Abstract
Herpes simplex encephalitis (HSE) still remains a serious illness with high morbidity and mortality. The characteristic presentation of HSE usually consists of fever, headache, and altered mental function. We present three patients with atypical features of HSE. First, a 48-year-old man with symptomatic posttraumatic epilepsy, who developed a gastrointestinal infection, seizures, and fever. After significant clinical improvement, the patient had fever again and developed a status epilepticus, which led to the diagnosis of HSE. Second, an 84-year-old woman with hyperactive delirium after levofloxacin intake. Cranial computed tomography (CCT) revealed hypodense temporal changes, prompting lumbar puncture and diagnosis of HSE. Third, a 51-year-old diabetic woman presented with fever and acute confusion. As CCT and cell count of cerebrospinal fluid (CSF) were normal, infection and hyperglycemia as initial diagnoses were postulated. Due to aphasic symptoms, the differential diagnosis of a stroke was taken into account. Thus a second lumbar puncture led to the correct diagnosis of HSE. These atypical presentations need a high grade of suspicion and a high willingness to reconsider the initial working diagnosis, in order to prevent a diagnostic delay.
Keywords: Acyclovir, atypical course of disease, cerebrospinal fluid, consciousness disturbance, herpes simplex encephalitis, herpes simplex virus
Introduction
Viral encephalitis is a life-threatening condition. The prognosis mainly depends on the viral pathogenicity, the host immune status, and the availability of virostatic therapy.[1,2] Herpes simplex virus Type I (HSV-1) is the most commonly recognized virus of such an acute, sporadic encephalitis worldwide.[3] The lethality without virostatic therapy was about 70% and could be lowered to 14-20% with the aid of a treatment regimen like acyclovir[3,4] Signs and symptoms of this rapidly progressive disease include headache for a few days, followed by acute confusion, focal deficits, seizures or hemiparesis, hallucinations, and altered levels of consciousness.[2] However, atypical course of disease can occur making diagnosis difficult and delayed.[2,3] Our intention by presenting three cases is to alert for atypical manifestations of herpes simplex encephalitis (HSE). We recommend a high index of suspicion, and repeated clinical and laboratory test when facing an encephalitic syndrome.
Case Reports
Case 1
A 48-year-old man with known symptomatic epilepsy reported diarrhea and fever for some days. This was followed by a series of focally beginning secondary generalized seizures. Thus the emergency physician administered 7.5 mg midazolam intravenously and admitted the patient to the neurological department. On admission, the patient was sedated and presented residual aphasia. A meningeal irritation was not noted. The neurological signs and symptoms were interpreted as postictal. There were no visible injuries, therefore a series of seizures due to afebrile infection was presumed. The patient was observed under intermediate care aspects. The next 2 days the patient's condition improved, he was afebrile and no focal neurological deficits were present. The medication with levetiracetam was augmented to a dosage of 1500 mg/daily. Electroencephalography showed slightly slowed focal activity on the left temporal side on the background of normal alpha wave activity. The day before the planned discharge from inpatient care, the patient suffered with sudden onset of a series of epileptic seizures progressing to a convulsive status with high fever of 40°C. Oral intubation and mechanical ventilation became necessary in order to treat status epilepticus. As anticonvulsive agents phenytoin, levetiracetam, midazolam, and propofol were applied, the Cranial computed tomography (CCT) scan at this time revealed hyodensities in the right temporal lobe and the right insular cortex [Figure 1a]. The left sided hypodensity is related to a former head injury. The following cerebrospinal fluid (CSF) analysis showed elevated lymphocytic cell count (27/μL; normal < 4) with normal glucose but elevated protein (699 mg/dl (normal < 450)), indicating an inflammatory CSF syndrome. Polymerase chain reaction (PCR) assay for HSV-1 was tested positive. A treatment regimen was implemented with acyclovir (10 mg/kg body weight) three times daily for 21 days. After 4 days of ventilation the patient could be extubated and improved clinically successful. Cranial magnetic resonance imaging (MRI) on day 10 showed extended encephalitic changes in the right frontal and temporal lobe [Figure 1b]. After a rehabilitation program, follow-ups took place as an outpatient. Yet due to neuropsychological impairments he cannot work in his profession as a carpenter anymore. Under the current antiepileptic therapy (levetiracetam 1500 mg daily), the patient is seizure-free.
Figure 1.
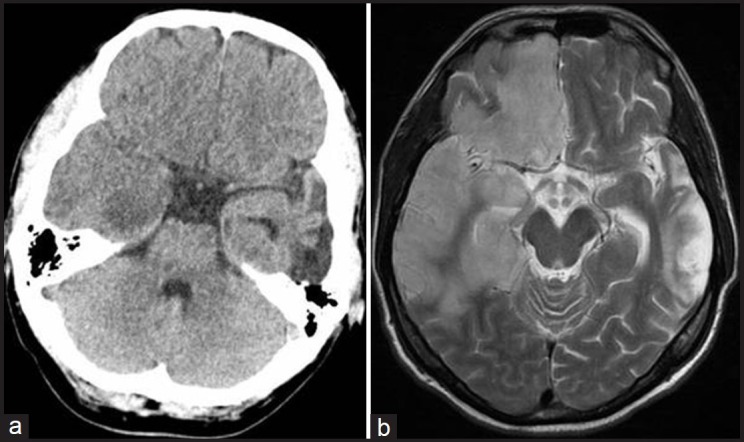
48-year-old man at time of convulsive state and temperature of 40°C. (a) Unenhanced axial CT scan shows right mesiotemporal hypodensity and swelling. (b) 10 days later, axial T2-weighted MR image shows increased signal intensity in the right temporal and frontal lobe
Case 2
An 84-year-old woman was found on the floor with altered mental status and myoclonic jerks. Some days earlier, levofloxacin was prescribed by her physician due to cystitis. On admission, the patient was somnolent and disorientated, but without meningeal irritation. On both arms, myoclonic jerks could be observed. The working diagnosis in the emergency room was quinolone associated delirium. In order to exclude other etiologies, a CCT was performed, revealing a hypodense lesion in the right temporal lobe [Figure 2a]. The following CSF analysis showed elevated lymphocytic cell count (36/μL; normal < 4) and protein (961 mg/dl (normal < 450)); lactate and glucose were normal [Figure 2b]. A therapy with acyclovir (10 mg/kg every 8 h for 14 days) was initiated. PCR assay for HSV-1 was found to be positive. Gradually the patient recovered and took part in a rehabilitation program. A year later, the patient was admitted due to a symptomatic seizure. At this time, she still showed marked neurocognitive impairment, needing moderate home care.
Figure 2.
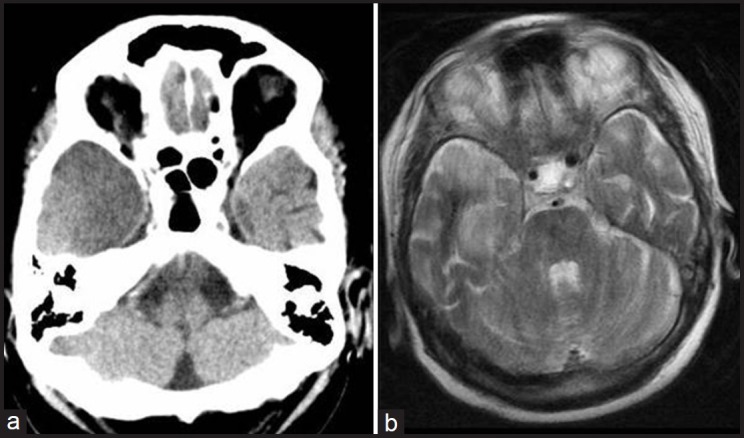
85-year-old woman with delirium and myoclonic jerks. (a) Unenhanced axial CT scan shows hypodensity of the right temporal lobe. (b) 4 days later axial T2-weighted MR image shows increased signal intensity in the right temporal lobe and additional movement artefacts
Case 3
A 51-year-old diabetic woman was admitted to hospital with fever and acute confusion. In the emergency department, no signs of meningeal irritation and focal neurological signs were detected. A CCT was unremarkable [Figure 3] and lumbar puncture showed 1 cell/μL (normal < 4) and slightly elevated protein 646 mg/dl (normal < 450) with normal glucose. As blood glucose was high (351 mg/dl), an infection triggered diabetic disorder was suspected. Therefore the patient was treated by the internist. The following day the patient suffered from aphasia. Since aphasia persisted, a stroke of the left temporal lobe was assumed next. However, as fever continued and confusional symptoms predominated, a second lumbar puncture was performed. The result, this time, showed elevated cell count (31 cells/μL, normal < 4) and elevated protein 1157 mg/dl (normal < 450). HSV was tested positive in the first and second CSF sample by PCR. Despite virostatic therapy with intravenous acyclovir (10 mg/kg every 8 h for 21 days), the patient's condition deteriorated, making mechanic ventilation and intensive care necessary. Furthermore neuroradiologically severe left-hemispheric encephalitic changes could be observed [Figure 3c]. After a prolonged rehabilitation program, the patient is at home, but needs professional care.
Figure 3.
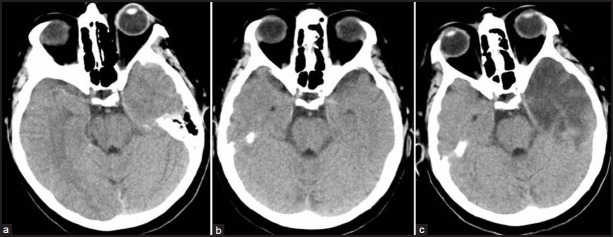
51-year-old diabetic woman with fever and confusion. (a) Unenhanced axial CT scan shows no significant changes in the left temporal lobe. (b) 2 days later unenhanced axial CT scan is still unremarkable. (c) 14 days later, unenhanced axial CT scan shows marked hypodensity in the left temporal lobe
Discussion
The characteristic clinical presentation of a viral encephalitis usually consists of fever, headache, clouding of consciousness, seizures, and often focal neurological deficits such as hemiparesis, ataxia, or dysphasia.[2,5,6] Besides HSV-1 and -2, other causative viruses come into question. Particularly depending on the geographical context, there are herpes viruses, adenoviruses, arboviruses, and numerous other viruses.[5] The diagnosis of viral encephalitis is challenging. A number of differential diagnoses had to be considered, such as vascular, metabolic, and other noninfective encephalopathies.[2,5,6]
In all the three patients, it was difficult to make the diagnosis of viral encephalitis. In the first patient with known symptomatic posttraumatic epilepsy, who reported diarrhea, initially, fever was missing. Since admission, he had been improved clinically, hence the working diagnosis was a series of seizures, triggered by a gastrointestinal infection. Not before the acute onset of high fever and an epileptic status, a concurrent etiology, in particular encephalitis was considered. This prompted imaging and CSF analysis and appropriate treatment. In the second patient, the working diagnosis was a delirium in the elderly due to the intake of quinolone.[7] Primarily encephalitis was not considered. CCT on admission showed a temporal, for a vascular event, atypical lesion. Hence, the suspicion was drawn to HSE, which was finally proved by CSF analysis. In the third patient, normal focal neurological status, normal CCT, normal cell count in CSF, and missing neck stiffness made an encephalitic cause of the signs and symptoms at the time of admission improbable. Initially a disorder associated with known long lasting diabetes was assumed, as current glucose level was elevated. The following aphasic symptoms led secondly to the suspicion of a stroke. However, as clinical signs and symptoms progressed, a second CSF analysis was conducted, leading to correct diagnosis.
From our patients we learn three lessons. First, HSE does not always have an abrupt onset with rapid progression, but can show a biphasic course of disease with a period of clinical improvement after a first phase of illness.[6] Additionally, in a patient with known epilepsy, a concurrent etiology, such as HSE in patient 1, has to be considered as the trigger of an epileptic status. Additionally, the fact that the nondominant lobe of the brain had been affected, might had been initially masking the signs of encephalitis.[8]
Second, in a delirium in an elderly with cognitive impairment, HSE should be included as a potential differential diagnosis. Despite HSE having a bimodal age distribution (patients below 20 years of age or above 50 with the peak between 60 and 64 years), only few data have been reported about HSE in older adults.[9,10] In a series of 12 elderly HSE patients, outcome was poor and mortality was high than in patients with HSE in general.[10] Major symptoms observed in this series had been behavioral changes and disorientation as in patient 2. These symptoms are common in various disorders in older patients and can easily be misdiagnosed. Thus if HSE is considered early imaging, preferably a MRI, due to its higher sensitivity in the evaluation of patients with encephalitis,[5] CSF studies should be performed.
Third, regarding HSE, early CSF analysis can show a normal cell count as in patient 3. Such a constellation has been reported lately in patients with a recent history of whole-brain-irritation, suggesting an anergic course of HSE.[11] Furthermore, it could be demonstrated in 2-3% of patients with HSE that a positive PCR of CSF for HSV could be confirmed, but no other pathological CSF parameters. Even these patients were all immunocompromised, as most other single patients reported earlier.[4,11,12,13,14,15,16,17] In all patient despite normal CSF cell count, test on HSV-1 by PCR assay was positive as reported by Jakob, et al.,[11] However, even PCR assay can be negative, leading to premature termination of antiviral treatment.[16]
In conclusion, diagnosis of HSE is challenging, needing a high grade of suspicion and a high willingness to reconsider the initial working diagnosis. CSF analysis and brain imaging are mandatory for identifying CNS symptoms. Moreover, as a first line of treatment, acyclovir is to be considered early, even before any proven diagnosis.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Steiner I, Budka H, Chaudhuri A, Koskiniemi M, Sainio K, Salonen O, et al. Viral encephalitis: A review of diagnostic methods and guidelines for management. Eur J Neurol. 2005;12:331–43. doi: 10.1111/j.1468-1331.2005.01126.x. [DOI] [PubMed] [Google Scholar]
- 2.Whitley RJ. Herpes simplex encephalitis: Adolescents and adults. Antiviral Res. 2006;71:141–8. doi: 10.1016/j.antiviral.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 3.Stahl JP, Mailles A, De Broucker T. Herpes simplex encephalitis and management of acyclovir in encephalitis patients in France. Epidemiol Infect. 2012;140:372–81. doi: 10.1017/S0950268811000483. [DOI] [PubMed] [Google Scholar]
- 4.Fodor PA, Levin MJ, Weinberg A, Sandberg E, Sylman J, Tyler KL. Atypical herpes simplex virus encephalitis diagnosed by PCR amplification of viral DNA from CSF. Neurology. 1998;51:554–9. doi: 10.1212/wnl.51.2.554. [DOI] [PubMed] [Google Scholar]
- 5.Tunkel AR, Glaser CA, Bloch KC, Sejvar JJ, Marra CM, Roos KL, et al. The management of encephalitis: Clinical practice guidelines by the Infectious Diseases Society of America. Clin Infect Dis. 2008;47:303–27. doi: 10.1086/589747. [DOI] [PubMed] [Google Scholar]
- 6.Kennedy PG. Viral encephalitis: Causes, differential diagnosis, and management. J Neurol Neurosurg Psychiatry. 2004;75:i10–5. doi: 10.1136/jnnp.2003.034280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tomé AM, Filipe A. Quinolones: Review of psychiatric and neurological adverse reactions. Drug Saf. 2011;34:465–88. doi: 10.2165/11587280-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 8.Asnis D, Niazi N. Non-dominant hemisphere encephalitis in patient with signs of viral meningitis, New York, USA. Emerg Infect Dis. 2009;15:1320–1. doi: 10.3201/eid1508.090466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Steiner I. Herpes simplex virus encephalitis: New infection or reactivation? Curr Opin Neurol. 2011;24:268–74. doi: 10.1097/WCO.0b013e328346be6f. [DOI] [PubMed] [Google Scholar]
- 10.Riera-Mestre A, Requena A, Martínez-Yelamos S, Cabellos C, Fernández-Viladrich P. Herpes simplex encephalitis in older adults. J Am Geriatr Soc. 2010;58:201–2. doi: 10.1111/j.1532-5415.2009.02655.x. [DOI] [PubMed] [Google Scholar]
- 11.Jakob NJ, Lenhard T, Schnitzler P, Rohde S, Ringleb PA, Steiner T, et al. Herpes simplex virus encephalitis despite normal cell count in the cerebrospinal fluid. Crit Care Med. 2012;40:1304–8. doi: 10.1097/CCM.0b013e3182374a34. [DOI] [PubMed] [Google Scholar]
- 12.Auyeung P, Dunn A. Atypical case of Herpes simplex encephalitis. Int Med J. 2008;38:294–5. doi: 10.1111/j.1445-5994.2008.01645.x. [DOI] [PubMed] [Google Scholar]
- 13.Santos E, Moralejo L, de Dios S, Fuertes A. Herpes simplex encephalitis with a normal cerebrospinal fluid. Med Clin (Barc) 2004;122:357–8. doi: 10.1016/s0025-7753(04)74238-4. [DOI] [PubMed] [Google Scholar]
- 14.Razavi B, Razavi M. Herpes simplex encephalitis-an atypical case. Infection. 2001;29:357–8. doi: 10.1007/s15010-001-1124-8. [DOI] [PubMed] [Google Scholar]
- 15.Hariri OR, Prakash L, Amin J, Minasian T, Qazi FM, Holt C. Atypical presentation of herpes simplex encephalitis in an infant. J Am Osteopath Assoc. 2010;110:615–7. [PubMed] [Google Scholar]
- 16.Adler AC, Kadimi S, Apaloo C, Marcu C. Herpes simplex encephalitis with two false-negative cerebrospinal fluid PCR tests and review of negative PCR results in the clinical setting. Case Rep Neurol. 2011;3:172–8. doi: 10.1159/000330298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shalchi Z, Bennett A, Hargroves D, Nash J. Diagnostic delay in a case of herpes simplex encephalitis.BMJ Case Rep 2009;2009:pii: bcr12. 8 doi: 10.1136/bcr.12.2008.1350. Diagnostic delay in a case of herpes simplex encephalitis BMJ Case Rep 2009;2009:pii: bcr1220081350. [DOI] [PMC free article] [PubMed] [Google Scholar]


