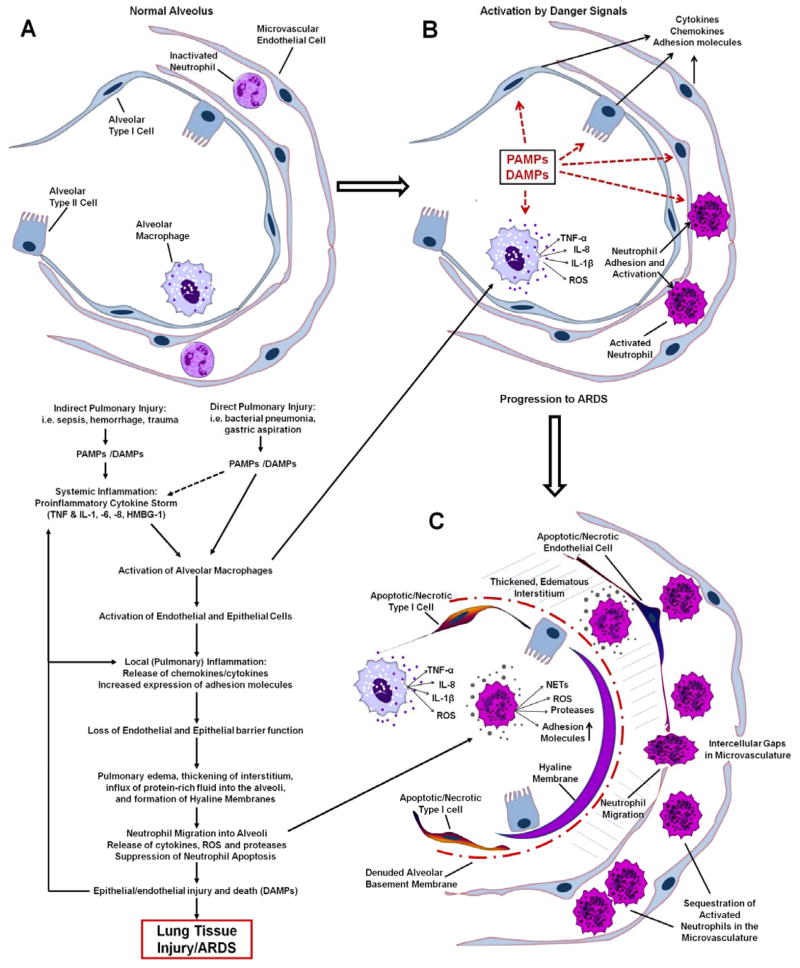
Figure 1.
Schematic illustrating some of the major events in the pathogenesis of ARDS. A: Top left panel: Normal alveolus with type I and type II epithelial cells, resident alveolar macrophage, capillary endothelial cells and inactivated circulating neutrophils. B: Top right panel: Activation of the innate immune system by indirect or direct lung injury (PAMPs/DAMPs) results in the release of proinflammatory cytokines and ROS by alveolar macrophages. Lung endothelial and epithelial activation further amplifies expression of cytokines and adhesion molecules that promote neutrophil adhesion and activation. C: Bottom right panel: The proinflammatory cascade drives robust neutrophil migration into a thickened, edematous interstitium and also into the alveolar space. Release of toxic mediators by recruited inflammatory cells drives cell death and lung tissue injury. Loss of epithelial barrier function results in flooding of the alveoli and hyaline membrane formation, thus impairing gas exchange.