ABSTRACT
Although the benefits of integrating behavioral health (BH) services into primary care are well established (World Health Organization and World Organization of Family Doctors, 2012; Chiles et al. in Clin Psychol–Sci Pr 6:204–220, 1999; Cummings 1997; O’Donohue et al. 2003; Olfson et al. in Health Aff 18:79–93, 1999; Katon et al. in Ann Intern Med 124:917–925, 2001; Simon et al. in Arch Gen Psychiatry 52:850–856, 1995; Anderson et al. in Diabetes Care 24:1069–1078, 2001; Ciechanowski et al. in Arch Intern Med 160:3278–3285, 2000; Egede et al. in Diabetes Care 25:464–470, 2002), research has focused primarily on describing the types of interventions behavioral health providers (BHPs) employ rather than on reasons for referral, treatment initiation rates, or the patient characteristics that may impact them. This study presents the results of a multisite card study organized by The Collaborative Care Research Network, a subnetwork of the American Academy of Family Physicians’ National Research Network devoted to conducting practice-based research focused on the provision of BH and health behavior services within primary care practices. The goals of the study included: (1) identifying the characteristics of patients referred for BH services; (2) codifying reasons for referral and whether patients were treated for the referral; (3) exploring any differences between patients who initiated BH contact and those who did not; and (4) assessing the types and frequency of BH services provided to patients who attended at least one appointment. Of the 200 patients referred to a BHP, 81 % had an initial contact, 71 % of which occurred on the same day. Men and women were equally likely to engage with a BHP although the time between appointments varied by gender. Depression and anxiety were the primary reasons for referral. Practice-based research is a viable strategy for advancing the knowledge about integrated primary care.
KEYWORDS: Integrated primary care, Collaborative care, Co-location behavioral health, Mental health, Treatment initiation rates
BACKGROUND
Mental health problems are common in patients seen in primary care practices [11]. It is estimated that as many as 25 % of primary care patients will have a diagnosable DSM mental health problem in a year [1]. When including sub-threshold conditions, conditions related to behaviors and poor life choices, and psychosocial stressors negatively impacting functioning, most primary visits have a significant psychosocial component [12]. The vast majority of common problems seen in primary care practices are related to behaviors, including tobacco abuse, obesity, diabetes, and hypertension, and it has been estimated that 40 % of premature deaths in the USA are attributable to health behavior factors [13, 14].
In an effort to improve the health care system, the movement towards integration of behavioral health into primary care settings has gained support [1, 15–20], and national and international organizations are recommending integration as an approach to improving health care [1, 18, 20]. Despite these advantages, many primary care practices still do not provide integrated services. A recent survey of all NCQA certified Patient-Centered Medical Homes found that less than 40 % of responding practices had any mental health, substance abuse, and health behavior services within the practice (Kessler, in review).
Primary care is an ideal environment in which to focus integration efforts because it is here that most patients with mental health, substance abuse, and health behavior needs are already being seen and often treated [21–29]. Integrated primary care practices hold the promise of better care through the potential for increased access to and utilization of services as well as improved identification and treatment of mental health issues. In addition to referring patients with mental health and substance abuse conditions, primary care providers (PCPs) can refer for treatment of the psychosocial and/or behavioral aspects of acute and chronic medical conditions that can complicate treatment and impact adherence to medical recommendations [26, 30].
Despite the prevalence of behavioral health need identified in primary care, however, the need has not always translated into actual care due to difficulties in accessing treatment resources and low treatment initiation rates among patients referred to specialty mental health [31]. On-site availability of services generates referrals, enhances communication, and facilitates collaborative treatment [32]. Patients will often initiate treatment whereas they may not if asked to go off-site. In an internal quality improvement survey of patients who attended Patient-Centered Behavioral Health (PCBH) services at Aesculapius Medical Center in Vermont, 62 % of patients responded that they initiated care because it was located at the primary care site [33]. Having a behavioral health provider on site allows for a single repository for a broad range of mental health, substance abuse, and medical problems, additionally allowing for relationships conducive to the sharing of medical and behavioral issues between PCPs and behavioral health providers (BHPs).
Despite the compelling arguments for addressing patients’ behavioral health needs, PCPs have identified quality behavioral health care as the singularly most difficult subspecialty medical service to access [34]. The literature that does exist suggests initiation rates to specialty mental health are less than 50 % [35, 36]. Initial data from two Vermont primary care sites working within the PCBH model have generated referral to treatment initiation rates of 95.5 and 69 % [37]. A limitation of that report is that at one site, patients scheduled and patient initiation were reported, while at the second site, patients referred and scheduled and patients scheduled and who began treatment were reported, creating limitations on data comparison. Building on this work, we proposed to assess treatment initiation rates in a range of integrated practices from around the country.
METHODS
Aims
The objectives of this study include:
Identifying the characteristics of patients referred for behavioral health (BH) services
Codifying reasons for referral and whether patients were treated for the referral
Exploring any differences between patients who initiated BH contact and those who did not
Assessing the types and frequency of BH services provided to patients who attended at least one appointment
Study population
Site coordinators in six primary care practices, all of the members of with the National Research Network’s Collaborative Care Research Network, were recruited. Sites were selected for geographic diversity, interest, and ability to participate. To be selected, practices needed to have behavioral health clinicians as part of the practice. Practices were located in Colorado, Massachusetts, Minnesota, and Vermont and included both rural and urban settings. Five of the sites completed the study, and one site withdrew from participation. Table 1 reviews the practice characteristics.
Table 1.
Practice characteristics
| Practice description | Location | Type | Number of sites |
|---|---|---|---|
| Federally qualified health center | Colorado | Rural and Urban | 4 |
| Internal medicine clinic | Vermont | Suburban | 1 |
| Academic health center and family medicine training clinic | Massachusetts | Rural | 1 |
| Academic health center and family medicine training clinic | Massachusetts | Urban | 1 |
| Family residency site; family practice clinic | Minnesota | Urban | 1 |
Across the five practices, 127 providers (71 females; 51 males; and 5 unknown) were consented into the study. PCPs included family physicians, family medicine residents, internists, nurse practitioners, and physician assistants. BHPs practicing in these health centers included psychologists and social workers. Among the PCPs, 83 (90.2 %) were family physicians and 9 (9.8 %) were internal medicine providers. Among the BHPs, five identified as Ph.D./Psy.Ds. and five MSWs. The remainder of the providers did not specify a discipline. The mean age of providers was 38.86 years (range, 27–60) and the average number of years of practice across all types of providers was 9.96 years (range, 1–38).
Data collection
Data were collected at each site for a total of 6 weeks. Patients who were identified for referral to a BHP by a PCP during the first 2 weeks of the study were included. The remaining 4 weeks of the study period were used to allow these patients to establish contact with a BHP.
Measures
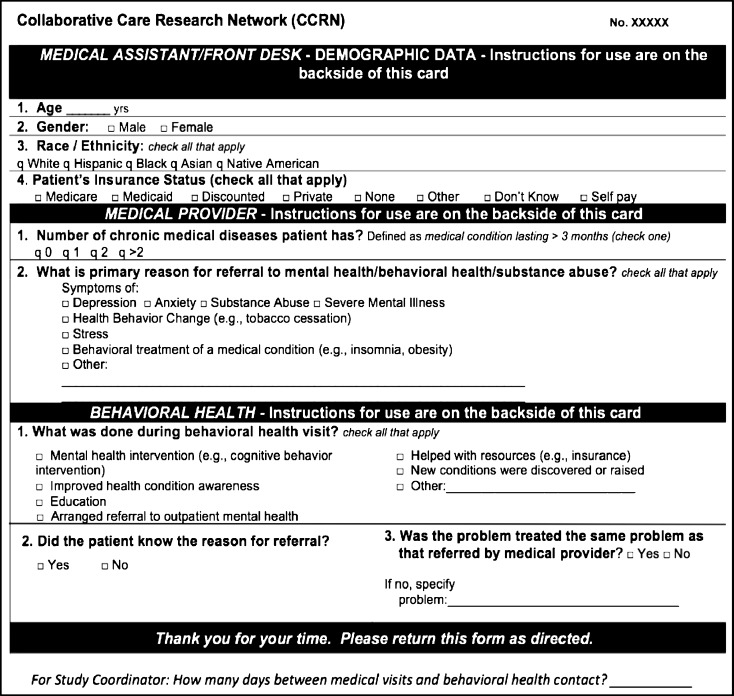
PCPs and BHPs completed brief forms recording their demographic information including age, gender, specialty, degrees, and credentials. The form is enclosed in Appendix 1. Each card assessed the patient’s age, gender, race/ethnicity, insurance status, number of chronic diseases, and primary reason for referral to behavioral health. For patients who established contact with a BHP, the focus of the first behavioral health encounter, the patient’s knowledge regarding the reason for referral, and the concordance between the reason for referral and focus of the session were assessed. Also, the number of days between the referral and the first contact with the BHP was calculated. The card is presented in Fig. 1.
Fig 1.
Study card
Procedures
Initially, all sites were asked to have the PCPs complete the top of the cards which included questions about patient demographics and reason for referrals. The BHPs were to complete the bottom portion of the cards for those patients that had contact with the BHPs. Because of site differences, procedures for completing the cards were somewhat varied. Prior to beginning data collection, three sites requested, and were subsequently granted permission after IRB amendment, to have BHPs complete the entire card for all patients identified for referral. This allowed these sites to proceed with data collection using existing operational workflows rather than retooling their practice for the purposes of this study.
Data analysis
Using SPSS version 19, descriptive statistics, univariate and nonparametric analyses were used as indicated to address each of the stated goals.
RESULTS
Across all providers, 200 patients were referred for behavioral health consultation, the majority (69 %, n = 138) being females. Although well over half of the sample were White (60 %; n = 120), 32 % (n = 64) were Hispanic due to a large Hispanic population at one of the five clinics. Insurance status was widely distributed with the largest proportion of patients (n = 71) having some form of discounted insurance, followed by Medicaid. Most patients (65 %) referred to a BHP had one or more chronic diseases. The patient sample demographic characteristics are presented in Table 2.
Table 2.
Sample demographics
| Total samplea | |
|---|---|
| N | 200 |
| Age | 35.44 (SD = 15.50) |
| Race | |
| White | 60.0 % (n = 120) |
| Hispanic | 32.0 % (n = 64) |
| Insurance | |
| Medicare | 9.0 % (n = 18) |
| Medicaid | 33.0 % (n = 66) |
| Discounted | 35.5 % (n = 71) |
| Private | 16.0 % (n = 32) |
| Number of chronic illnesses | |
| 0 | 34.5 % (n = 69) |
| 1 | 22.5 % (n = 45) |
| 2 | 14.0 % (n = 28) |
| 3 or more | 24.0 % (n = 48) |
| Treatment initiation | 81 % (n = 162) |
aTotal sample reflects all cases included in one or more analyses. Due to missing data, the actual n is also reported for every variable in subsequent analyses
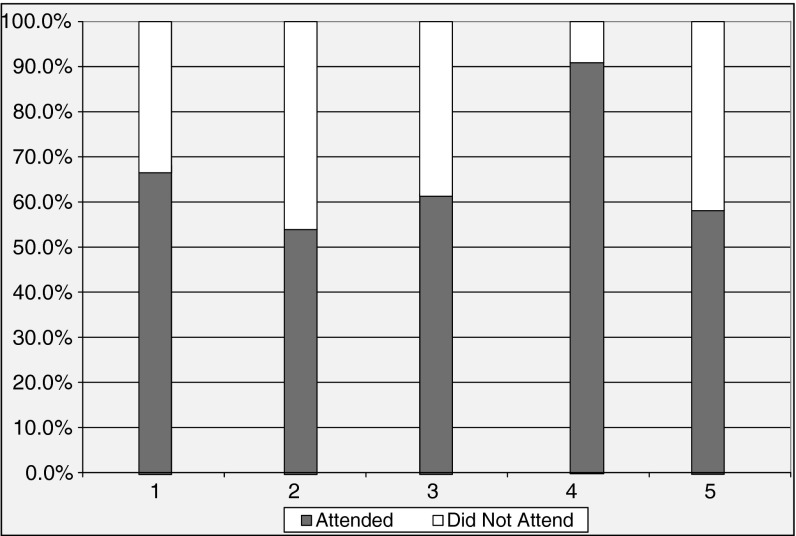
Among all referred patients, 162 initiated treatment for an 81 % average rate of behavioral health engagement. Treatment initiation varied across sites as shown in Fig. 2, from as low as 54.5 % at one site to a maximum of 90.6 % at another site.
Fig 2.
Behavioral health engagement by site
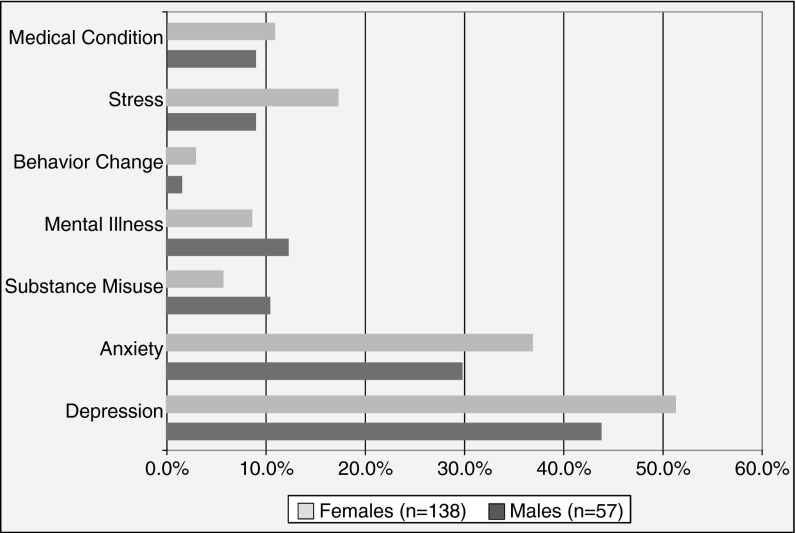
Eighty-seven percent of referred patients (n = 142) reported that they were aware of the reason for the BH referral, and in 80.0 % of cases (n = 130), the BH visit was focused on the stated reason for referral. In every site except for the one with the majority of the patients, patients were aware of the reason for the referral and the BH visit was focused on the stated reason for referral. The stated reasons for BH referral, by gender, are presented in Fig. 3.
Fig 3.
PCP reasons for behavioral health referral. Categories are not mutually exclusive as instructions were to check all that apply
Some 80.4 % of females (n = 111) and 80.7 % of males (n = 46) attended a BH visit after referral. The number of days between the medical visit which prompted the referral to behavioral health and when the patient was seen for the consultation was 3.82 days (range = 0–35 days; SD = 8.21). Notably, the number of days between the medical and behavioral health visit among females (4.51 days, SD = 8.70) was significantly longer than among males (2.67 days; SD = 7.30; F = 4.71, p = 0.03). Of note, most BH visits occurred on the same day as the medical visit (n = 109, 71.2 %). The majority (64.9 %) of males were seen for their BH visit on the same day as their medical visit, with a range from 0 to 35 days, whereas only 53.6 % of females were seen on the same day of their medical visit, with a range from 0 to 30 days.
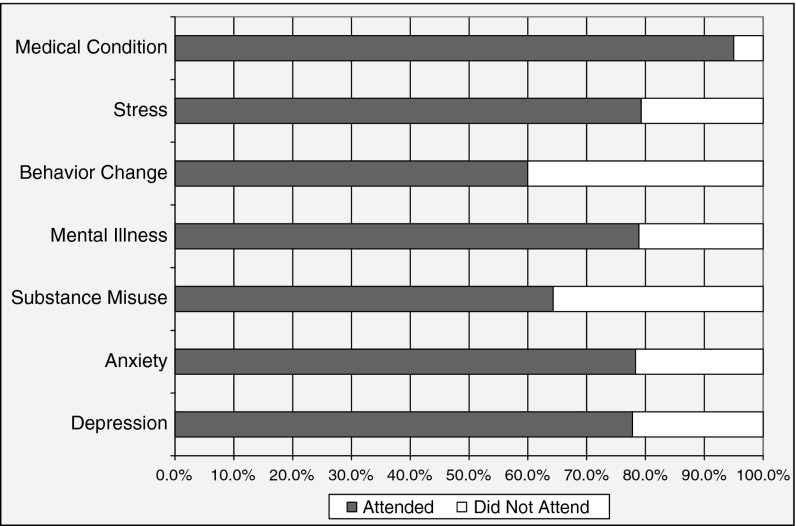
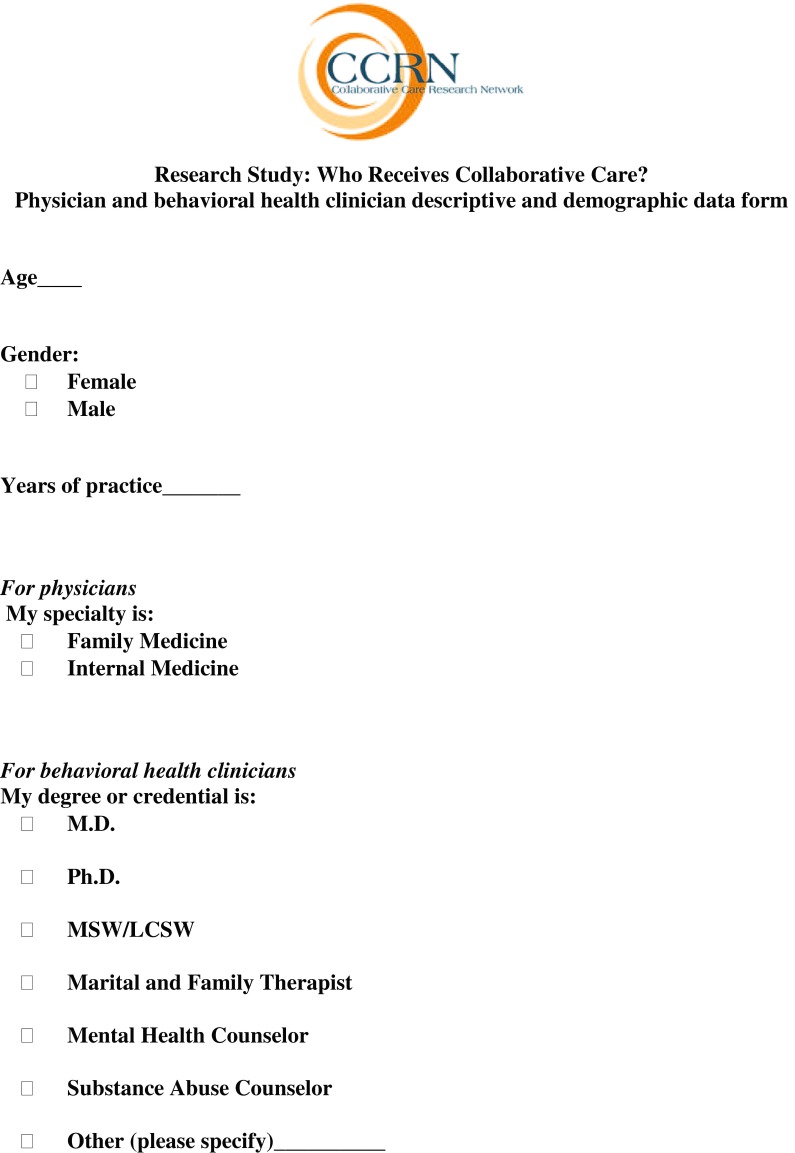
Initiation rates were then considered within each reason for referral. As Fig. 4 shows, individuals who were referred for a medical condition were most likely to initiate treatment, and those referred for behavior change were the least likely. The characteristics of treatment initiators were further analyzed to descriptively explore potential demographic or other associated variables. Although the small sample size did not allow for meaningful comparisons between the attenders and non-attenders, the frequency distribution provides the basis from which inquiry can occur in future studies. There was no notable difference in gender or age between those who attended a BH visit and those who were referred to BH but never had an initial visit during the period of data collection. Finally, the types and frequency of BH services provided to patients who attended one or more appointments (not mutually exclusive categories) are shown in Fig. 5.
Fig 4.
Reasons for referral and attendance at behavioral health visit
Fig 5.
Types and frequency of behavioral health services
DISCUSSION
In addition to clinical face validity and burgeoning empirical support for treating specific conditions using models of integrated service delivery, it is important to further examine and understand the processes of how this care is provided. The most notable finding in this study was the large proportion of referred patients who attended an initial BH visit. The findings underscore the importance of same day access to BH services as 71 % of the sample was seen by a BHP on the same day as their medical appointment which generated the referral. Among those who attended an initial BH visit, the time delay between the medical and BH visit was less for men than for women. Moreover, not only were 87 % of patients clear about why their PCP referred them for BH services, PCPs were accurate about the need for the referral as 80 % of the time the BHP and patient actually addressed the referral issue in the BH visit. This finding may be an anomaly given the maturity of the integrated primary care (IPC) practices involved in this study, as many of the practices employed routine screening instruments to proactively identify BH needs such as depression or anxiety. Newly developed IPC practices might find it necessary to train PCPs on how to present BH services to patients in a manner that is not demoralizing or confusing to patients but rather increases the likelihood of patient engagement.
In this study, most of the patients referred for behavioral health consultations during the period of data collection were Caucasian females. Despite a relatively young age for the sample (M = 35 years), 65 % were coping with one or more chronic diseases. Psychosocial complexity is common among all patients managing a chronic illness and effective treatment plans must include attention to this complexity. Given that most care for a chronic illness occurs outside of the PCP’s office (i.e., it is done by the patient and/or family members through daily attention to self-care, exercise, diet, pain management, etc.), consultations with BHPs to assess self-management goals and barriers, which may include mental health conditions, are indicated as part of high-quality and routine primary care.
Consistent with the literature, it is not surprising that depression and anxiety were reported as the most common reasons for BHP involvement. Indeed, these represent the most prevalent mental health conditions, the symptoms which are typically concomitant with chronic medical conditions, as well as syndromes with physical symptoms for which care by a PCP could be sought (e.g., insomnia, gastrointestinal distress, lethargy, poor appetite, and weight gain). Patients referred for depression and anxiety, as well as those referred for stress and medical conditions, were highly likely to attend the initial BH visit. In contrast, comparatively lower rates of attendance were noted when the reason for referral was related to substance use or behavior change. This result is not surprising and likely represents expected discordance between the PCPs’ commitment to treating substance abuse and lifestyle factors impacting chronic medical illness and patients’ commitment to engaging in substance abuse treatment or difficult behavioral changes.
Finally, BHPs employed the expected services during the initial visit, with assessment and consultation being the most common, followed by BH interventions. In more traditional mental health settings (outside of primary care clinics), delivering an intervention on the first BH visit is rare. The relatively high proportion of interventions reported during the initial visit (over one third of patients received an intervention) is a reflection of the sophisticated service delivery models employed among the study sites.
LIMITATIONS
While the treatment initiation rates in this study are provocative, we acknowledge the methodological limitations. The sample sizes were discrepant by site and not large enough to allow for between practice comparisons. Differences in treatment initiation rates may in part reflect the differences between practices’ patient populations and local variations in integrated primary care models. A more systematic investigation is warranted.
CONCLUSION
Given the contemporary primary care focus on chronic disease, on comorbidity between chronic medical and behavioral health disorders, and the apparent willingness of patients with chronic health issues to initiate behavioral health interventions, investigation of behavioral health interventions with multi-morbidities should be considered. This investigation was conducted during a time when multiple sites were making the transition to electronic health records (EHR). Further investigations utilizing larger networks of practices that are EHR enabled will facilitate this type of research.
This report is not sufficient for us to understand the precise reasons why patients do not initiate treatment. Future studies should clarify the relative impact of patient factors, types of conditions, and systemic factors such as team composition, service delivery model, and physical environment on treatment initiation in IPC practices.
There is a growing understanding that most primary care patients can benefit from a psychosocial assessment. With the movement toward panel-based and population-based care in which patient services are protocol driven rather than referral driven, the entire construct of referral for mental health and substance abuse services will need to be reevaluated. Further, the movement within primary care toward including behavioral risk assessment as part of the regular process of care will broaden and change the role of the primary care behavioral health provider. Enhanced knowledge about why and how PCPs involve BHPs, as well as patient characteristics which influence these processes will inform the development of successful integrated primary care practices. Ultimately, the promulgation of IPC practices has the potential to broaden access to care, improve health outcomes, and lower costs.
Appendix 1
Footnotes
Implications
Practice: In order to maximize the chances of higher rates of behavioral health treatment initiation than what is commonly achieved through referrals to specialty mental health care, primary care practices should integrate on-site behavioral health services.
Policy: Resources should be directed toward the further development of policies that facilitate the provision of behavioral health services to patients in primary care.
Research: Card study methodology can be effectively implemented across different kinds of integrated primary care practices to assess patient variables associated with behavioral health treatment initiation.
REFERENCES
- 1.World Health Organization and World Organization of Family Doctors. Integrating mental health into primary care: a global perspective. Geneva: World Health Organization. Available at http://www.who.int/mental_health/policy/Integratingmhintoprimarycare2008_lastversion.pdf. Accessed January 26, 2012
- 2.Chiles JA, Lambert MJ, Hatch AL. The impact of psychological interventions on medical cost offset: a meta-analytic review. Clin Psychol–Sci Pr. 1999;6:204–220. doi: 10.1093/clipsy.6.2.204. [DOI] [Google Scholar]
- 3.Cummings NA. Behavioral health in primary care: dollars and sense. In: Cummings NA, Johnston JN, Cummings J, editors. Behavioral Health in Primary Care: A Guide for Clinical Integration. Madison, CT: Psychosocial Press; 1997. pp. 3–21. [Google Scholar]
- 4.O’Donohue WT, Cummings NA, Ferguson KE. Clinical integration: the promise and the path. In: Cummings NA, O’Donohue WT, Ferguson KE, editors. Behavioral Health as Primary Care: Beyond Efficacy to Effectiveness. Reno, NV: Context; 2003. pp. 15–30. [Google Scholar]
- 5.Olfson M, Sing M, Slesinger HJ. Mental health/medical cost care offsets: opportunities for managed care. Health Aff. 1999;18:79–93. doi: 10.1377/hlthaff.18.2.79. [DOI] [PubMed] [Google Scholar]
- 6.Katon WJ, Sullivan M, Walker E. Medical symptoms without identified pathology: relationship to psychiatric disorders, childhood and adult trauma, and personality traits. Ann Intern Med. 2001;124:917–925. doi: 10.7326/0003-4819-134-9_part_2-200105011-00017. [DOI] [PubMed] [Google Scholar]
- 7.Simon GE, VonKorff M, Barlow W. Health care costs of primary care patients with recognized depression. Arch Gen Psychiatry. 1995;52:850–856. doi: 10.1001/archpsyc.1995.03950220060012. [DOI] [PubMed] [Google Scholar]
- 8.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24:1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 9.Ciechanowski PS, Katon WJ, Russo JE. Depression and diabetes: impact of depressive symptoms on adherence, function, and costs. Arch Intern Med. 2000;160:3278–3285. doi: 10.1001/archinte.160.21.3278. [DOI] [PubMed] [Google Scholar]
- 10.Egede LE, Zheng D, Simpson K. Comorbid depression is associated with increased health care use and expenditures in individuals with diabetes. Diabetes Care. 2002;25:464–470. doi: 10.2337/diacare.25.3.464. [DOI] [PubMed] [Google Scholar]
- 11.Cwikel J, Zibler N, Feinson M, Lerner Y. Prevalence and risk factors of threshold and sub-threshold psychiatric disorders in primary care. Soc Psych Psych Epid. 2008;43(3):184–191. doi: 10.1007/s00127-007-0286-9. [DOI] [PubMed] [Google Scholar]
- 12.VandenBos G, DeLeon P. The use of psychotherapy to improve physical health. Psychother Theor Res Pract Train. 1988;25(3):335–343. doi: 10.1037/h0085353. [DOI] [Google Scholar]
- 13.McGinnis JM, Foege WH. Actual causes of death in the United States. J Am Med Assoc. 1993;270(18):2207–2212. doi: 10.1001/jama.1993.03510180077038. [DOI] [PubMed] [Google Scholar]
- 14.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States. J Am Med Assoc. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 15.Blount A. Integrated primary care: organizing the evidence. Fam Syst Health. 2003;21:121–133. doi: 10.1037/1091-7527.21.2.121. [DOI] [Google Scholar]
- 16.Doherty WJ, McDaniel SH, Baird MA. Five levels of primary care/behavioral healthcare collaboration. Behav Healthc Tomorrow. 1996;5:25–27. [PubMed] [Google Scholar]
- 17.Institute of Medicine. Crossing the quality chasm: a new health system for the 21st Century. Washington, DC: National Academies Press. 2001. Available at http://www.nap.edu/catalog.php?record_id=10027. Accessed January 26, 2012. [PubMed]
- 18.Institute of Medicine. Improving the quality of health care for mental and substance-use conditions: quality chasm series. Washington, DC: National Academies Press. 2006. Available at http://www.nap.edu/catalog.php?record_id=11470#toc. Accessed January 26, 2012. [PubMed]
- 19.Pincus HA. The future of behavioral health and primary care: drowning in the mainstream or left on the bank? Psychosomatics. 2003;44:1–11. doi: 10.1176/appi.psy.44.1.1. [DOI] [PubMed] [Google Scholar]
- 20.U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration. Transforming mental health care in America: the federal action agenda: first steps. 2006. Available at http://www.samhsa.gov/Federalactionagenda/NFC_execsum.aspx. Accessed January 26, 2012.
- 21.Beardsley RS, Gardocki GJ, Larson DB, Hidalgo J. Prescribing of psychotropic medication by primary care physicians and psychiatrists. Arch Gen Psychiatry. 1988;45:1117–1119. doi: 10.1001/archpsyc.1988.01800360065009. [DOI] [PubMed] [Google Scholar]
- 22.deGruy FV. Mental health care in the primary care setting. In: Donaldson MS, Yordy KD, Lohr KN, Vanselow NA, editors. Primary Care: America’s Health in a New Era. Washington, DC: National Academies Press; 1996. pp. 285–311. [PubMed] [Google Scholar]
- 23.Fries JF, Koop CE, Beadle CE, Cooper PP, England MJ, Greaves RF, et al. Reducing health care costs by reducing the need and demand for medical services: the Health Project Consortium. N Engl J Med. 1993;329:321–325. doi: 10.1056/NEJM199307293290506. [DOI] [PubMed] [Google Scholar]
- 24.Goldman HH, Rye P, Sirovatka P. A report of the surgeon general. Washington, DC: Department of Health and Human Services; 2000. [Google Scholar]
- 25.Petterson SM, Phillips RL, Bazemore AW, Dodoo MS, Zhang X, Green LA. Why there must be room for mental health in the medical home. 2008. Available at www.aafp.org/afp. Accessed January 26, 2012. [PubMed]
- 26.Regier D, Narrow W, Rae D, Manderscheid R, Locke B, Goodwin F. The de facto US mental and addictive services system: epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Arch Gen Psychiatry. 1993;50:85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- 27.Robins LN, Regier DA, editors. Psychiatric Disorders in America: The Epidemiologic Catchment Area Study. New York, NY: The Free Press; 1991. [Google Scholar]
- 28.Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the United States: results from the national comorbidity survey replication. Arch Gen Psych. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- 29.Wang PS, Demler O, Olfson M, Pincus HA, Wells KB, Kessler RC. Changing profiles of service sectors used for mental health care in the United States. Am J Psychiatry. 2006;163:1187–1198. doi: 10.1176/appi.ajp.163.7.1187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wagner EH, Austin BT, Davis C, Hindmarsh M, Schaefer J, Bonomi A. Improving chronic illness care: translating evidence into action. Health Aff. 2001;20(6):64–78. doi: 10.1377/hlthaff.20.6.64. [DOI] [PubMed] [Google Scholar]
- 31.Pincus HA, Hough L, Houtsinger JK, Rollman BL, Frank RG. Emerging models of depression care; multi-level (6P) strategies. Int J Methods Psychiatr Res. 2003;12:54–63. doi: 10.1002/mpr.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kessler R, Stafford D. Primary care is the de facto mental health system. In: Kessler R, Stafford D, editors. Collaborative Medicine Case Studies: Evidence in Practice. New York, NY: Springer; 2008. pp. 9–21. [Google Scholar]
- 33.Internal Aesculapius Medical Center document 2009.
- 34.Cunningham PJ. Beyond parity: a primary care physicians’ perspectives on access to mental health care. Health Aff. 2009;28(3):w490–w501. doi: 10.1377/hlthaff.28.3.w490. [DOI] [PubMed] [Google Scholar]
- 35.Williams J, Palmes G, Kurt K, Pulley A, Meschan JF. Referral by pediatricians of children with behavioral health disorders. Clin Pediatr. 2005;44:343–349. doi: 10.1177/000992280504400410. [DOI] [PubMed] [Google Scholar]
- 36.Scholle SH, Haskett RF, Hanusa BH, Pincus HA, Kupfer DJ. Addressing depression in obstetrics/gynecology practice. Gen Hosp Psychiatry. 2003;25:83–90. doi: 10.1016/S0163-8343(03)00006-9. [DOI] [PubMed] [Google Scholar]
- 37.Kessler R. Mental health care treatment initiation when mental health services are incorporated into primary care practice. J Am Board Fam Med. 2012;25(2):255–259. doi: 10.3122/jabfm.2012.02.100125. [DOI] [PubMed] [Google Scholar]