Abstract
Introduction: Community-acquired pneumonia (CAP) is among the common diseases that causes illness and death world-wide. Limited data is available for the treatment of patients with CAP and/or medical outcome of CAP patients in Pakistan. This cross-sectional and prospective study was done to determine etiology of CAP patients and to evaluate the therapeutic effects of antibiotics commonly used in treating CAP patients in two different inner-city hospitals, Pakistan. Methods: The study was conducted on 200 hospitalized patients presenting clinical and radiographic evidences of CAP. The patients were assessed for the causative pathogen and their prescriptions were analyzed for the management and treatment of CAP and associated symptoms of pneumonia. Finally the medical outcomes were evaluated. Results: On establishing the microbial etiology of pneumonia among different CAP causing pathogens, K. pneumoniae was found to be the most identified causative agent (30%) followed by S. pneumoniae (23%). Majority of the patients received cephalosporin antibiotics (80%) followed by aminoglycosides (65%) and penicillins (50%) either as monotherapy or combination treatment. Therapeutic success was observed to occur in majority of the patients. The recovery of CAP patients occurred probably because they received antibiotics which are recommended by WHO and American Thoracic Society. Another reason for successful therapeutic outcome was found to be the significant patient compliance for treatment. Conclusion: There is a great need for such types of investigational studies to be conducted in developing countries which may guide the empirical therapy and help in defining proper treatment guidelines.
Keywords: Aminoglycosides, CAP Patients, Combination Therapy for CAP, Empirical Therapy, Patient Compliance, Respiratory Tract Infections
Introduction
Community-acquired pneumonia (CAP) is considered among critical respiratory tract infections that account for millions of death globally every year.1,2 CAP has been long considered as a leading cause of illness and mortality globally.3 Most of the patients diagnosed for CAP are usually hospitalized and some may also require to be treated during intensive care.4,5 S. pneumonia is considered to be the leading agent causing CAP, however the causative pathogens may differ depending on various factors such as age and ecological aspects. This variation of pathogen and unknown microbial cause usually ends up with initial empirical antibiotic therapy.6 Though different established guidelines for the treatment of CAP3,7-9, have suggested few antimicrobial regimen for CAP patients, further studies should vitally be conducted for determining the major causative pathogens and the most effective therapy against CAP especially in developing countries as they might help developing appropriate therapeutic regimen against CAP. For many years, numerous studies have been performed to evaluate the etiology and treatment of CAP,10-12 however, prospective studies regarding the etiology and treatment protocols followed to manage and treat patients with CAP in Pakistan, have been limited.13 In Pakistan, most of the patients with respiratory tract infections are usually treated empirically as for CAP, amoxicillin-clavulanate (2 g PO q12h), cefotaxime (1 g IV q8h or ceftriaxone 1 g IV q24h), ciprofloxacin and levofloxacin (levofloxacin 750 mg IV every 24 h) are prescribed as empirical therapy. Although few efficient studies have been done recently, still there are numerous concerns relating the disease conditions, hospital patient care, biodisposition/serum profile studies,14,15 use of natural products16-18 and synthetic proteins19-24 in developing countries that critically need to be addressed and managed. As CAP is also among these critical conditions, thereby the purpose of this study was to determine the causative pathogens of CAP in Pakistan and to perform a comparative evaluation of the antibiotic and associated therapy used in hospitals to treat patients suffering from CAP. We conducted this study on hospitalized CAP patients to provide the information collected by the investigational audit on the antibiotic treatment practice along with determining the microbial etiology of CAP in Pakistan. In future, our study may contribute in developing an appropriate antimicrobial regimen for the better management of CAP in Pakistan.
Materials and methods
Method
This study was conducted at two hospitals; Jinnah Hospital and Combined Military Hospital (CMH) in Lahore, Pakistan. The relevant doctors of the hospital general wards approved the study protocol and allowed for further proceedings. The study design included: patient data collection, evaluation of patient careprocesses, determination of microbial etiology, assessment of prescribed medication/antibiotics and assessment of medical outcomes of patients under study.
Patient selection /Inclusion criteria
The study was conducted by enrolling 200 hospitalized patients (100 males and 100 females) in general ward presenting clinical and radiographic evidences of CAP. These patients were then further examined to determine if they met the study inclusion criteria. The inclusion criteria comprised of the diagnostic symptoms recommended by American Thoracic Society25 as follows: 1) patients having physical symptoms such as bronchial wheezing and other related symptoms like cough, sputum and chest pain, 2) Confirmed clinical diagnosis of pneumonia evidenced by radiographs showing pulmonary infiltration/consolidation.
However, patients who have been included in any of the previous studies in last three months and/or were pregnant or lactating were excluded from this study.
Data collection
Data were collected by taking patient history and extracting the clinical findings and treatment regimen from their medical records/prescriptions. The patient history related to their vital signs, clinical manifestations, presence of co-existing disease, use of any drug before being hospitalized, and the treatment which the patients were receiving for CAP after being hospitalized (including antibiotics/other drugs, dose, frequency) was collected. The chest radiographical images and their results were also collected. Moreover, the data related to the causative pathogen were also collected by analyzing the records of laboratory results obtained by patient’s specimens. The medical outcomes of treated patients were also recorded to be further assessed.
Patient’s specimen for causative pathogen
The blood cultures, sputum samples and nasal swabs were taken as patient specimen to perform the microbial laboratory tests in order to determine the pathogen responsible for causing CAP.
Microbial etiology of pneumonia
To determine the etiology of CAP, that is, which pathogen is the major cause of CAP in Pakistan, the prescription/patient record containing the laboratory results indicating causative pathogen of CAP were collected, evaluated and compiled. The microbial culture and identification was performed according to hospital protocol.
Assessment of medical outcomes
The patient’s medical outcome was estimated by observing the associated physical symptoms such as fever and bronchial sounds. Improvement in chest radiographs was also observed. Moreover, therapeutic success was declared when the patients recovered from all CAP-associated symptoms and did not receive additional antimicrobial therapy other than the prescribed one.
Statistical analysis
A mean age comparison was drawn by Student’s T-Test. Data were summarized as means ± standard deviation. One-way analysis of variance (ANOVA) was used to test the differences and p<0.05 was considered to indicate statistical significance.
Results
Patient’s characteristics
Two hundred hospitalized CAP patients with a mean age of 44.8 ± 17.0 enrolled in this study were examined and their vital signs were observed throughout the study. The details of recorded vital signs are shown in Table 1. Moreover, smoking status was recorded positive for 39% of patients, and approximately 30% of the studied patients did not receive any pneumococcal vaccination. Among the total number of CAP patients under study, empirical antibiotic therapy was given to approximately 40% patients before being admitted and properly diagnosed for pneumonia.
Table 1. Vital signs of pneumonia patients .
| Vital Signs | Values |
| Age | 44.8 ± 17.04 |
| Body weight | 68.2 ± 20.93 |
| BP Systolic (mm Hg) | 127.05 ± 22.86 |
| BP Diastolic (mm Hg) | 75.5 ± 19.3 |
| Pulse Rate (/min) | 93.45 ± 36.73 |
| Respiratory Rate (/min) | 32.55 ± 18.87 |
Microbial etiology of pneumonia
On microbial laboratory testing of specimen obtained from patients, K. pneumoniae was found to be the most frequent identified agent to be responsible for causing CAP in about 60 patients (30%) out of two hundred patients, followed by S. pneumoniae that contributed in causing CAP in 46 patients (23%). Gram-negative diplococci and M. pneumoniae were found responsible for causing CAP in 34 (17%) and 22 (11%) patients, respectively, as shown in Fig. 1. However, there were 10 (5%) cases of unidentified microbial pathogen.
Fig. 1 .
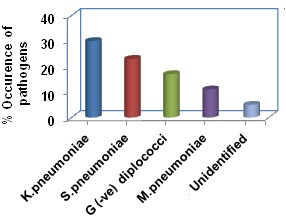
Percentage of causative pathogens identified in 200 CAP patients
Prescribed treatment
As soon as the microbial diagnosis was established for the CAP patients enrolled in this study, patients started to receive clinical course of antibiotic treatment either as a single antibiotic (Fig. 2) or in combination with other antimicrobials (Fig. 3). Majority of the patients received cephalosporin antibiotics contributing for 80% antibiotic treatments. The other frequently used antibiotics were aminoglycosides (65%) and penicillins (50%). Quinolones and macrolides were used as 25 and 20%, respectively, to treat CAP patients; however, the remaining population received either tetracycline (15%) or fluoroquinolone (10%). Majority of the patients on combination therapy received either a combination of cephalosporin and aminoglycosides (55%) or of cephalosporin, penicillin and aminoglycosides (25%). The other combinations of antibiotics used to treat CAP patients were aminoglycosides and penicillin (15%), cephalosporin and penicillin (10%), and macrolides and penicilines (5%). The details of combinations of antibiotics used as treatment protocol are shown in Fig. 3. The prescribing ratio of NSAIDs and glucocorticoids were 80 and 15% respectively; however, combination of NSAIDs and glucocorticoids (10%) was also prescribed.
Fig. 2.
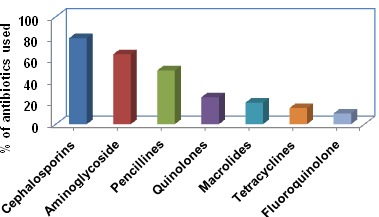
Percentage usage of different antibiotics prescribed during the treatment of 200 patients
Fig. 3.
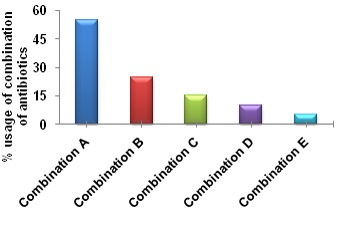
Percentage usage of combination of different antibiotics prescribed during the treatment of 200 pneumonia patients. Combination A: Cephalosporins + Aminoglycosides; Combination B: Cephalosporins + Aminoglycosides + Penicilines; Combination C: Aminoglycosides + Penicilines; Combination D: Cephalosporins + Penicilines; Combination E: Macrolides + Penicilines.
Medical outcomes
Therapeutic success was observed to occur in majority of the patients. Cephalosporins as monotherapy as well as in combination with other antimicrobials were found to be associated with the highest success rate relating to the medical outcome in CAP patients treated. This was followed by the combinations of aminoglycosides plus cephalosporins, aminoglycosides and penicillines. Similarly on the basis of their successful therapeutic outcomes, cephalosporins, aminoglycosides and penicilines were also prescribed as monotherapy other than combination therapy to most of the patients as depicted in Fig. 2.
Discussion
From many years ago, different guidelines for the proper management of pneumonia have been developed 3-7-9, Despite this rapid progress regarding various strategies and antibacterial treatment, the considerable cases of pneumonia have been associated with the high rate of mortality worldwide especially in developing countries. This is the case with Pakistan and only limited studies26-28 have been conducted to evaluate the implementation of these guidelines and treatment protocols including the process of care, diagnostic measurements, use of recommended antibiotics and practice of empirical antimicrobial therapy for CAP patients. This study was conducted on 200 hospitalized patients of CAP in the general wards of two public hospitals in Lahore, Pakistan, to evaluate the major causative pathogens, management/treatment protocol and implementation of approved guidelines for pneumonia. To the best of our knowledge, a very few studies29-31 have been done in Pakistan for the evaluation of the major microbial cause of CAP among patients. In this study, laboratory analysis of patient’s specimen was done to verify the causative pathogen and K. pneumoniae was found to be the main microbial agent in most of the patients followed by S. pneumoniae. The contribution of other microbial pathogens in causing CAP in patients under this study is shown in Fig. 1. However, pathogens differ among various studies performed in different areas or countries.32,33 This variation in the microbial etiology for CAP found among various investigational studies conducted in different countries might be due to the divergence in laboratory tests and environmental/epidemic causes. After the verification of microbial etiology, prescribing measures for antibiotics were evaluated by analyzing and comparing patients’ prescription and results of microbial etiology. Cephalosporin was found to be the most prescribed antibiotic as monotherapy and in combination with either aminoglycosides or penicilines (Fig. 2 and Fig. 3). The most probable reason for active prescription of cephalosporins was found to be the success rate in terms of positive patient’s medical outcome. Similarly, cephalosporins in other recent studies34,35 have also shown to be one of the most effective therapies in treating CAP and reducing cases of mortality. Besides, an additional interesting finding of the current study was that no case of severe consequences or mortality was observed if any patient did receive empirical therapy prior to the confirmation microbiological data for etiology of CAP. Moreover, a positive medical outcome was estimated by assessing the resolution of associated physical symptoms and no need for further antibiotic treatment was observed in majority of the CAP patients under study after they received the prescribed treatment.
Conclusion
In summary, this study was conducted on 200 hospitalized CAP patients for the evaluation of microbial etiology, implementation/compliance of approved CAP-guidelines and rate of success in terms of patient medical outcome. The most appealing results from present study are the therapeutic success that was observed to occur in majority of the patients. The recovery of CAP patients occurred probably because they received antibiotics which are recommended drugs by WHO and American Thoracic Society. Another reason for successful therapeutic outcome was found to be the significant patient compliance towards treatment. Thereby, this study shows that proper implementation of developed guidelines relating the prescription of antibiotics and process of patient care can surely contribute in improving the management of CAP in developing countries.
Acknowledgment
Authors did not receive any grant for the accomplishment of this article. Authors would like to admire Dr. Javed Iqbal from CMH, Dr. Wasim Shafqat and Dr. Arif Qayyum from Jinnah Hospital for their cooperation and provision of facilities for this study.
Ethical issues
The relevant doctors of the hospital general wards approved the study protocol and allowed for further proceedings.
Competing interests
Authors declare that they have no conflict of interests.
References
- World Health Organization, WHO. Burden of Disease Project. Geneva: World Health Organization. 2005.
- Mogyoros M. Challenges of managed care organizations in treating respiratory tract infections in an age of antibiotic resistance. Am J Manag Care . 2001;7:S163–S169. [PubMed] [Google Scholar]
- American Thoracic Society. American Thoracic SocietyGuidelines for the management of adults with community-acquired pneumoniaDiagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Respir Crit Care Med . 2001;163:1730–54. doi: 10.1164/ajrccm.163.7.at1010. [DOI] [PubMed] [Google Scholar]
- Ewig S, Ruiz M, Mensa J, Marcos MA, Martinez JA, Arancibia F. et al. Severe community-acquired pneumoniaAssessment of severity criteria. Am J Respir Crit Care Med . 1998;158:1102–8. doi: 10.1164/ajrccm.158.4.9803114. [DOI] [PubMed] [Google Scholar]
- Oosterheert JJ, Bonten MJ, Hake E, Schneider MM, Hoepelman AI. Severe community-acquired pneumonia: what’s in a name? . Curr Opin Infect Dis . 2003;16: 153– 9. doi: 10.1097/00001432-200304000-00012. [DOI] [PubMed] [Google Scholar]
- Shefet D, Robenshtock E, Paul M, Leibovici L. Empiric antibiotic coverage of atypical pathogens for community acquired pneumonia in hospitalized adults. Cochrane Database Syst Rev . 2005;2:CD004418. doi: 10.1002/14651858.CD004418.pub2. [DOI] [PubMed] [Google Scholar]
- British Thoracic Society. Guidelines for the management of community acquired pneumonia in adults. Thorax . 2001;56:1–64. doi: 10.1136/thorax.56.suppl_4.iv1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartlett JG, Dowell SF, Mandell LA, File TM, Musher DM, Fine MJ. Practice guidelines for the management of community acquired pneumonia in adults. Clin Infect Dis . 2000;31:347–82. doi: 10.1086/313954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mandell LA, Marrie TJ, Grossman RF, Chow AW, Hyland RH. Canadian Community-acquired Pneumonia Working Group. Canadian guidelines for the initial management of community-acquired pneumonia: an evidence-based update by the Canadian Infectious Diseases Society and the Canadian Thoracic Society. Clin Infect Dis . 2000;31:383–421. doi: 10.1086/313959. [DOI] [PubMed] [Google Scholar]
- Aubier M, Verster R, Regamey C, Geslin P, Vercken JB. Sparfloxacin European Study Group. Once-daily sparfloxacin versus high-dosage amoxicillin in the treatment of community-acquired, suspected pneumococcal pneumonia in adultsSparfloxacin European Study Group. Clin Infect Dis . 1998;26:1312–20. doi: 10.1086/516366. [DOI] [PubMed] [Google Scholar]
- Tremolieres F, de Kock F, Pluck N, Daniel R. Trovafloxacin versus high-dose amoxicillin (1g three times daily) in the treatment of community-acquired bacterial pneumonia. Eur J Clin Microbiol Infect Dis . 1998;17:447–53. doi: 10.1007/BF01691581. [DOI] [PubMed] [Google Scholar]
- Donowitz G, Mandell G. Acute Pneumonia. In: Mandell GL, Bennet JE, Dolin R editor(s). Principles and Practice of Infectious Diseases. 5th Edition. Vol. 1, USA: Churchill Livingstone. 2000;717-743.
- Qazi SA. Antibiotic strategies for developing countries: Experience with acute respiratory tract infections in Pakistan. Clin Infect Dis . 1999;28:214–8. doi: 10.1086/515124. [DOI] [PubMed] [Google Scholar]
- Parveen A, Akash MSH, Rehman K, Tariq M, Zahra N, Iqbal T. Biodisposition kinetics of isoniazid in healthy females. J App Pharm . 2012;3:676–81. [Google Scholar]
- Qadir MI, Saleem M, Khalid SH, Malik SA, Massud A, Ali M. et al. Plasma lipid alterations in leukemia patients. J App Pharm . 2011;1:159–64. [Google Scholar]
- Lei Y, Zhang S, Fang L, Akash MSH, Shi W, Sun K. et al. A sensitive and specific enzyme immunoassay for detecting tartrazine in human urinary samples. Anal Methods . 2013;5:925–30. [Google Scholar]
- Akash MSH, Rehman K, Rasool F, Sethi A, Abrar MA, Irshad A. et al. Alternate therapy of Type 2 diabetes mellitus (T2DM) with Nigella (Ranunculaceae) J Med Plants Res . 2011;5:6885–9. [Google Scholar]
- Rehman K, Akash MSH, Azhar S, Khan SA, Abid R, Waseem A. et al. A biochemical and histopathologic study showing protection and treatment of gentamicin-induced nephrotoxicity in rabbits using vitamin c. Afr J Tradit Complement Altern Med . 2012;9:360–5. doi: 10.4314/ajtcam.v9i3.9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akash MSH, Shen Q, Rehman K, Chen S. Interleukin-1 receptor antagonist: A new therapy for type 2 Diabetes Mellitus. J Pharm Sci . 2012;101:1647–58. doi: 10.1002/jps.23057. [DOI] [PubMed] [Google Scholar]
- Akash MSH, Rehman K, Li N, Gao JQ, Sun H, Chen S. Sustained delivery of IL-1Ra from pluronic F127-based thermosensitive gel prolongs its therapeutic potentials. Pharm Res . 2012;29:3475–85. doi: 10.1007/s11095-012-0843-0. [DOI] [PubMed] [Google Scholar]
- Akash MSH, Rehman K, Chen S. Role of Inflammatory Mechanisms in pathogenesis of Type 2 Diabetes Mellitus. J Cell Biochem . 2013;114:525–31. doi: 10.1002/jcb.24402. [DOI] [PubMed] [Google Scholar]
- Akash MSH, Rehman K, Sun H, Chen S. IL-1Ra improves normoglycemia and insulin sensitivity in diabetic GK-Rats. Eur J Pharmacol . 2013;701:87–95. doi: 10.1016/j.ejphar.2013.01.008. [DOI] [PubMed] [Google Scholar]
- Akash MSH, Rehman K, Chen S. sustained delivery of IL-1Ra from PF127 gel reduces hyperglycemia in diabetic GK rats. PLoS One . 2013;8:e55925. doi: 10.1371/journal.pone.0055925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Akash MSH, Rehman K, Gillani Z, Sun H, Chen S. Cross-species comparison of IL-1Ra sequence between human and rat. J Proteomics Bioinform . 2013;6:38–42. [Google Scholar]
- Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC. et al. Infectious Diseases Society of America; American Thoracic Society. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis . 2007;44:S27–S72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hazir T, Qazi SA, Nisar YB, Maqbool S, Asghar R, Iqbal I. et al. Comparison of standard versus double dose of amoxicillin in the treatment of non-severe pneumonia in children aged 2-59 months: A multi-centre, double blind, randomized controlled trial in Pakistan. Arch Dis Child . 2007;92:291–7. doi: 10.1136/adc.2005.092494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zuberi FF, Khan JA. Prospective comparison of prediction rules of mortality risk for CAP in a developing country. Int J Tuberc Lung Dis . 2008;12:447–52. [PubMed] [Google Scholar]
- Irfan M, Hussain SF, Mapara K, Mogri M, Bana M, Malik A. et al. Community acquired pneumonia: risk factors associated with mortality in a tertiary care hospitalized patients. J Pak Med Assoc . 2009;59:448–52. [PubMed] [Google Scholar]
- Mastro TD, Ghafoor A, Nomani NK, Ishaq Z, Anwar F, Granoff DM. et al. Antimicrobial resistance of pneumococci in children with acute lower respiratory tract infection in Pakistan. Lancet . 1991;337:156–9. doi: 10.1016/0140-6736(91)90813-5. [DOI] [PubMed] [Google Scholar]
- Mastro TD, Nomani NK, Ishaq Z, Ghafoor A, Shaukat NF, Esko E. Use of nasopharyngeal isolates of Streptococcus pneumoniae and Haemophilus influenzae from children in Pakistan for surveillance for antimicrobial resistance. Pediatr Infect Dis J . 1993;12:824–30. doi: 10.1097/00006454-199310000-00006. [DOI] [PubMed] [Google Scholar]
- Tanwani AK, Khan MA, Qazi SA. Antimicrobial drug resistance patterns in acute respiratory infections in children of Pakistan. In: Ohba Y, Kanno T, Okabe H, et al, eds. Quality control in the clinical laboratory ’95. Proceedings of the 8xxsupthxysup International Symposium on Quality Control; Kobe, Japan. Tokyo: Excerpta Medica 1995;108-115. [Google Scholar]
- Bochud PY, Moser F, Erard P, Verdon F, Studer JP, Villard G. Bochud PY, Moser F, Erard P, Verdon F, Studer JP, Villard GCommunity-acquired pneumoniaA prospective outpatient study. Medicine . 2001;80:75–87. doi: 10.1097/00005792-200103000-00001. [DOI] [PubMed] [Google Scholar]
- Wattanathum A, Chaoprasong C, Nunthapisud P, Chantaratchada S, Limpairojn N, Jatakanon A. et al. Community-acquired pneumonia in Southeast Asia: the microbial differences between ambulatory and hospitalized patients. Chest . 2003;123:1512–9. doi: 10.1378/chest.123.5.1512. [DOI] [PubMed] [Google Scholar]
- Arnold FW, Summersgill JT, Lajoie AS, Peyrani P, Marrie TJ, Rossi P. et al. A worldwide perspective of atypical pathogens in community-acquired pneumonia. Am J Respir Crit Care Med . 2007;175:1086–93. doi: 10.1164/rccm.200603-350OC. [DOI] [PubMed] [Google Scholar]
- Blasi F, Iori I, Bulfoni A, Corrao S, Costantino S, Legnani D. Can CAP guideline adherence improve patient outcome in internal medicine departments? . Eur Respir J . 2008;32:902–10. doi: 10.1183/09031936.00092607. [DOI] [PubMed] [Google Scholar]


