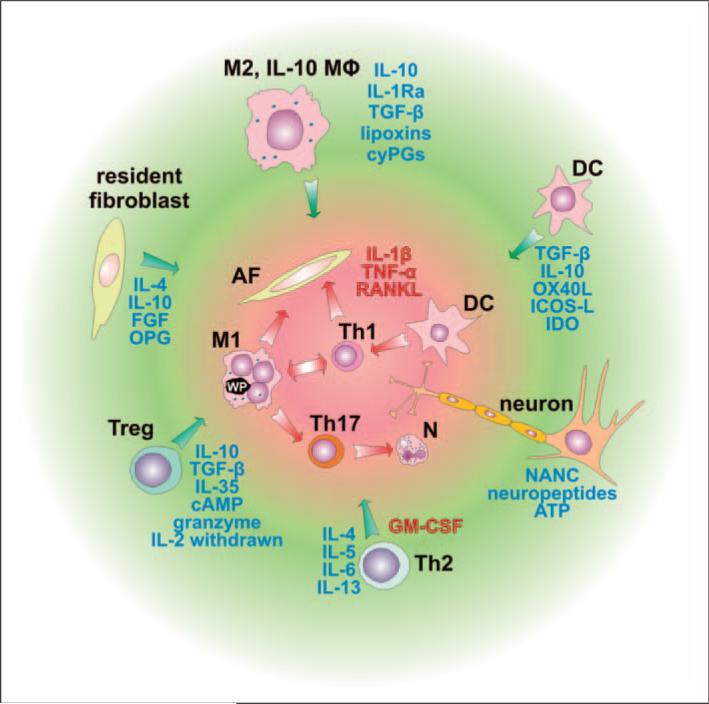
Figure 3.
Cell populations involved in the suppression of the inflammatory response. Cells involved in the inflammatory reaction, such as classically-activated macrophages (M1), Th1 cells, Th17 cells, activated fibroblasts, dendritic cells (DC) and neutrophils, contribute to bone resorption mostly through IL-1β, TNF-α and receptor activator of NF-κB ligand (RANKL) signaling. Activity of the above-mentioned cells is controlled and suppressed by several factors secreted predominantly from immune cells represented by macrophages stimulated through the IL-4, IL-13, α-tocopherol, IgG-containing immune complexes (IC), apoptotic cells or prostaglandins, leading to the ‘alternatively activated’ healing phenotype (M2), from regulatory IL-10-secreting macrophages (IL-10 MΦ), DCs, regulatory T cells (Treg) and Th2 cells. Depending on the modulating properties of signals they receive, DCs could play a pro-inflammatory role by activating pro-inflammatory Th1 or Th17 cells, or an anti-inflammatory role by activating regulatory T cells (Treg) that suppress immune reactions. Furthermore, inflammatory cells could be suppressed by resident fibroblasts and neurons. AF, activated fibroblast; cyPGs, cyclopentenone prostaglandins; GM-CSF, granulocyte-macrophage colony stimulating factor; OPG, soluble receptor for RANKL – osteoprotegerin; FGF, fibroblast growth factor; OX40L, tumor necrosis factor ligand superfamily member 4; ICOS-L, inducible T-cell co-stimulator ligand, IDO, indolamine 2,3 dioxygenase; NANC, non-adrenergic non-cholinergic neurotransmitters. Anti-inflammatory factors leading to bone remodeling are in blue, pro-inflammatory factors or those associated with bone resorption are in red.