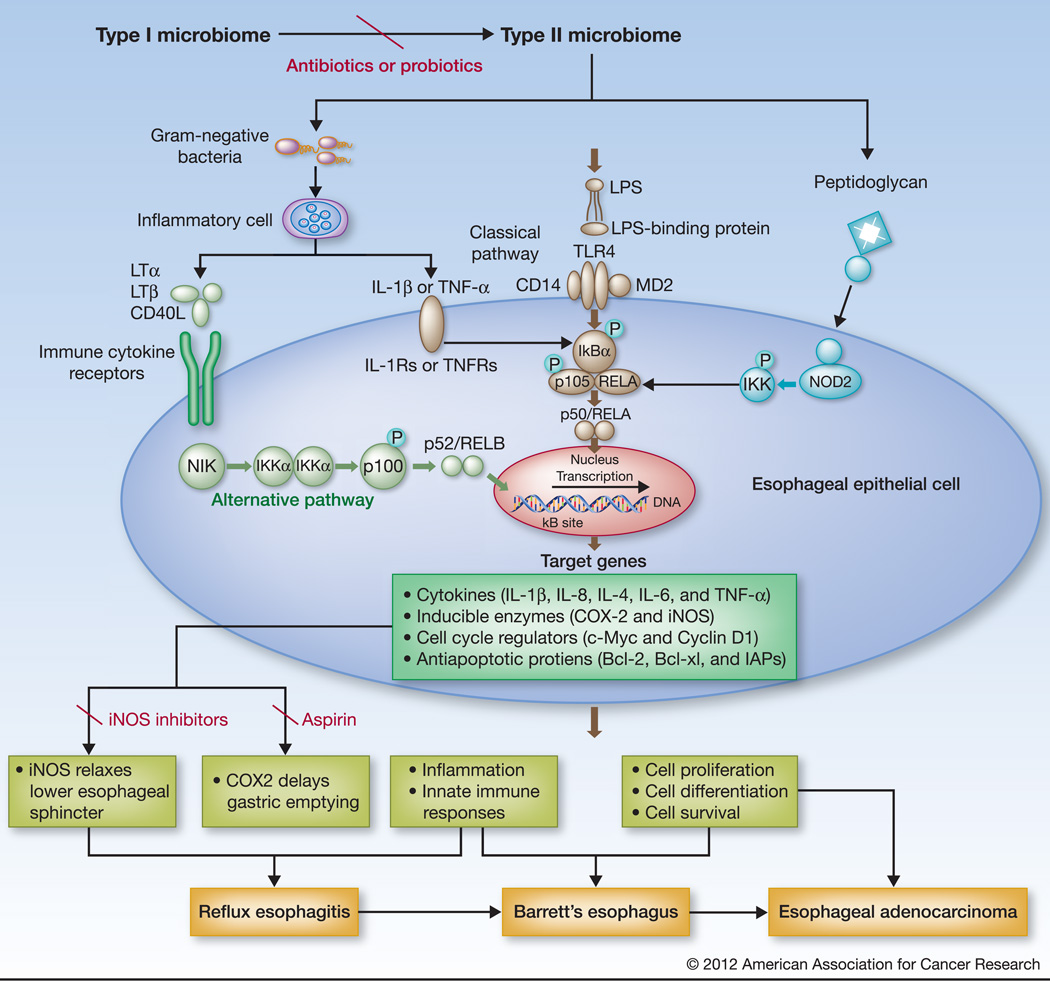
Figure 1.
Hypothetical activation of NF-kB pathway by type II microbiome in the esophagus. The type I microbiome, more closely associated with normal esophagus, is dominated by Gram-positive bacteria, while the type II microbiome, mainly associated with abnormal esophagus, including reflux esophagitis and Barrett's esophagus, contains a larger proportion of Gram-negative bacteria. The increased Gram-negative bacterial components, such as LPS might thus directly stimulate TLRs (mainly TLR4) leading to activation of the classical NF-kB pathway (p50/RELA; middle); LPS might also stimulate inflammatory cells, like macrophages, to release cytokines that bind to cytokine receptors on esophageal epithelial cells to trigger the alternative NF-B pathway (p52/RelB; left). Moreover, Peptidoglycan from Gram-negative bacteria might act on NOD-like receptors to activate the NF-kB pathway (right). NF-kB activation up-regulates the expression of its downstream genes encoding a variety of cytokines, inducible enzymes, and proteins that provoke inflammation, relaxes smooth muscles, and regulate cell proliferation and apoptosis. Known NF-kB regulated enzymes include iNOS that relaxes the lower esophageal sphincter and COX2 that delays gastric emptying. The end effects could be the induction of gastroesophageal reflux, metaplasia, and/or neoplasia. The effect could be prevented by reversion of the type II to type I microbiome using antibiotics or probiotics, NF-kB inhibitors, or selective inhibitors to iNOS or COX2 (Aspirin).