Abstract
Objective
We investigated the user requirements of African-American youth (aged 14–24 years) to inform the design of a culturally appropriate, network-based informatics intervention for the prevention of HIV and other sexually transmitted infections (STI).
Materials and Methods
We conducted 10 focus groups with 75 African-American youth from a city with high HIV/STI prevalence. Data analyses involved coding using qualitative content analysis procedures and memo writing.
Results
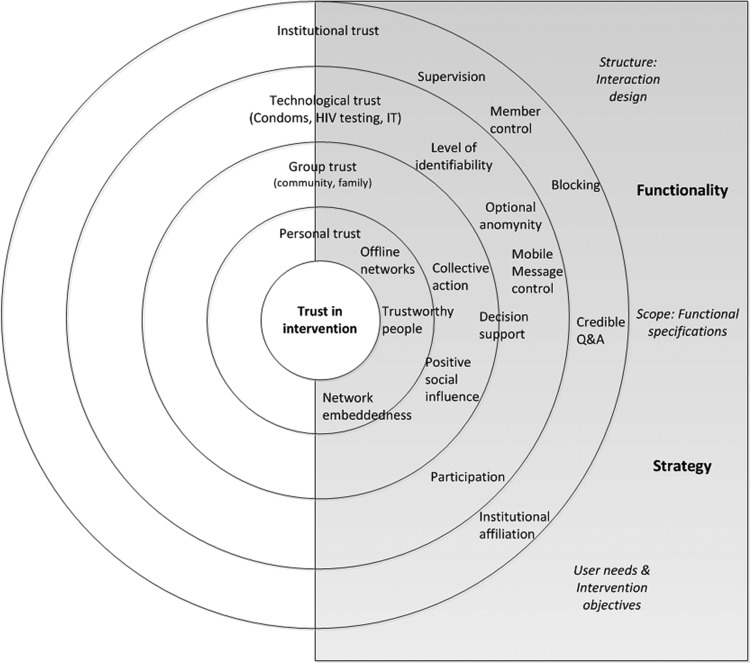
Unexpectedly, the majority of participants’ design recommendations concerned trust. Youth expressed distrust towards people and groups, which was amplified within the context of information technology-mediated interactions about HIV/STI. Participants expressed distrust in the reliability of condoms and the accuracy of HIV tests. They questioned the benevolence of many institutions, and some rejected authoritative HIV/STI information. Therefore, reputational information, including rumor, influenced HIV/STI-related decision making. Participants’ design requirements also focused on trust-related concerns. Accordingly, we developed a novel trust-centered design framework to guide intervention design.
Discussion
Current approaches to online trust for health informatics do not consider group-level trusting patterns. Yet, trust was the central intervention-relevant issue among African-American youth, suggesting an important focus for culturally informed design. Our design framework incorporates: intervention objectives (eg, network embeddedness, participation); functional specifications (eg, decision support, collective action, credible question and answer services); and interaction design (eg, member control, offline network linkages, optional anonymity).
Conclusions
Trust is a critical focus for HIV/STI informatics interventions for young African Americans. Our design framework offers practical, culturally relevant, and systematic guidance to designers to reach this underserved group better.
Keywords: Consumer health informatics, HIV/STI prevention, African Americans, youth, social networks, culturally informed design
Introduction
Sexually transmitted infections (STI), including HIV, are a significant public health concern for young people in the USA. Among 15–24-year-olds, 9.1 million new cases of STI, such as chlamydia, develop annually.1 In 2010, 8293 new cases of HIV emerged in this group.2 African-American youth have the highest rates of HIV and other STI of any racial group in the USA.2 3 Social network characteristics may explain these differential rates: with higher rates of HIV/STI in their social networks, African-American youth face greater odds of acquiring these infections during each sexual encounter.2 4 5 Network-mediated social influence also affects HIV/STI-related risk behavior.6 7 Therefore, interest is growing in social network-based HIV/STI prevention for youth,8 9 especially using social technologies.10 11 Although several offline network-based interventions have reduced HIV/STI-related risk behavior,12–14 previous HIV/STI informatics interventions have rarely adopted a network-based approach.15–18 Therefore, we sought to extend both HIV/STI prevention informatics and network intervention research by developing and evaluating a hybrid online/offline network intervention for African-American youth.
Design guidance is lacking for social network-based informatics applications promoting sexual health, particularly within underserved groups.19 Therefore, to inform intervention development, we conducted a series of design-oriented focus groups with African-American youth in a US city with high HIV/STI prevalence. Unexpectedly, most youth recommendations focused on trust, pointing to an important cultural issue for designing consumer health informatics (CHI) applications, or ‘… any electronic tool, technology or system that is primarily designed to interact with health information users or consumers’.20 Consequently, we present a novel trust-centered design framework for online HIV/STI prevention with African-American youth. We discuss the implications of these findings, then outline specific design choices salient to our framework. We conclude that trust should be a central design focus in CHI interventions for African-American youth.
Background and significance
Whether online or offline, network-based HIV/STI prevention must make trust a central concern.21 Trust is ‘…a state of favorable expectation regarding other people's actions and intentions’.22 Or we may distrust, holding ‘negative expectations’.23 Trust in one's sexual partners is a predictor of condom use and HIV/STI risk.24–28 Risk reduction requires both trust in prevention technologies, such as condoms and HIV/STI tests, and trust in HIV/STI interventions themselves.21 Similarly, trust is a critical antecedent to the success of CHI interventions,29 30 affecting how they are used: whether recommendations are followed,29 31 whether users contribute content or participate in discussions,32 33 and whether personal information is disclosed.34 Although at a nascent stage,35 health informatics research is thus increasingly focused on online trust promotion.
Specific design decisions can influence trust in CHI applications. Professional visual design may engender trust.36 Quality markers, such as references, may increase user trust in information.36 Trust may be enhanced with user participation in content production.37 Trust may be promoted by responsiveness to user needs, as with system personalization.36 38 References from users may also be used to promote the trust required for health-related transactions.39 For example, reputation systems, like RateMDs.com, provide decision support for choosing healthcare providers, and recommender systems like the one embedded in PatientsLikeMe.com aid in treatment option assessment.
Although these design approaches may promote user trust in general, they do not account for group-level trusting patterns.40 Trusting patterns vary among social groups in the USA,41 reflecting group culture, or the ‘system of meaning that underlies routine and behavior in everyday…life’.42 In the USA, race is a significant determinant of differences in trust levels.41 African Americans’ greater distrust of healthcare institutions is linked to a history of unethical medical experimentation and unequal treatment in healthcare settings.43 This distrust is linked to an inequity in health service usage,44 45 potentially including CHI applications.46 When compared to whites, African Americans are less likely to use personal health records,47 48 and patient portals,49 50 or to look for health information online.51 These racial differences are not entirely explained by internet access differentials.48 50 51 African Americans also express more concerns about online privacy than other racial groups.52
Given these differences, formative research must inform CHI intervention development to ensure effectiveness for African Americans.20 53 Similarly, trust is a critical factor in the emerging practice of culturally informed design of CHI interventions for this group.19 53 54 Therefore, an urgent need exists to investigate collective trust perceptions in order to inform the design of network-based informatics interventions, particularly those aspiring to engage African Americans. Sociological trust theory offers a useful bridge between the broad lens of culturally informed design and our specific trust focus.
Theoretical framework: sociology of trust
Sociological trust theory highlights the collective basis of trust. Trust is a multilevel phenomenon, with (dis)trust carrying over between targets at different levels of social aggregation, including people, groups, technologies, and institutions.55 Cultural factors, including norms, values, and symbols, tell us who or what to trust, and when to trust (the ‘primary targets of trust’).55 The expectations underlying (dis)trust are systemically rooted in culture. Two key expectation types include: axiological trust, the morality of others—including honesty and benevolence23 55 and instrumental trust, which concerns competence or reliability.55 We also accord trust to ‘secondary targets’, or sources of information about the trustworthiness of people or things, including reputation and credentials.55 As will be discussed, each of these trust targets and expectation types were important to participants.
Social contexts influence trust, partly by reinforcing trustworthy behavior.56 Cultural factors, such as the internalization of social norms, tell us how to respond to someone's investment of trust in us. Trust is also made possible when groups can monitor their members57 and enact social sanctions against them—whether or not this is actually done (‘network closure’). Our investments in ongoing relationships with others also facilitate trust.57 Sociological theory, therefore, identifies trust as both a cultural phenomenon and a network capability; both insights helped us interpret user requirements and translate them into a design framework.
Research aims and objectives
Using trust theory, we examine youth's intervention-relevant trust concerns and design preferences for a network-based informatics intervention focused on HIV/STI prevention. We aim to translate youth's perspectives into a trust-centered design framework to guide our own informatics intervention, as well as others focused on HIV/STI prevention for young African Americans.
Methods
Intervention context
We initiated a quasi-experimental intervention study to test a community-based HIV/STI prevention intervention's efficacy for African-American youth in a high prevalence area of Michigan. The intervention's offline components include ‘HOPE’ (HIV/sexually transmitted disease outreach, prevention and education) parties, at which young people host facilitated HIV/STI education sessions for themselves and the people in their ‘naturally occurring’ social networks. Face-to-face HOPE parties were created in 2000 by YOUR Center, a local, faith-based non-profit organization.58 The intervention's new informatics components are being developed to amplify the HOPE parties’ effects by giving participants tools to promote and support safer sex in their social networks. We plan to leverage the HOPE party networks through an informatics intervention that will reinforce normative messages regarding risk reduction and support safer sex goal achievement. The planned informatics intervention will include applications for existing social network systems used by HOPE party participants, such as Facebook and Twitter, and a suite of standalone tools on a HOPE party website (to include an associated mobile application). We report here on focus groups initiated to inform the design of this informatics intervention.
Study participants
This research was conducted in a midwestern, mid-sized urban area where young residents experience disproportionate HIV/STI rates.59 60 The county has unemployment and poverty rates above the state average,61 and the city's population is over 50% African American.61 Participants included 75 African Americans who averaged 18.3 years of age (see table 1). More than half (71%) were women. The majority (88%) were heterosexual; 12% were lesbian, gay, or bisexual (LGB). Fifty-seven per cent had not completed high school. The majority (67%) were students or unemployed.
Table 1.
Characteristics of study participants (n=75)
| Characteristics | Number | Percentage |
|---|---|---|
| Gender | ||
| Male | 22 | 29 |
| Female | 53 | 71 |
| Age | ||
| Mean/median | 18.3/18 | |
| Range | 14–25 | |
| Sexual orientation | ||
| Heterosexual | 66 | 88 |
| Gay/lesbian/bisexual | 9 | 12 |
| Education | ||
| Grade 8 or less | 3 | 4 |
| Grades 9–12, no diploma | 40 | 53 |
| High school graduate or equivalent | 11 | 15 |
| Some college | 16 | 21 |
| Associate or Bachelor's degree | 3 | 4 |
| No response | 2 | 3 |
| Employment | ||
| Full-time | 1 | 1 |
| Part-time | 15 | 20 |
| Unemployed or student | 50 | 67 |
| No response/other | 9 | 12 |
Research design
Between 2009 and 2010, we conducted 10 semistructured focus group interviews with African-American youth, including one for LGB participants. We chose the focus group method because it can elicit group-level assessments, meanings, and processes.62 The interviews, lasting from 90 min to 2 h, addressed young people's intervention-relevant perspectives and design preferences. The focus group discussion guide is published online as supplementary material to this paper. Focus groups had two facilitators and an average of eight participants. Participants were recruited through community-based organizations (CBO), churches, high schools, vocational programmes, and word of mouth. They completed a demographic survey and received a US$20 honorarium.
Focus groups were audio recorded and transcribed. Transcripts were analyzed deductively using sociological trust theory and inductively; both strategies used a qualitative content analytic approach63 within NVivo software. Initially, three sample focus group transcripts, selected for their age/gender diversity, were discussed by three research team members. Sociological trust concepts and emergent themes were identified and used to construct a preliminary codebook. Using this codebook, data were coded by one research team member (TCV) and the team discussed the results. Additional emergent themes were identified and incorporated into the codebook after discussion. Memos developed using these codes formed the basis of this paper.
Results
Intervention-relevant trust concerns
Personal and group trust
Participants expressed powerful expectations of morally questionable conduct by others in HIV/STI-related contexts, suggesting ‘personal trust’55 as a design concern. For youth, HIV/STI infection was a sign that people did not care about themselves (see table 2). Participants also believed that people took negative experiences out on others. This presumed vengefulness was evident in their belief that people with HIV/STI deliberately infect others. Therefore, participants felt that sharing rumors about people perceived as intentionally spreading the disease was almost a public service. Participants also believed people were dishonest—particularly about revealing their HIV/STI status. They contended that widespread infidelity and irresponsibility contributed to the burden of HIV/STI in their community. Participants stated that self-protection was therefore essential, ‘Since you can't trust nobody, you got to protect yourself’. Personal distrust was reinforced by distrust in the social groups to which residents belonged. Participants believed the social context, including unstable families and community disinvestment, supported immoral conduct.
Table 2.
Youths’ intervention-relevant trust concerns
| Personal trust (axiological/moral (dis)trust) | |
| Caring | ‘…if they cared they wouldn't have gotten it in the first place by having unprotected sex…’ |
| Vengefulness | ‘…there was going around a picture of a guy in (city name) passing around AIDS… I passed it on to everybody, because, he don't care…’ |
| Dishonesty | ‘If they do have disease, they're not really gonna tell you.’ |
| Infidelity | ‘…you can be with one person and they can do… other stuff… so having sex period… is putting yourself at risk.’ |
| Irresponsibility | ‘People are not being responsible here.… Everybody know everybody, everybody done did everybody.’ |
| Group trust (network closure/accountability) | |
| Family instability | ‘A lot of people don't care (for themselves) because they ain't got nobody to care for them.’ |
| Community disinvestment | ‘…everything leaving (city name)… it's not safe any more… like it can be with the STDs, it can be with the crime… we just don't care.’ |
| Institutional trust (benevolence) | |
| Government | ‘The Center of Disease Control, they know that African Americans are dying out… from HIV and AIDS. What are they doing about it?... sex education in seventh grade. It's like they want us to die out.’ |
| Healthcare providers | ‘P1: And I think some doctors just become doctors to be nasty. P2: And to get money. Some just, like I said, doctors get a paycheck. They don't really care…’ ‘…the (school) nurses… since they are ‘certified’ they cannot talk about you…’ |
| Teachers | ‘…teachers… know you, judge you, and they like to talk about you.’ |
| Churches | ‘…you don't talk about (sexuality) because it's supposedly bad… (with) that kind of an attitude… questions are shoved under the carpet.’ |
| CBO | ‘(Name of CBO)… they answer your questions, they're up front…’ |
| Technological trust | |
| Information technologies (privacy and safety) | |
| Social costs of HIV/STI-related information seeking | ‘…if we are embarrassed or it's too personal, we can… use the internet and not have to talk to people about it.’ |
| Technology-facilitated privacy breaches | ‘…the messages may be shown to other people… people may change your original text message…’ |
| Negative gossip | ‘When we do speak upon it, it's more of just gossip… what such and such done her.’ |
| Fighting | ‘…they're talking about who's sleeping with whose man. (The internet is) trouble.’ |
| Prevention technologies (instrumental (dis)trust) | |
| Reliability of condoms | ‘…no matter who it is… make sure you use a condom…’‘ The last time I learned about HIV and STDs is the…seventh grade… I learned that even though you use a condom, you can still get it.’ |
| Accuracy of HIV tests | ‘… before we get intimate or get serious, we should both go get checked together.’‘ …maybe you don't have it this time, maybe… it's sitting there in your body not coming out ‘til five years later. You turn thirty, how I got this? “I don't know.”’ |
| Trust in information (secondary targets of trust) | |
| Credentials of experts | ‘…you never know by touching hands, I know that you can't… but… I still don't want to touch it cause you, they might come up with a new invention, and it might come out in the air and you can get it…’ |
| Reputation and rumor | ‘They said most of the people in the (apartment complex) had it and trying to pass it down… a lot of people messing with the same person.’ ‘They be lying sometimes. They steal somebody's phone and just take a picture. And be like, “she got this. They got this. Don't mess with them”… they be mad at them.’ |
CBO, community-based organization; STD, sexually transmitted disease; STI, sexually transmitted infection.
Institutional trust
Participants doubted the benevolence of institutions in relation to their HIV/STI response. Some believed that the government did not care what happened to African Americans and that doctors had self-serving motives. However, nurses, especially those in schools, were thought to be more impartial and information shared with them would be confidential. Perceived judgment by teachers at school left some skeptical of school-based sex education (SBSE). Although churches were important to many, some youth felt that church-goers were judgmental regarding sexuality. CBO were viewed as more helpful than other organizations due to their honesty and HIV/STI awareness-building programmes.
Technological trust
Sociological theory asserts that trust ‘carries over’ between targets; similarly, youths’ personal trust concerns were amplified when communicating about HIV/STI with information technologies. Given the sensitive nature of HIV/STI issues, these concerns focused on privacy and safety. Therefore, while youth wanted better access to HIV/STI information, they perceived high social costs in looking for it. Participants feared technology-facilitated privacy breaches. For example, people said mobile phones may be stolen or ‘borrowed’, so personal messages could be viewed by others and easily forwarded, and sometimes altered in the process. With an intervention focus on HIV/STI, participants worried about the spread of negative gossip on the internet. This seemed plausible because such gossip frequently focused on sexuality, including allegations of promiscuity. Frequent online fighting was also a concern in an intervention context, because fighting often focused on infidelity accusations—sometimes accompanied by claims regarding HIV/STI transmission. Participants felt that the potential for online fighting was exacerbated by a lack of accountability on social media.
Participants’ technological trust also focused on HIV/STI prevention technologies, including condoms and HIV tests. For youth, suitable modes of HIV/STI prevention conformed largely to recommended strategies: limiting one's sexual partners, condom use, and HIV/STI screening. Although most advocated condom use, some youth distrusted the reliability of condoms—an ‘instrumental distrust’.55 Such fears may have been reinforced by SBSE that emphasized condom failure.64 Participants did not state whether their distrust of condoms was linked to condom failure experiences, but some felt they were insufficiently informed about effective condom use: ‘us in our community don't always get taught about lubrication… that's looked down upon, but… that could be why it's breaking.’
Similarly, many participants espoused the belief that HIV/STI testing was an important self-protective strategy. Several planned to get tested with any new partners. Test results were also seen as a reliable certification of disease-free status. Yet, a significant minority expressed distrust in HIV test results; this was linked to confusion about how long test results remained accurate and the time period between HIV infection and a positive test result.
Trust in information
As mentioned, sociological theory characterizes information as a ‘secondary’ target of trust.55 Participants reported inconsistent access to trusted information about HIV/STI. In a state where SBSE policy is decided locally, some youth went to schools that did not provide any SBSE. Adults often had difficulty speaking frankly with youth about sexual health. Participants said this left them with critical knowledge gaps, ‘(t)he education, the knowledge of how to catch the STDs are not there. We think we know but you really don't know.’ At times, people were forced to gain information from untrusted sources, ‘…growing up, I had to learn from the streets what an STD was.’
Furthermore, participants in four focus groups rejected the research-based information they had received about HIV transmission, advocating the view that HIV can spread through toilet seats, saliva, and shaking hands. These beliefs may be interpreted as a lack of trust in experts’ credentials, including those accorded by healthcare institutions.
For youth, information about others’ reputations was critical to HIV/STI-related decisions. Participants said that reputation-oriented rumors circulated consistently, rapidly and widely through mobile technologies. Some doubted the motives of people who circulated such rumors and questioned their veracity. Nevertheless, participants still avoided people thought to have HIV/STI, ‘I ain't gonna say I believe what this person is telling me… it might be true. It might not… but… I'll probably stay clear away from them.’
Design feature preferences
Participants’ design preferences often aligned with their aforementioned trust concerns, informing development of a trust-centered design framework that incorporates recommendations about intervention strategy and functionality (figure 1).
Figure 1.
Trust-centered design framework for informatics-based, social network intervention for HIV/sexually transmitted infections prevention.
Intervention strategy
Participants’ aforementioned perspectives on institutions suggested that CBO might provide trusted institutional affiliations for an intervention. As table 3 shows, participants wanted CBO to reach more people. Perhaps because of personal distrust, network embeddedness, including endorsement by trusted people, was also thought to be an ingredient of intervention success. Youth also wanted to participate in an intervention, from promoting it to writing blogs to educating younger people.
Table 3.
Trust-centered design preferences
| System strategy | |
| User needs and intervention objectives | |
| Institutional affiliation | ‘(CBOs)… are really… influential… as far as promoting awareness… but y'all could be more aggressive and get your names out more.’ |
| Network embeddedness | ‘…they be like “I ain't going it unless my boy doing it.” …Try to best suit how people is…’ |
| Participation | ‘…teach… you will feel better…’‘ Where we could write a blog.’ ‘Have us promote your website.’ |
| System functionality | |
| Functional specifications | |
| Credible Q&A services | ‘…if you're talking to somebody that you know is a… professional about it, you might get more facts.… Not just he said, she said.’ |
| Decision support | |
| Recommendations of condoms and lubrication, with use instructions | ‘…how to put a condom on… the proper ways.’ |
| Local resources | ‘…more places they felt comfortable that it was going to be confidential.’ |
| Identification of high-risk places | ‘…what area codes have more sexually transmitted disease(s)…’ |
| Identification of high risk people | ‘…the type of people who have… an STD…’ |
| Interactive risk assessment tools | ‘…different questions… when they answer it… tell them, “…you could be at a risk of this or at risk of that.”’ |
| Scenarios | ‘…what can result from what you're doing. Just scenarios. Like this happened, this happened.’ |
| Personal stories | ‘…get somebody they age that's going through the problem.’ ‘…people (with HIV/AIDS)… discuss… how they caught it… and how they're dealing with it and how everybody treating them from it.’ |
| Trustworthy people | ‘Trying to find out this about this. It'd have to be somebody you… trust.’ |
| Collective action | ‘When… it's something that can affect the black community… people want to be involved.’ |
| Positive social influence | ‘Why can't we have some positive peer pressure within the community?’ |
| Interaction design | |
| Optional anonymity | ‘…the option to either have a user name or just go on as “guest”.’ |
| Level of identifiability | ‘I don't want… my picture and my profile on a sexually transmitted disease website… Because everybody in (name of city) knows each other and stuff gets started real easily.’ ‘…anonymous discussion wouldn't be too bad where there's no picture.’ |
| Mobile messages | ‘…one of your friends might have your phone and then it gets around to everybody.’ |
| Offline networks | ‘I'd rather be in there… with my friend… he have my back or I got they back…’ ‘…we all interested to have… new friends… even a website buddy.’ |
| Supervision | ‘…it should be moderated… in case somebody who is just out there to find a site to start a mess.’ |
| Membership control | ‘You can report them, and… they can get booted off the site.’ |
| Blocking | ‘…I have to block somebody (on Facebook) today.’ |
CBO, community-based organization; Q&A, question and answer; STD, sexually transmitted disease.
Intervention functionality
The most desired intervention feature was credible information, provided via articles or question and answer (Q&A) services. In line with their institutional trust patterns, desired Q&A services might connect them to nurses or CBO staff. For example, youth responded positively to the prospect of texting questions to a nurse. The next most desired intervention functions were decision support aids. As per their inconsistent trust in prevention technologies, the most popular possibility was recommendations about condoms and lubrication, and videos on correct usage. Participants also wanted information about confidential local services, such as HIV/STI testing sites and sources of free condoms. Several wanted application features that would identify sources of risk, including specific people and neighborhoods. To help assess individual risk, participants requested scenarios and interactive evaluation tools. A few desired personal stories to give the information more life.
Participants wanted ‘good role models’ and other trustworthy people to be with them in an intervention. Relatedly, there was interest in creating profiles for couples. Although some youth preferred to connect online only with people they had met offline, a few felt open to making new, trustworthy friends in an intervention context. Several wanted an intervention to facilitate collective action to help the whole community get involved in prevention. A desire existed for positive social influence from peers to be part of an intervention.
Interaction design
Participants wanted optional anonymity when using an intervention and a choice regarding their level of identifiability (including online pseudonyms)—log-ins, profiles and friends should not be mandatory. They were also concerned about possible privacy breaches associated with unsolicited mobile messages. Therefore, they responded more positively to the idea of initiating mobile communication, such as with Q&A services.
Because participants worried about the potential for negative interactions, they looked to intervention providers to institute safety mechanisms. Participants expressed a desire for supervision, like moderation on a discussion board. For example, LGB youth feared discrimination and thought prevention would require supervision. Participants wanted to choose with whom they interacted. Membership control features, such as reporting, and individualized solutions, such as blocking, were mechanisms identified for doing so. Participants felt a connection to offline networks, such as partners and close friends, also increased online safety.
Discussion
Results of this study highlight a need to revisit the undifferentiated approaches to online trust that prevail in health informatics. Supporting a collective approach, trust issues were central to African-American young people. In line with a cultural interpretation, participants’ concerns referred to multiple targets. Their design preferences also went beyond established online trust-promoting strategies. As part of this, they advocated for intervention features, such as positive social influence and collective action, which align with sociological theory's insights regarding the collective basis of trust. Therefore, we present a new, trust-centered design framework for a network-based HIV/STI prevention informatics intervention with this population. This framework summarizes participants’ design preferences systematically, while conceptually organizing them with the aid of sociological theory's concept of trust targets.
A strength of our framework's theoretical grounding is that it aligns CHI intervention design with insights regarding the cultural basis of trust. Therefore, we offer interventionists an approach for addressing trust as a system of collective meaning, with the implication that designers should focus effort on connecting their CHI applications with a group's pre-existing cultural associations regarding trust. Furthermore, sociological trust theory asserts that there is a ‘carry over’ between varied trust targets, including those at different levels of social aggregation. This insight highlights the importance of the social context of a CHI intervention regarding HIV/STI to its acceptance. Related design choices echo work in non-health contexts to build trust by leveraging offline relationships.65 66 However, our framework goes further in suggesting that interventionists should concern themselves with positioning their efforts in collaboration with people and institutions that young African Americans already trust. Such concerns broaden the lens of traditional CHI application design practice, and extend health informatics investigations of trust beyond the better articulated area of data security.
To address technological trust, our framework proposes a new application area for user reference aggregation. Decision support features, such as recommender systems, could address instrumental distrust in condoms and HIV/STI tests by providing reviews or ratings of them, and the personal value of risk-reduction behaviors. Such aggregate recommendations may facilitate well-placed trust in prevention technologies and behaviors, while exerting positive social influence. For example, participants’ interpersonal distrust can be read partly as a critique of behavioral norms in their community. Yet, publicly available normative information concerning HIV/STI is limited because preventive behaviors, such as condom use, are typically pursued privately.67 Online recommendations may facilitate the communication and visibility68 of norms, making them more amenable to deliberate change.
Following sociological theory, our framework contends that an intervention could influence group trust by facilitating network closure, with ‘trustworthy’ behavior being a potential result. Therefore, sociological trust theory provides a theoretical basis for designing CHI interventions that promote group monitoring and accountability. In our case, building on youths’ desire for participation, an intervention could provide youth with opportunities to disclose their HIV/STI-related intentions and actions voluntarily, perhaps through a Facebook application or standalone reputation system. As requested, and building on couple-centered HIV/STI prevention,69 an intervention could also allow couples to share information about their commitments. Such public statements could hold people accountable to themselves and others. Although the success of such approaches requires positive youth involvement, this could be facilitated by training and support. For our intervention, the availability of a cadre of educated HOPE party participants offers advantages.
Trust-centered design aligns with contextual models of sexual health that treat youth risk behavior as the endpoint of influences including peer networks, families, communities, and institutions.70 Using sociological trust theory as a basis for design, an intervention could address such contextual risk factors through (as youth requested) collective action, thus building on findings from community informatics71 72 and offline interventions that created health-based social movements.73 Young people could thus be moderators of web-based discussion, conduct outreach, or disseminate pro-safer sex messages through their online social networks. There may also be a place for online activism that engages the wider community, such as e-petitions or online event organizing.
Our design framework is unique in explicitly addressing reliance on rumors for HIV/STI-related decision-making. Rumor circulation is unsurprising given participants’ perceptions of authoritative risk information. Rumors are ‘unverified and instrumentally relevant information statements’74 that emerge when information is unavailable or distrusted.75 Therefore, a plausible solution would be, as requested, to provide the aforementioned Q&A services. User responsiveness is an established approach for engendering online trust,32 38 and appropriate professional involvement may confer credibility. Because mobile technologies are used most often to search for HIV/STI information,76 a mobile platform may be appropriate—if youth initiate this communication.
As per previous informatics research,32 an intervention should give participants a choice about their anonymity and identifiability. Nevertheless, participants wanted to interact at an online HIV/STI prevention intervention with trustworthy people. Youth could thus be encouraged to recruit their trusted friends to participate, and interventionists could offer offline activities that allow youth to build relationships before online engagement. For our intervention, the offline HOPE parties offer a useful platform for this. The training and support of good role models, such as HOPE party hosts, and the involvement of professionals could help ensure desired interactions. Still, the preponderance of negative online behavior77 reinforced the need for institutionally supported safety components, such as supervision and blocking.
Several limitations of this paper should be noted. We conducted focus groups with African-American youth in one city. Therefore, we are unable to generalize results to a wider population. The study also focused on HIV/STI, conditions with unique social characteristics that may have heightened trust-related concerns. Therefore, generalizability to other health issues is unknown. The majority of our sample was female; young women may be more sensitive to trust and safety issues than young men. People concerned with trust might seek a role in designing our informatics intervention. However, the theme of trust emerged in all focus groups, despite the stated purpose of simply helping to design an HIV/STI prevention intervention. Participants’ trust in CBO should also be interpreted in light of a CBO's role in hosting several focus groups. Although external confirmation is required, results informed the development of a novel design framework that offers much-needed insight into the culturally specific design requirements of young African Americans in the context of HIV/STI prevention. We will apply this design framework in ongoing intervention design, and look forward to tracking its potential contribution to intervention acceptance and use.
Moreover, in contrast to previous work, our results demonstrate the potential value of adopting a collective approach to trust within the CHI field. While perhaps particularly important within our study context, we contend that trust-centered design holds promise for better reaching socioeconomically marginalized groups whose challenging life circumstances may render questions of trust and distrust central to daily living.
Conclusion
Trust is a critical, multifaceted concern for young African Americans as they consider using an informatics intervention for HIV/STI prevention. Participants’ concerns extended beyond those typically considered in the context of online trust. Based on consistent expression of such trust issues, we presented a new, trust-centered design framework as a contribution to the field of culturally informed design. Our approach holds promise for more effective engagement of African-American youth in informatics interventions for HIV/STI prevention, as well as, potentially, other groups and health contexts in which trust must be intentionally cultivated.
Acknowledgments
The authors would like to thank Kai Zheng for his review of an early version of this manuscript. They also wish to thank the participants, who generously and honestly shared their perspectives regarding a challenging topic.
Footnotes
Contributors: TCV and DJK designed the study with input from TRC and AG. TRC collected data. TCV, TRC, DJK and AG analyzed the data. TCV wrote the initial manuscript, which was then revised by TCV, TCR, DJK and AG. All authors had full access to all of the data in the study and can take responsibility for the integrity of the data and the accuracy of the data analysis. All authors approved the final version of the manuscript.
Funding: This publication was supported by the Prevention Research Center of Michigan cooperative agreement no 1-U48-DP-001901 from the Centers for Disease Control and Prevention. Funding was also provided by the Michigan Institute for Clinical and Health Research through NIH grant #UL1RR024986. The research reported here does not necessarily represent the official positions of the Centers for Disease Control and Prevention or the National Institutes of Health.
Competing interests: None.
Ethics approval: This study received ethics approval from the University of Michigan, Health Sciences and Behavioral Sciences Institutional Review Board.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Weinstock H, Berman S, Cates W. Sexually transmitted diseases among american youth: incidence and prevalence estimates, 2000. Perspect Sex Reprod Health 2004;36:6–10 [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention Diagnoses of HIV Infection and AIDS in the United States and Dependent Areas, 2010. http://www.cdc.gov/hiv/surveillance/resources/reports/2010report/ (accessed 10 Mar 2013).
- 3.Ellen JM, Aral SO, Madger LS. Do differences in sexual behaviors account for the racial/ethnic differences in adolescents’ self-reported history of a sexually transmitted disease? Sex Transm Dis 1998;25:125–9 [DOI] [PubMed] [Google Scholar]
- 4.Jennings J, Glass B, Parham P, et al. Sex partner concurrency, geographic context, and adolescent sexually transmitted infections. Sex Transm Dis 2004;31:734–9 [DOI] [PubMed] [Google Scholar]
- 5.Aral SO. Sexual network patterns as determinants of STD rates: paradigm shift in the behavioral epidemiology of STDs made visible. Sex Transm Dis 1999;26:262–4 [DOI] [PubMed] [Google Scholar]
- 6.Doljanac RF, Zimmerman MA. Psychosocial factors and high-risk sexual behavior: race differences among urban adolescents. J Behav Med 1998;21:451–67 [DOI] [PubMed] [Google Scholar]
- 7.Stanton B, Li X, Pack R, et al. Longitudinal influence of perceptions of peer and parental factors on African American adolescent risk involvement. J Urban Health 2002;79:536–48 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doherty IA, Padian NS, Marlow C, et al. Determinants and consequences of sexual networks as they affect the spread of sexually transmitted infections. J Infect Dis 2005;191(Suppl. 1):S42–54 [DOI] [PubMed] [Google Scholar]
- 9.Coates TJ, Richter L, Caceres C. Behavioural strategies to reduce HIV transmission: how to make them work better. Lancet 2008;372:669–84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Freeman B, Chapman S. Gone viral? Heard the buzz? A guide for public health practitioners and researchers on how Web 2.0 can subvert advertising restrictions and spread health information. J Epidemiol Community Health 2008;62:778–82 [DOI] [PubMed] [Google Scholar]
- 11.Chiasson MA, Hirshfield S, Rietmeijer C. HIV prevention and care in the digital age. J Acquir Immune Defic Syndr 2010;55:S94–S7 [DOI] [PubMed] [Google Scholar]
- 12.Wang K, Brown K, Shen S-Y, et al. Social network-based interventions to promote condom use: a systematic review. AIDS Behav 2011;15:1298–308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Latkin C, Mandell W, Vlahov D, et al. The long-term outcome of a personal network-oriented HIV prevention intervention for injection drug users: the SAFE study. Am J Community Psychol 1996;24:341–64 [DOI] [PubMed] [Google Scholar]
- 14.Latkin CA, Sherman S, Knowlton A. HIV prevention among drug users: outcome of a network-oriented peer outreach intervention. Health Psychol 2003;22:332–9 [DOI] [PubMed] [Google Scholar]
- 15.Bailey JV, Murray E, Rait G, et al. Interactive computer-based interventions for sexual health promotion. Cochrane Database Syst Rev 2010;8:1–81 [DOI] [PubMed] [Google Scholar]
- 16.Bennett GG, Glasgow RE. The delivery of public health interventions via the internet: actualizing their potential. Annu Rev Public Health 2009;30:273–92 [DOI] [PubMed] [Google Scholar]
- 17.Bull SS, Breslin LT, Wright EE, et al. Case study: an ethics case Study of HIV Prevention Research on Facebook: the Just/Us Study. J Pediatr Psychol 2011;36:1082–92 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jaganath D, Gill HK, Cohen AC, et al. Harnessing online peer education (HOPE): integrating C-POL and social media to train peer leaders in HIV prevention. AIDS Care 2011;24:593–600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Montague E, Perchonok J. Health and wellness technology use by historically underserved health consumers: systematic review. J Med Internet Res 2012;14:e78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gibbons MC, Wilson RF, Samal L, et al. Impact of consumer health informatics applications. Rockville, MD: Agency for Healthcare Research and Quality, 2009 [Google Scholar]
- 21.Johnson B, Redding C, DiClemente R, et al. A network-individual-resource model for HIV prevention. AIDS Behav 2010;14:204–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Möllering G. The trust/control duality. Int Sociol 2005;20:283–305 [Google Scholar]
- 23.McKnight D Harrison, Chervany N. Trust and distrust definitions: one bite at a time. In: Falcone R, Singh M, Tan Y-H, eds. Trust in cyber-societies. Berlin: /Heidelberg: Springer, 2001: 27–54 [Google Scholar]
- 24.Manning WD, Flanigan CM, Giordano PC, et al. Relationship dynamics and consistency of condom use among adolescents. Perspect Sex Reprod Health 2009;41:181–90 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bauman LJ, Berman R. Adolescent relationships and condom use: trust, love and commitment. AIDS Behav 2005;9:211–22 [DOI] [PubMed] [Google Scholar]
- 26.Eyre SL, Flythe M, Hoffman V, et al. Primary relationship scripts among lower-income, African American young adults. Fam Process 2012;51:234–49 [DOI] [PubMed] [Google Scholar]
- 27.Jadack RA, Fresia A, Rompalo AM, et al. Reasons for not using condoms of clients at urban sexually transmitted diseases clinics. Sex Transm Dis 1997;24:402–8 [DOI] [PubMed] [Google Scholar]
- 28.Kershaw TS, Ethier KA, Niccolai LM, et al. Misperceived risk among female adolescents: social and psychological factors associated with sexual risk accuracy. Health Psychol 2003;22:523–32 [DOI] [PubMed] [Google Scholar]
- 29.Jimison H, Gorman PN, Nygren P, et al. Barriers and drivers of health information technology use for the elderly, chronically ill and underserved. Rockville, MD: Agency for Healthcare Research and Quality, 2009 [PMC free article] [PubMed] [Google Scholar]
- 30.Kim B, Han I. The role of trust belief and its antecedents in a community-driven knowledge environment. J Am Soc Inf Sci Technol 2009;60:1012–26 [Google Scholar]
- 31.Song J, Zahedi FM. Trust in health infomediaries. Decis Support Syst 2007;43:390–407 [Google Scholar]
- 32.Leimeister JM, Ebner W, Krcmar H. Design, implementation, and evaluation of trust-supporting components in virtual communities for patients. J Manag Info Syst 2005;21:101–31 [Google Scholar]
- 33.Ridings CM, Gefen D, Arinze B. Some antecedents and effects of trust in virtual communities. J Strateg Info Syst 2002;11:271–95 [Google Scholar]
- 34.Patel VN, Abramson E, Edwards AM, et al. Consumer attitudes toward personal health records in a beacon community. Am J Manag Care 2011;17:e104–20 [PubMed] [Google Scholar]
- 35.Or CKL, Karsh B-T. A systematic review of patient acceptance of consumer health information technology. J Am Med Inform Assoc 2009;16:550–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sillence E, Briggs P, Harris P, et al. Health Websites that people can trust—the case of hypertension. Interact Comput 2007;19:32–42 [Google Scholar]
- 37.Kukafka R, Khan SA, Hutchinson C, et al. Digital partnerships for health: steps to develop a community-specific health portal aimed at promoting health and well-being. AMIA Annu Symp Proc 2007:428–32 [PMC free article] [PubMed] [Google Scholar]
- 38.Fan H, Smith SP, Lederman R, et al. Why people trust in online health communities: an integrated approach. 21st Australasian Conference on Information Systems; 1–10 December 2010 Brisbane, Australia [Google Scholar]
- 39.Resnick P, Varian HR. Recommender systems. Commun ACM 1997;40:56–8 [Google Scholar]
- 40.Beldad A, de Jong M, Steehouder M. How shall I trust the faceless and the intangible? A literature review on the antecedents of online trust. Comput Human Behav 2010;26:857–69 [Google Scholar]
- 41.Smith SS. Race and trust. Annu Rev Sociol 2010;36:453–75 [Google Scholar]
- 42.Bodker K, Pedersen JS. Workplace cultures: looking at artifacts, symbols, and practices. In: Greenbaum JM, Kyng M, eds. Design at work: cooperative design of computer systems. Hillsdale, NJ: L. Erlbaum Associates, 1991: 121–36 [Google Scholar]
- 43.Armstrong K, McMurphy S, Dean L, et al. Differences in the patterns of health care system distrust between blacks and whites. J Gen Intern Med 2008;23:827–33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.O'Malley AS, Sheppard VB, Schwartz M, et al. The role of trust in use of preventive services among low-income African-American women. Prev Med 2004;38:777–85 [DOI] [PubMed] [Google Scholar]
- 45.Musa D, Schulz R, Harris R, et al. Trust in the health care system and the use of preventive health services by older black and white adults. Am J Public Health 2009;99:1293–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gibbons M, Wilson R, Samal L, et al. Consumer health informatics: results of a systematic evidence review and evidence based recommendations. Transl Behav Med 2011;1:72–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yamin CK, Emani S, Williams DH, et al. The digital divide in adoption and use of a personal health record. Arch Intern Med 2011;171:568–74 [DOI] [PubMed] [Google Scholar]
- 48.Roblin DW, Houston Ii TK, Allison JJ, et al. Disparities in use of a personal health record in a managed care organization. J Am Med Inform Assoc 2009;16:683–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ancker J, Barrón Y, Rockoff M, et al. Use of an electronic patient portal among disadvantaged populations. J Gen Intern Med 2011;26:1117–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Sarkar U, Karter AJ, Liu JY, et al. Social disparities in internet patient portal use in diabetes: evidence that the digital divide extends beyond access. J Am Med Inform Assoc 2011;18:318–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Fox S. The social life of health information, 2011. Washington, DC: Pew Internet and American Life Project, 2011. [April 30, 2012]. http://www.pewinternet.org/Reports/2011/Social-Life-of-Health-Info.aspx (accessed 10 Mar 2013). [Google Scholar]
- 52.Spooner T, Rainie L. African-Americans and the Internet Washington, DC: Pew Internet and American Life Project, 2000. http://www.pewinternet.org/Reports/2000/AfricanAmericans-and-the-Internet.aspx (accessed 10 Mar 2013). [Google Scholar]
- 53.Gibbons M Christopher. Use of health information technology among racial and ethnic underserved communities. Perspect Health Inf Manag 2011;8:1f. [PMC free article] [PubMed] [Google Scholar]
- 54.Valdez R, Gibbons M, Siegel E, et al. Designing consumer health IT to enhance usability among different racial and ethnic groups within the United States. Health Technol 2012;2:225–33 [Google Scholar]
- 55.Sztompka P. Trust: a sociological theory. Cambridge, New York: Cambridge University Press, 1999 [Google Scholar]
- 56.Dunn J. The concept of ‘trust’ in the politics of John Locke. In: Rorty R, Schneewind JB, Skinner Q, eds. Philosophy in history: essays on the historiography of philosophy. Cambridge, UK: Cambridge University Press, 1984: 279–302 [Google Scholar]
- 57.Hardin R. Trust. Cambridge, UK; Malden, MA: Polity, 2006 [Google Scholar]
- 58.Griffith DM, Pichon LC, Campbell B, et al. YOUR Blessed Health: a faith-based CBPR approach to addressing HIV/AIDS among African Americans. AIDS Educ Prev 2010;22:203–17 [DOI] [PubMed] [Google Scholar]
- 59.Michigan Department of Community Health January 2011 Quarterly HIV/AIDS Analysis. Lansing, MI: MDCH, 2011. [March 7, 2011]. [Google Scholar]
- 60.Michigan Department of Community Health Michigan sexually transmitted diseases database. Lansing, MI: MDCH, 2011. http://www.mdch.state.mi.us/pha/osr/chi/STD_H/frame.html (accessed 10 Mar 2013). [Google Scholar]
- 61.US Census Bureau Fact Sheet [by city]. Washington, DC: U.S. Census Bureau, 2000. http://factfinder2.census.gov/faces/nav/jsf/pages/index.xhtml (accessed 10 Mar 2013). [Google Scholar]
- 62.Bloor M. Focus groups in social research. London, UK: Sage, 2001 [Google Scholar]
- 63.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res 2005;15:1277–88 [DOI] [PubMed] [Google Scholar]
- 64.Kimmel A, Williams T, Veinot TC, et al. “I make sure I am safe and I make sure I have myself in every way possible”: African-American Youth Perspectives on Sexuality Education. Sex Educ 2013;1:172–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fogg BJ, Soohoo C, Danielson DR, et al. How do users evaluate the credibility of Web sites?: a study with over 2500 participants. Proceedings of the 2003 Conference on Designing for User Experiences; San Francisco, California: 997097: ACM, 2003: 1–15 [Google Scholar]
- 66.Stuart HC, Dabbish L, Kiesler S, et al. Social transparency in networked information exchange: a theoretical framework. Proceedings of the ACM 2012 Conference on Computer Supported Cooperative Work; Seattle, Washington, USA: 2145275: ACM, 2012: 451–60 [Google Scholar]
- 67.Latkin CA, Knowlton AR. Social network approaches to HIV prevention: implications to community impact and sustainability. In: Trickett EJ, Pequegnat W, eds. Community interventions and AIDS. New York: Oxford University Press, 2005: 105–29 [Google Scholar]
- 68.Kraut RE, Resnick P, Kiesler S. Building successful online communities: evidence-based social design. Cambridge, Mass: MIT Press, 2011 [Google Scholar]
- 69.Burton J, Darbes L, Operario D. Couples-focused behavioral interventions for prevention of HIV: systematic review of the state of evidence. AIDS Behav 2010;14:1–10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.DiClemente R, Wingood G, Crosby R. A contextual perspective for understanding and preventing STD/HIV among adolescents. In: Romer D, ed. Reducing adolescent risk: toward an integrated approach. Thousand Oaks, Calif: Sage Publications, 2003: 366–73 [Google Scholar]
- 71.Cohill A, Kavanagh A. Community networks: lessons from Blacksburg,Virginia. Boston, Mass: Artech House, 1997 [Google Scholar]
- 72.Hampton KN. Internet use and the concentration of disadvantage: glocalization and the urban underclass. Am Behav Sci 2010;53:1111–32 [Google Scholar]
- 73.Yoshikawa H, Wilson PA, Peterson JL, et al. Multiple pathways to community-level impacts in HIV prevention: implications for conceptualization, implementation, and evaluation of interventions. In: Trickett EJ, Pequegnat W, eds. Community interventions and AIDS. New York: Oxford University Press, 2005: 28–55 [Google Scholar]
- 74.DiFonzo N, Bordia P. Rumor, gossip and urban legends. Diogenes 2007;54:19–35 [Google Scholar]
- 75.Shibutani T. Improvised news; a sociological study of rumor. Indianapolis: Bobbs-Merrill, 1966 [Google Scholar]
- 76.Fox S. Health topics. Washington, DC: Pew Internet and American Life Project, 2011. http://pewinternet.org/Reports/2011/HealthTopics.aspx (accessed 10 Mar 2013). [Google Scholar]
- 77.Veinot TC, Campbell TR, Kruger D, et al. Drama and danger: the opportunities and challenges of promoting youth sexual health through online social networks. AMIA Annu Symp Proc 2011:1–10 [PMC free article] [PubMed] [Google Scholar]