Abstract
Granular cell tumour, also known as Abrikossoff tumour, is a relatively uncommon benign neoplasm, which is more commonly found in females in the 4th to 6th decades of life even though it can occur in all ages.
It occurs in all areas of the body but about 45–65% of all lesions are reported in the head and neck region. Intraoral lesions represent about 70% of the granular cell tumours of the head and neck, and account for 1/3 of all cases affecting the whole body.
Most of the intraoral lesions occur on the tongue, usually on the lateral aspect, followed by the buccal mucosa and hard palate. Although majority of granular cell tumours are benign, some are clinically aggressive and a few frankly malignant forms have been reported. Some benign lesions exhibit surface ulcerations and this clinical appearance, combined with the overlying pseudoepitheliomatous hyperplasia, seen histologically, may lead to misdiagnosis of malignancy if adequate biopsy material was not taken.
A case of granular cell tumour which occurred on the midline area of the dorsum of the posterior 1/3 of the tongue is reported in a 20-year-old female patient. It is interesting because the patient was younger than the average age of occurrence and the tumour occurred in a similar site to that of a lingual thyroid.
Keywords: Granular cell tumour, Pseudoepitheliomatous hyperplasia, Squamous cell carcinoma of tongue, Lingual thyroid, Dorsum of posterior one-third of tongue
1. Introduction
Granular cell tumour is a rare benign soft tissue neoplasm of unknown aetiology (Regezi and Scuibba, 2003), first described in a patient with a lesion on the tongue by Abrikossoff (1926). He named it granular cell myoblastoma at the time because of the apparent association between granular cell and skeletal muscle.
Granular cell tumour can occur in all parts of the body, with about 45–65% of all reported cases occurring in the head and neck region (Eguia et al., 2006; Nagaraj et al., 2006; Sposto et al., 2006). Although granular cell tumours have been reported in all age groups ranging from 11 months to 85 years, most cases generally occur between the 4th and 6th decades of life (Nagaraj et al., 2006; Sposto et al., 2006; Rubinstein et al., 1987). However, in a literature review, Becelli et al. (2001) reported an age range between the 2nd and 6th decades of life with an average age of 50 years. In all these studies there was a general consensus that the granular cell tumours were rare in children.
Granular cell tumours are generally reported to be about 2–3 times more common in females than males (Eguia et al., 2006; Nagaraj et al., 2006; Sposto et al., 2006; Becelli et al., 2001; Naief et al., 1997; Nishida et al., 2000), however, other authors have not found any gender differences (Billeret-Lebranchu, 1999). They are more prevalent in black patients than whites by a ratio of 3:1 (Sposto et al., 2006; Becelli et al., 2001; Zangari et al., 1996).
The intraoral lesions represent about 70% of the granular cell tumours involving the head and neck, and account for 1/3 of all cases occurring in the body (Becelli et al., 2001). In the oral cavity, the tongue is the most common site followed, in the order of frequency, by the buccal mucosa and hard palate (Sposto et al., 2006; Becelli et al., 2001). On the tongue, 48% occur in the dorsum, 15% on the lateral border and the rest on the ventral surface. Other reported intraoral sites include the lip, gingivae, hard palate and the uvula (Becelli et al., 2001; Regezi et al., 1979; Lamey et al., 1987).
Eguia et al. (2006) reported eight cases of granular cell tumours of the oral cavity with a 62.5% (5) female involvement compared to 37.5% male involvement, and 75% (6) occurrence on the tongue, one in lower gingiva and one in buccal mucosa. Sposto et al. (2006) also reported three cases of granular cell tumour of the tongue all of which involved female patients with age range between 30 years and 42 years.
Recently, most of the lingual lesions have been reported to occur on the lateral border of the dorsum of the tongue (Eguia et al., 2006). Therefore, the purpose of this paper was to report a case of granular cell tumour of the tongue, in a 20-year-old female patient, which occurred on the dorsum of the tongue and mimicked ectopic lingual thyroid, and also to review the literature on the lesion.
2. Case report
A 20-year-old female patient was referred by the dental surgeon to the Department of Oral and Maxillofacial Surgery in King Khalid Hospital, Najran, Saudi Arabia complaining of a swelling on the dorsum of the tongue of about 6 months duration which was slowly getting bigger and painful. She also complained of enlarged swelling in the thyroid region.
Her past medical history was unremarkable. Physical examination revealed a firm, well-circumscribed and slightly tender lump on the right side of midline of the dorsum of the posterior 1/3 of the tongue at its junction with the anterior 2/3 of tongue (near the foramen caecum). There was also a non-tender swelling in the midline of the neck, which moved on swallowing.
The differential diagnosis of the lingual lump, considered at the time, included granular cell tumour, lingual thyroid, schwannoma, neurofibroma, irritational fibroma and lipoma.
In view of the enlarged lump in neck, the patient was referred to the general surgeon for opinion concerning the thyroid gland. Ultrasound scan of the thyroid gland as well as thyroid function test (TSH, T3, T4) were reported as normal. 99mTC pertechnetate scan of the thyroid showed slightly enlarged thyroid gland in the normal anatomical position with uniform distribution of the radionuclide. No discrete “hot” or “cold spots” (nodules) were seen. The swelling on the tongue did not appear to concentrate any radioactivity thus ruling out ectopic thyroid gland.
The lump on the tongue was excised under local anaesthesia. The histopathology report was as follows: “pseudoepitheliomatous hyperplasia of the stratified squamous epithelium beneath which are large polyhedral cells with acidophilic granular cytoplasm and pyknotic nuclei. Surrounding muscle fibres are also evident. These features are consistent with granular cell tumour” (Figs. 1–3).
Figure 1.

Photomicrograph of the lesion showing pseudoepitheliomatous hyperplasia of the overlying stratified squamous epithelium. H&E stain (scanner view).
Figure 2.

Photomicrograph of the lesion showing granular cells in close proximity to the skeletal muscle in the connective tissue. H&E stain. Magnification 10×.
Figure 3.
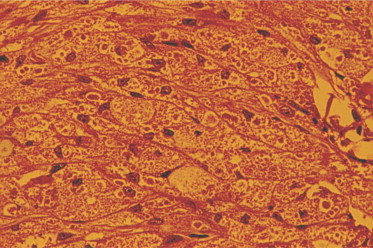
Photomicrograph of the lesion showing large polyhedral cells with acidophilic granules. H&E stain. Magnification 20×.
There was no sign of recurrence of the lesion 3 years postoperatively but the patient stopped attending the clinic and has not been back for 7 years now.
3. Discussion
Granular cell tumour, also known as Abrikossoff tumour, is slow growing and usually asymptomatic and often discovered accidentally. It usually presents as a small single submucosal nodular mass, about 1–3 cm in size, hard in consistency and usually covered by intact mucosa (Regezi and Scuibba, 2003; Nagaraj et al., 2006; Sposto et al., 2006). However, large lesions have been reported, including a case of an extensive granular cell tumour which occupied the right side of the palate from the central incisor to the soft palate (Becelli et al., 2001). Some large lesions may show surface ulcerations which may give a clinical impression of a malignant neoplasm. The ulceration in such cases is usually due to local trauma (Regezi and Scuibba, 2003).
Most granular cell tumours are found on the head and neck region with the tongue as the most common location with 23–28% of cases (Sposto et al., 2006). On the tongue, the granular cell tumour usually occurs on the postero-lateral aspect, in a position similar to the usual site of occurrence of squamous cell carcinoma, and may present with similar symptoms, especially, when the surface of the lesion is ulcerated (Sposto et al., 2006).
In addition, the tongue lesions characteristically show loss of gustatory papillae and atrophy of the overlying mucosa. This modification of the overlying mucosa in the lingual lesions is especially important because the clinical appearance can also mimic a carcinoma (Eguia et al., 2006). This is another reason why some cases were initially suspected of being squamous cell carcinoma until proved otherwise by histopathological examination (Eguia et al., 2006).
Although granular cell tumour generally occurs as a single small submucosal nodule, multiple lesions have been reported (Sposto et al., 2006; Collins and Jones, 1995). These multiple lesions account for about 5–25% of all cases of granular tumours (Becelli et al., 2001; Zangari et al., 1996; Collins and Jones, 1995; Pressor and Chung, 1980; Apisarnathanarax, 1981) and are seen more in black women (Becelli et al., 2001; Collins and Jones, 1995; Pressor and Chung, 1980; Apisarnathanarax, 1981). Sometimes a patient, who presents initially with a solitary lesion, can develop multiple lesions later (Collins and Jones, 1995). Rifkin et al. (1986) observed that multiple tumours may be found in up to 20% of black patients who present initially with a solitary granular cell tumour.
In addition to the oral mucosa, granular cell tumours are also seen in skin, gastrointestinal tract, respiratory tract, biliary system, larynx, male and female reproductive tracts (Sposto et al., 2006; Collins and Jones, 1995), as well as other sites in the head and neck region including the orbit, larynx, parotid gland and peripheral and cranial nerves (Sposto et al., 2006; Collins and Jones, 1995).
Differential diagnosis of granular cell tumour should include benign connective tissue and neural tumours such as fibromas, lipomas, neuromas, neurofibromas or schwannomas with their malignant variants, minor salivary gland tumours and even oral carcinomas (Eguia et al., 2006; Sposto et al., 2006). In the case reported here, the location of the lesion in the midline of the tongue near the foramen caecum aroused the suspicion of lingual thyroid and was therefore, included in the differential diagnosis but was ruled out after the thyroid scan excluded thyroid tissue.
The aetiology of granular cell tumour has generated a lot of controversies in the past. It was originally thought to arise from striated muscle, histiocytes, fibroblasts, myoepithelium and nerve cell connective tissue (Rubinstein et al., 1987; Collins and Jones, 1995; Noonan et al., 1979). Because of the uncertainty surrounding its aetiology, granular cell tumour, has, in the past, been variously referred to as granular cell myoblastoma, granular cell neurofibroma or granular cell schwannoma (Eguia et al., 2006). But it is now believed that the unique granular cells that make up the lesion are of neural (primitive schwann cell) origin, predominantly, on the basis of immunochemical studies which have localised neuron-specific enolase and S-100 protein markers on the tumour cells (Regezi and Scuibba, 2003; Eguia et al., 2006; Nagaraj et al., 2006; Becelli et al., 2001; Collins and Jones, 1995).
Histologically, granular cell tumour is poorly circumscribed and is composed of numerous strands and sheets of large polyhedral cells, 30–60 μm in diameter, with distinct cellular membrane. The individual cells have abundant pale cytoplasm filled with numerous eosinophilic coarse granules and small round or oval nuclei, often containing one or two nucleoli. These granular cells merge with the surrounding tissue and, especially in the lingual lesions, seem to be in intimate association with striated muscle, giving the impression that they arise from these structures (Zangari et al., 1996). However, Azzopardi (1956), pointed out that more than 50% of granular cell tumours were found in tissues not containing striated muscle fibres.
The overlying epithelium frequently presents with proliferative histologic pattern which may be so extensive as to show horn-pearl formation and which has been described as pseudoepitheliomatous hyperplasia. Some authors have reported 87% incidence of pseudoepitheliomatous hyperplasia in the overlying epithelium (Eguia et al., 2006). In other studies, however, cases with pseudoepitheliomatous hyperplasia were not so high and did not exceed 50% (Naief et al., 1997; Nishida et al., 2000).
In lesions involving the tongue, the pseudoepitheliomatous hyperplasia may be so pronounced that it may be interpreted as squamous cell carcinoma (Regezi and Scuibba, 2003; Nagaraj et al., 2006). Such misdiagnosis may result in improper treatment, especially, if the fragment of tissue obtained from incisional biopsy is either too small or too superficial (Sposto et al., 2006; Van Der Wal et al., 1989). In this regard, the method of obtaining tissue by fine needle aspiration biopsy to diagnose granular cell tumour as reported by Nagaraj et al. (2006) would appear inherently unreliable.
Although granular cell tumours are benign, about 10% of cases show clinically malignant behaviour (Lack et al., 1980) and less than 2% of cases have distant metastasis (Eguia et al., 2006; Sposto et al., 2006; Nishida et al., 2000; Guilliani et al., 2004).
Some authors have suggested that the distinction between benign and malignant types is fairly difficult because there is striking histological similarity between both varieties and a lack of reliable criteria to provide a prediction of development of a malignant behaviour (Sposto et al., 2006) and therefore, only the presence of regional and distant metastasis will aid in the differentiating benign granular cell tumour from its malignant counterpart (Nagaraj et al., 2006). However, other authors report that malignancy of granular cell tumour is suggested by its rapid growth, broad dimensions (>4 cm) and the presence of necrotic and haemorrhagic areas, high mitotic index and cellular and nuclear pleomorphism (Becelli et al., 2001; Lack et al., 1980). Cases of metastasis of malignant granular cell tumour have been discovered 14 years after the identification of the primary lesion (Becelli et al., 2001).
The actual co-existence of granular cell tumours and squamous cell carcinomas is rare but well documented Naief et al. (1997), in a review of the literature, found 13 cases of granular cell tumours associated with carcinomas and reported the first case of its kind in the oral cavity, involving the tongue.
Surgical excision is the treatment of choice for granular cell tumour, regardless of whether the lesion is solitary or multifocal (Collins and Jones, 1995) and since the granular cell tumour has poorly defined margin, the recommended treatment is excision with a margin of safety (Eguia et al., 2006). In most cases this treatment results in cure.
Recurrence is uncommon and is, frequently, a result of incomplete excision of the original lesion (Guilliani et al., 2004). However, Becelli et al. (2001) reported only 15% recurrence rate following incomplete excision while Lack et al. (1980) reported that 19 out of 48 cases of incompletely excised margins did not have any recurrence.
The malignant granular cell tumours are reported to develop 31–41% local recurrence and 50–63% distant metastasis and therefore, the most effective treatment is wide excision with 2–3 cm of margin but in the oral cavity, where tissue preservation is essential, Mohs’ micrographic surgery is indicated (Sposto et al., 2006).
Radiation and chemotherapy are not recommended for the benign lesions because of the resistance of the tumour and potential carcinogenic effect of such treatment (Nagaraj et al., 2006), but are recommended for treatment of malignant forms of the lesion (Becelli et al., 2001). Spontaneous regression of the benign forms of granular cell tumour has also been reported (Regezi and Scuibba, 2003).
In conclusion, a case of granular cell tumour on the dorsum of the tongue is reported in a 20-year-old female patient. Since it is such a rare lesion it is very easy to misdiagnose. The lesion occurred in the midline dorsum of the tongue whereas most granular cell tumours occur on the lateral aspect. The location of this lesion on the dorsum of the tongue necessitated further investigations to establish that the lesion was not thyroid tissue. This is because excising such a lump might render the patient hypothyroid if it happens to be the only thyroid tissue in the body.
References
- Abrikossoff A. Uber myome ausgehend von der quergestreiften wilkurlicken muskulatur. Virchows Arch. (Pathol. Anat.) 1926;260:215–233. [Google Scholar]
- Apisarnathanarax P. Granular cell tumour. J. Am. Acad. Dermatol. 1981;5:171–182. doi: 10.1016/s0190-9622(81)70085-9. [DOI] [PubMed] [Google Scholar]
- Azzopardi J.G. Histogenesis of the granular cell myoblastomas. J. Pathol. Bacteriol. 1956;71:85–94. doi: 10.1002/path.1700710113. [DOI] [PubMed] [Google Scholar]
- Becelli R., Perugini M., Gasparini G., Cassoni A., Fabiani F. Abrikossoff’s tumour. J. Craniofac. Surg. 2001;12:78–81. doi: 10.1097/00001665-200101000-00013. [DOI] [PubMed] [Google Scholar]
- Billeret-Lebranchu V. Granular cell tumor: epidemiology of 263 cases. Arch. Anat. Cytol. Pathol. 1999;47:26–30. [PubMed] [Google Scholar]
- Collins B.M., Jones A.C. Multiple granular cell tumours of the oral cavity. Report of a case and review of the literature. J. Oral Maxillofac. Surg. 1995;53:707–711. doi: 10.1016/0278-2391(95)90178-7. [DOI] [PubMed] [Google Scholar]
- Eguia A., Uribarri A., Gay-Escoda C., Crovetto M.A., Martinez-Conde R., Aguirre J.M. Granular cell tumour: report of 8 intraoral cases. Med. Oral Pathol. Oral Cir. Bucal. 2006;11:E425–E428. [PubMed] [Google Scholar]
- Guilliani M., Lajolo C., Pagnoni M., Boari A., Zannonni G.F. Granular cell tumor of the tongue (Abrikossoff’s tumour). A case report and review of the literature. Minerva Stomatol. 2004;53:465–469. [PubMed] [Google Scholar]
- Lack E.E., Worsham G.F., Calihan M.D., Crawford B.E., Klappenbach S., Rowden G., Chun B. Granular cell tumour: a clinicopathological study of 110 patients. J. Surg. Oncol. 1980;13:301–316. doi: 10.1002/jso.2930130405. [DOI] [PubMed] [Google Scholar]
- Lamey P.S., Rennie J.S., James J. Multiple granular cell tumours of the palate. Int. J. Oral Maxillofac. Surg. 1987;16:236–238. doi: 10.1016/s0901-5027(87)80138-8. [DOI] [PubMed] [Google Scholar]
- Nagaraj P.B., Ongole R., Bhujanga-Rao B.R. Granular cell tumor of the tongue in a 6-year-old girl. A case report. Med. Oral Pathol. Oral Cir. Bucal. 2006;11:E162–E164. [PubMed] [Google Scholar]
- Naief N.S., Brandwein M., Lawson W., Lumerman G.R. Synchronous lingual granular cell tumour and squamous cell carcinoma. A case report and review of the literature. Arch. Otolaryngol. Head Neck Surg. 1997;123:543–547. doi: 10.1001/archotol.1997.01900050099013. [DOI] [PubMed] [Google Scholar]
- Nishida M., Inoue M., Yanai A., Matsumoto T. Malignant granular cell tumour in the masseter muscle: case report. J. Oral. Maxillofac. Surg. 2000;58:345–348. doi: 10.1016/s0278-2391(00)90070-3. [DOI] [PubMed] [Google Scholar]
- Noonan J.D., Horton C.E., Old W.L., Stokes T.L. Granular cell myoblastoma of the head and neck. Review of the literature and 10-year experience. Am. J. Surg. 1979;138:611–614. doi: 10.1016/0002-9610(79)90430-6. [DOI] [PubMed] [Google Scholar]
- Pressor R., Chung E.B. Granular cell tumour in black patients. J. Natl. Med. Assoc. 1980;72:1171–1175. [PMC free article] [PubMed] [Google Scholar]
- Regezi J.A., Bastakis J.G., Courtney R.M. Granular cell tumour of the head and neck. J. Oral. Surg. 1979;37:402–406. [PubMed] [Google Scholar]
- Regezi J.A., Scuibba J. fourth ed. Saunders; Philadelphia, PA: 2003. Oral Pathology: Clinical-pathologic Correlations. pp. 171–173. [Google Scholar]
- Rifkin R.H., Blocker S.H., Palmer J.O., Temberg J.L. Multiple granular cell tumours: a familial occurrence in children. Arch. Surg. 1986;121:945–947. doi: 10.1001/archsurg.1986.01400080091017. [DOI] [PubMed] [Google Scholar]
- Rubinstein D., Shanker D.B., Finlayson L., Boxalt L., Krafchik B. Multiple cutaneous granular cell tumours in children. Paediatr. Dermatol. 1987;4:94–97. doi: 10.1111/j.1525-1470.1987.tb00759.x. [DOI] [PubMed] [Google Scholar]
- Sposto M.R., Navarro C.M., de Andrade C.R. Granular cell tumour (Abrikossof tumour): case report. Oral. Oncol. Extra. 2006;42:194–197. [Google Scholar]
- Van Der Wal N., Baak J.P.A., Schipper N.W., Van Der Waal I. Pseudoepitheliomatous hyperplasia in granular cell tumour of the tongue. J. Oral. Pathol. Med. 1989;18:8–10. doi: 10.1111/j.1600-0714.1989.tb00723.x. [DOI] [PubMed] [Google Scholar]
- Zangari F., Trombelli L., Calura G. Granular cell myoblastoma: review of the literature and report of a case. Minerva Stomatol. 1996;45:231–237. [PubMed] [Google Scholar]


