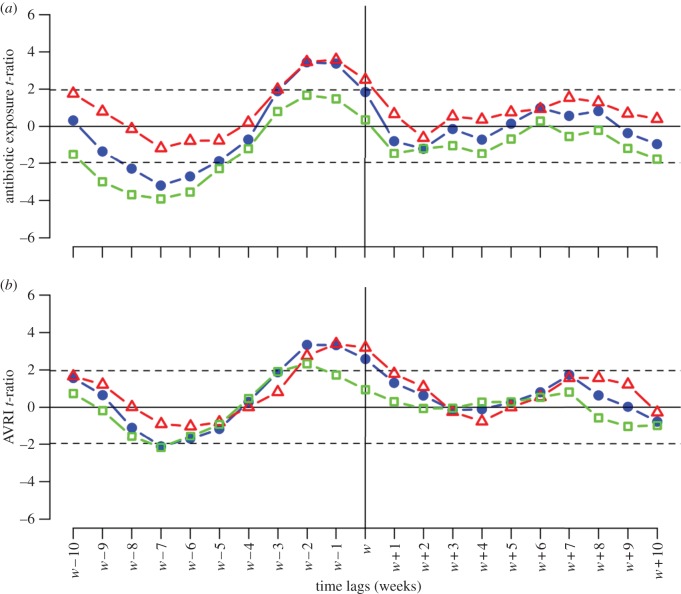
Figure 3.
Statistical association between SPMI and AVRI or antibiotic exposure. Antibiotic and AVRI time series were detrended, and seasonality removed to create ‘residual time series’. Lagged regression coefficient t-ratios between numbers of meningitis cases and residual antibiotic or residual AVRI are plotted for all lags k between weeks −10 and +10. (a) SPMI association with antibiotics. Total (blue circles) and resistant meningitides (red triangles) are positively significantly linked to antibiotic use at weeks −1 and −2. Long-term relationships were observed between total and susceptible meningitides (green squares) and antibiotic use, with a negative significant link for weeks −5 to −8, with a peak at −7. (b) SPMI association with AVRI. Regardless of strain susceptibility, increased SPMI was significantly associated with high AVRI incidence during the same and the preceding 2 weeks, indicating positive short-term dependency. Negative long-term dependency (week −7) was observed for total and susceptible meningitides, but associations were only marginally significant. Like the antibiotics analysis, resulting t-ratios were markedly asymmetric.