Figure 2.
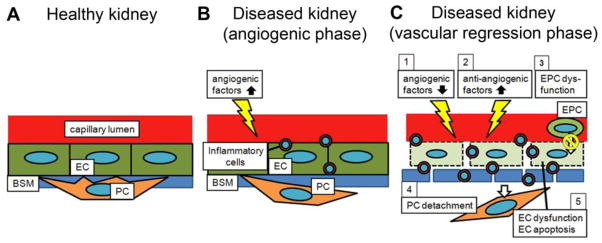
Schematic of mechanisms of peritubular capillary (PTC) rarefaction following kidney injury. (A) In the healthy kidney, pericytes (PC) are embedded into the capillary basement membrane (BSM) and attached to capillary endothelial cells (EC). This close relationship between PCs and ECs supports capillary integrity. (B) Subsequent to an initial insult, angiogenic factors (e.g. VEGF) are up-regulated and ECs are proliferative. PCs promptly start to migrate away from the capillary area. Simultaneously, inflammatory cells infiltrate into the interstitium. (C) In response to continuous insults, (1) angiogenic factors are down-regulated, (2) anti-angiogenic factors (e.g. thrombospondin-1) are up-regulated, (3) endothelial progenitor cells (EPCs) do not promote neoangiogenesis, (4) PC detachment from vasculature destabilizes ECs, and (5) EC dysfunction and EC apoptosis progress. All of these mechanisms contribute to an anti-angiogenic environment, resulting in PTC rarefaction. The capillary BSM is also degraded. Additionally, a large number of inflammatory cells migrate from the capillary lumen into the extracapillary space. Note that some of the angiogenic factors (e.g. angiopoietin-1) and anti-angiogenic factors (e.g. thrombospondin-1) induce infiltration of inflammatory cells, which impairs the angiogenic response.
