Abstract
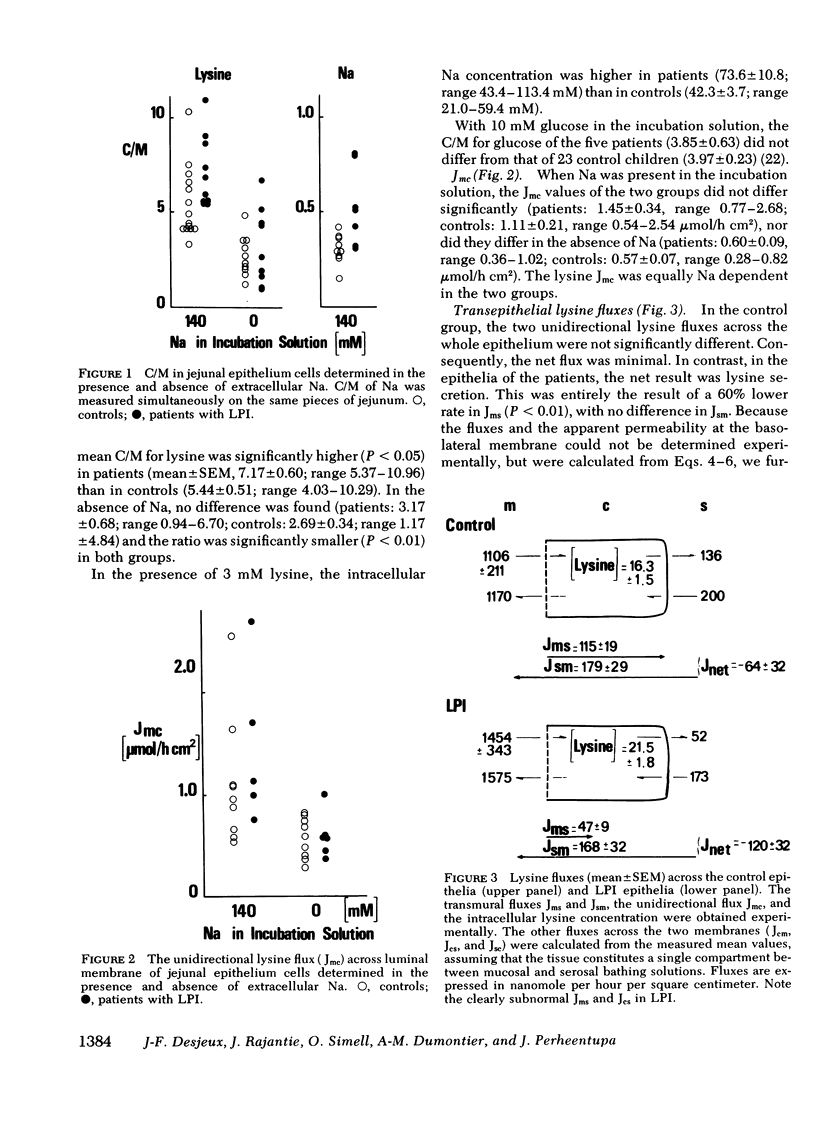
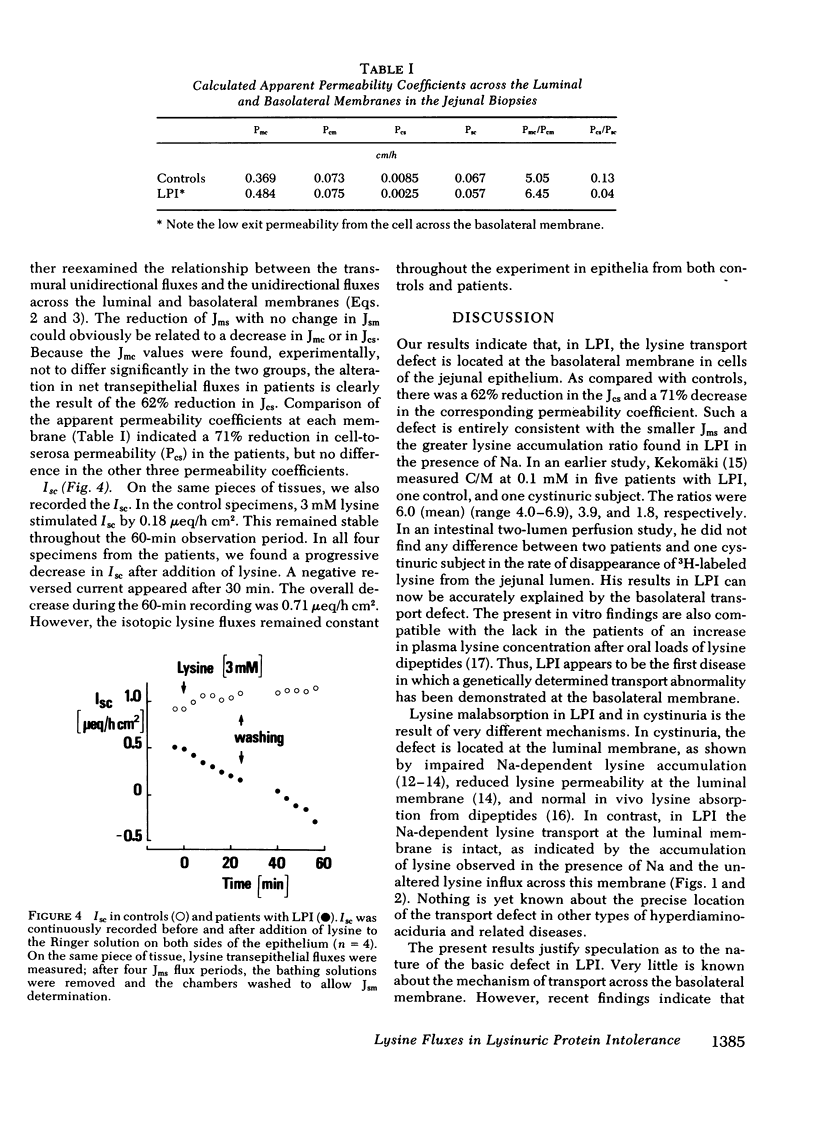
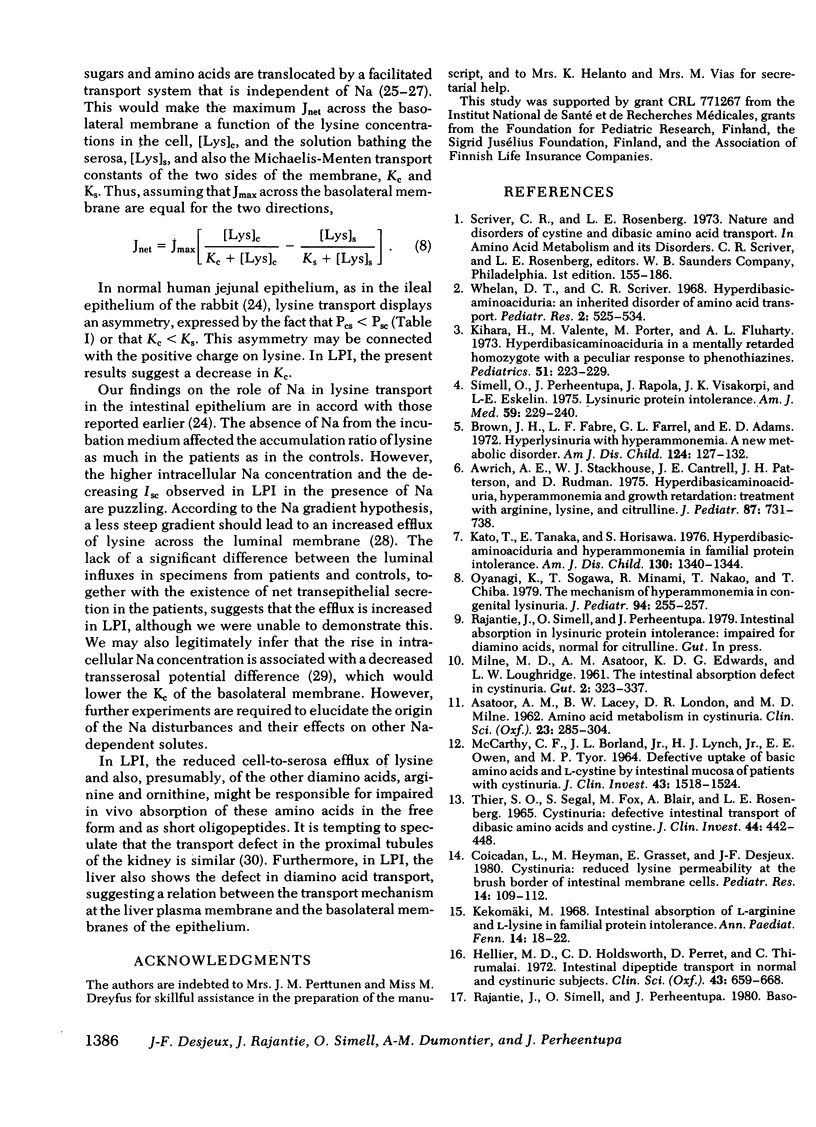
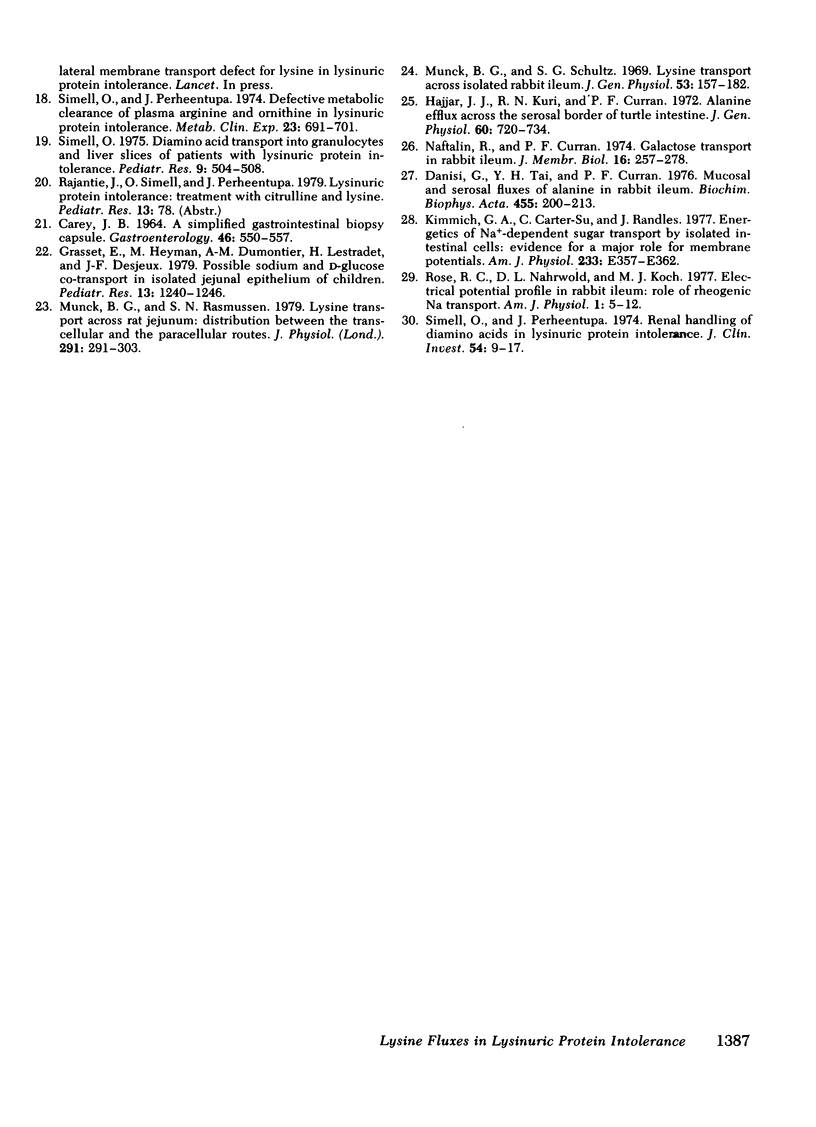
Lysinuric protein intolerance (LPI) is one of a group of genetic diseases in which intestinal absorption of the diamino acids lysine, arginine, and ornithine is impaired. In LPI, the clinical symptoms are more severe than in the kindred disorders. The mechanism of lysine absorption was, therefore, investigated in vitro on peroral jejunal biopsy specimens in seven patients with LPI and 27 controls. The lysine concentration ratio between cell compartment and medium was significantly higher in the LPI group (mean±SEM, 7.17±0.60) than in the controls (5.44±0.51). This was also true for the intracellular Na concentration (LPI, 73.6±10.8 mM; controls 42.3±3.7 mM). The rate of unidirectional influx of lysine across the luminal membrane was Na dependent and was the same in the two groups. In the absence of an electrochemical gradient, net transepithelial lysine secretion was observed in LPI. This was entirely the result of a 60% reduction of the unidirectional flux from mucosa to serosa. Calculation of unidirectional fluxes revealed the most striking difference at the basolateral membrane, where the flux from cells to serosa was reduced by 62% and the corresponding permeability coefficient reduced by 71%. A progressive reduction in short-circuit current appeared in the epithelia of all four patients with LPI tested after addition of 3 mM lysine. Thus, LPI appears to be the first disease in which a genetically determined transport defect has been demonstrated at the basolateral membrane.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- ASATOOR A. M., LACEY B. W., LONDON D. R., MILNE M. D. Aminoacid metabolism in cystinuria. Clin Sci. 1962 Oct;23:285–304. [PubMed] [Google Scholar]
- Awrich A. E., Stackhouse W. J., Cantrell J. E., Patterson J. H., Rudman D. Hyperdibasicaminoaciduria, hyperammonemia, and growth retardation: Treatment with arginine, lysine, and citrulline. J Pediatr. 1975 Nov;87(5):731–738. doi: 10.1016/s0022-3476(75)80296-4. [DOI] [PubMed] [Google Scholar]
- Brown J. H., Fabre L. F., Jr, Farrell G. L., Adams E. D. Hyperlysinuria with hyperammonemia. A new metabolic disorder. Am J Dis Child. 1972 Jul;124(1):127–132. doi: 10.1001/archpedi.1972.02110130129021. [DOI] [PubMed] [Google Scholar]
- CAREY J. B., Jr A SIMPLIFIED GASTROINTESTINAL BIOPSY CAPSULE. Gastroenterology. 1964 May;46:550–557. [PubMed] [Google Scholar]
- Coicadan L., Heyman M., Grasset E., Desjeux J. F. Cystinuria: reduced lysine permeability at the brush border of intestinal membrane cells. Pediatr Res. 1980 Feb;14(2):109–112. doi: 10.1203/00006450-198002000-00008. [DOI] [PubMed] [Google Scholar]
- Danisi G., Tai Y. H., Curran P. F. Mucosal and serosal fluxes of alanine in rabbit ileum. Biochim Biophys Acta. 1976 Nov 11;455(1):200–213. doi: 10.1016/0005-2736(76)90164-4. [DOI] [PubMed] [Google Scholar]
- Grasset E., Heyman M., Dumontier A. M., Lestradet H., Desjeux J. F. Possible sodium and D-glucose cotransport in isolated jejunal epithelium of children. Pediatr Res. 1979 Nov;13(11):1240–1246. doi: 10.1203/00006450-197911000-00008. [DOI] [PubMed] [Google Scholar]
- Hajjar J. J., Khuri R. N., Curran P. F. Alanine efflux across the serosal border of turtle intestine. J Gen Physiol. 1972 Dec;60(6):720–734. doi: 10.1085/jgp.60.6.720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hellier M. D., Holdsworth C. D., Perrett D., Thirumalai C. Intestinal depeptide transport in normal and cystinuric subjects. Clin Sci. 1972 Nov;43(5):659–668. doi: 10.1042/cs0430659. [DOI] [PubMed] [Google Scholar]
- Kato T., Tanaka E., Horisawa S. Hyperdibasicaminoaciduria and hyperammonemia in familial protein intolerance. Am J Dis Child. 1976 Dec;130(12):1340–1344. doi: 10.1001/archpedi.1976.02120130046010. [DOI] [PubMed] [Google Scholar]
- Kekomäki M. Intestinal absorption of L-arginine and L-lysine in familial protein intolerance. Ann Paediatr Fenn. 1968;14(1):18–22. [PubMed] [Google Scholar]
- Kihara H., Valente M., Porter M. T., Fluharty A. L. Hyperdibasicaminoaciduria in a mentally retarded homozygote with a peculiar response to phenothiazines. Pediatrics. 1973 Feb;51(2):223–229. [PubMed] [Google Scholar]
- Kimmich G. A., Carter-Su C., Randles J. Energetics of Na+-dependent sugar transport by isolated intestinal cells: evidence for a major role for membrane potentials. Am J Physiol. 1977 Nov;233(5):E357–E362. doi: 10.1152/ajpendo.1977.233.5.E357. [DOI] [PubMed] [Google Scholar]
- MCCARTHY C. F., BORLAND J. L., Jr, LYNCH H. J., Jr, OWEN E. E., TYOR M. P. DEFECTIVE UPTAKE OF BASIC AMINO ACIDS AND L-CYSTINE BY INTESTINAL MUCOSA OF PATIENTS WITH CYSTINURIA. J Clin Invest. 1964 Aug;43:1518–1524. doi: 10.1172/JCI105028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milne M. D., Asatoor A. M., Edwards K. D., Loughridge L. W. The intestinal absorption defect in cystinuria. Gut. 1961 Dec;2(4):323–337. doi: 10.1136/gut.2.4.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munck B. G., Rasmussen S. N. Lysine transport across rat jejunum: distribution between the transcellular and the paracellular routes. J Physiol. 1979 Jun;291:291–303. doi: 10.1113/jphysiol.1979.sp012813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munck B. G., Schultz S. G. Lysine transport across isolated rabbit ileum. J Gen Physiol. 1969 Feb;53(2):157–182. doi: 10.1085/jgp.53.2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naftalin R., Curran P. F. Galactose transport in rabbit ileum. J Membr Biol. 1974;16(3):257–278. doi: 10.1007/BF01872418. [DOI] [PubMed] [Google Scholar]
- Oyanagi K., Sogawa H., Minami R., Nakao T., Chiba T. The mechanism of hyperammonemia in congenital lysinuria. J Pediatr. 1979 Feb;94(2):255–257. doi: 10.1016/s0022-3476(79)80838-0. [DOI] [PubMed] [Google Scholar]
- Rose R. C., Nahrwold D. L., Koch M. J. Electrical potential profile in rabbit ileum: role of rheogenic Na transport. Am J Physiol. 1977 Jan;232(1):E5–12. doi: 10.1152/ajpendo.1977.232.1.E5. [DOI] [PubMed] [Google Scholar]
- Simell O. Diamino acid transport into granulocytes and liver slices of patients with lysinuric protein intolerance. Pediatr Res. 1975 May;9(5):504–508. doi: 10.1203/00006450-197505000-00008. [DOI] [PubMed] [Google Scholar]
- Simell O., Perheentupa J. Defective metabolic clearance of plasma arginine and ornithine in lysinuric protein intolerance. Metabolism. 1974 Aug;23(8):691–701. doi: 10.1016/0026-0495(74)90001-8. [DOI] [PubMed] [Google Scholar]
- Simell O., Perheentupa J., Rapola J., Visakorpi J. K., Eskelin L. E. Lysinuric protein intolerance. Am J Med. 1975 Aug;59(2):229–240. doi: 10.1016/0002-9343(75)90358-7. [DOI] [PubMed] [Google Scholar]
- Simell O., Perheentupa J. Renal handling of diamino acids in lysinuric protein intolerance. J Clin Invest. 1974 Jul;54(1):9–17. doi: 10.1172/JCI107753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- THIER S. O., SEGAL S., FOX M., BLAIR A., ROSENBERG L. E. CYSTINURIA: DEFECTIVE INTESTINAL TRANSPORT OF DIBASIC AMINO ACIDS AND CYSTINE. J Clin Invest. 1965 Mar;44:442–448. doi: 10.1172/JCI105157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whelan D. T., Scriver C. R. Hyperdibasicaminoaciduria: an inherited disorder of amino acid transport. Pediatr Res. 1968 Nov;2(6):525–534. doi: 10.1203/00006450-196811000-00011. [DOI] [PubMed] [Google Scholar]


