Abstract
Aim:
The evaluation of soy allergy in patients over 14 years of age suffering from atopic dermatitis. The evaluation of the correlation to the occurence of peanut and pollen allergy.
Materials and Methods:
Altogether 175 persons suffering from atopic dermatitis were included in the study: Specific IgE, skin prick tests, atopy patch tests to soy, history and food allergy to peanut and pollen allergy were evaluated.
Results:
The early allergic reaction to soy was recorded in 2.8% patients. Sensitization to soy was found in another 27.2% patients with no clinical manifestation after soy ingestion. The correlation between the positive results of examinations to soy and between the occurence of peanut and pollen allergy was confirmed in statistics.
Conclusion:
Almost one third of patients suffering from atopic dermatitis are sensitized to soy without clinical symptoms. The early allergic reaction to soy occur in minority of patients suffering from atopic dermatitis.
Keywords: Atopic dermatitis, pollen allergy, peanut allergy, soy allergy, specific IgE, skin prick tests
Introduction
What was known?
Food allergy to soy has been described to date primarily in young children with atopic dermatitis, most patients are likely to develop soy tolerance by late childhood. But epidemiologic data on soybean allergy in adults is virtually lacking.
Soy is introduced into the diet early in life, often in the form of infant formula in children with intolerance or allergy to cow's milk. Allergenicity of soybean proteins has been documented since the 1980s. Soybean exposure is widespread in Asia and the USA but its consumption has increased in Europe too during the past years, particularly in vegetarian cuisine and because of food technological benefits achieved by adding soy proteins to various processed food products. Soy is consumed as soy oil, soy flour, soy milk, soy drinks, soy flakes. As it is a good and cheap protein source, it may be part of a wide variety of processed foods such as meat products, sausages, bakery goods, chocolate or breakfast cereals. Therefore, undeclared traces of soy may represent a hidden allergen in compound food products. In this context, knowledge on the minimum doses of soy capable of inducing an allergic reaction is highly important.
Food allergy to soy has been described to date primarily in young children with atopic dermatitis[1,2,3] affecting approximately 0.4% of children.[4] Most patients with soy allergy are likely to develop soy tolerance by late childhood.[4] Moreover, epidemiologic data on soybean allergy in adults is virtually lacking.[5,6] Just a few papers on clinical aspects of soy allergy have been published within the recent years.
In Central Europe soy is a clinically relevant birch pollen-related allergenic food. Crossreaction is mediated by a Bet v 1 homologous protein, Gly m 4. Additionally, birch pollen allergic patients might acquire through Bet v 1 sensitization allergies to mungbean or peanut, in which Vig r 1 and Ara h 8 are the main cross-reactive allergens.[7] This suggests that there are two soy allergy phenotypes, with the late-onset variety possible related to either birch pollen cross-reactivity or persistent peanut allergy.[7]
The aim of our study is the evaluation of the occurence of allergic reaction to soy according the history and evaluation of the results of examinations to soy allergy in patients over 14 yrs of age suffering from atopic dermatitis (the evaluation of the results of specific IgE, skin prick tests, atopy patch test). Our other aim is the evaluation, if the occurence of pollen and peanut allergy is in the correlation with the occurence of positive results of specific IgE (sIgE), skin prick tests (SPT) and atopy patch tests (APT) to soy in this group of patients.
Materials and Methods
Patients over 14 yrs of age with atopic dermatitis examined at Department of Dermatology and Venereology, University Hospital and Medical Faculty of Charles University, Hradec Králové, Czech republic from January 2005 to June 2009 were included in the study.
The diagnostic work - up of food allergy to soy (SPT, APT, sIgE) in intervals with milder symptoms of atopic dermatitis (evaluated with SCORAD) was performed.
All included patients signed the informed consent with the study and agreement of local Ethics comitee was given to this study.
Examinations
Complete dermatological and allergological examination was performed in all included patients. The occurrence of asthma bronchiale (AB) was recorded with spirometry examination at allergological outpatient department.
The evaluation of pollen allergy
The occurence of pollen allergy was determined according the history about the pollen allergy and according the specific IgE level and the SPT results for pollen (containing Bet v 1 and Bet v 2 allergens and for pollen containing homologous allergens).
Commercial extracts Alyostal (Stallergens, France) was used for SPT. The serum level of the sIgE has been measured with the method of CAP (system FEIA - Pharmacia Diagnostics, Uppsala, Sweden). The level of specific IgE higher than 0.35 U/ml was assessed as positive. Allergy to pollen was defined as having a clear history of allergic reaction to pollen with the positive results in SPT or specific IgE to pollen containing Bet v 1 and Bet v 2 allergens.
Scoring of atopic dermatitis
The diagnosis of atopic dermatitis was made with the Hanifin-Rajka criteria[8] at the outpatient department of Dermatology and Venereology, university hospital and medical faculty of charles university, Hradec Králové, Czech republic.
Severity of eczema was scored in agreement with SCORAD score: As a mild form to 20 points, as moderate over 20 to 50 points, as a severe form over 50 points.
Personal history
The detailed personal history of possible food allergy was taken in all included patients.
The patients answered if they suffered from immediate or late food adverse reactions affecting the skin, gastrointestinal tract, or respiratory tract not only after the ingestion of soy, but also after ingestion of other foods.
After the discontinuation of antihistamines and topical steroids for at least five days and systemic steroid therapy and phototherapy at least two months, the SPT and the APT were performed. The serum level of the sIgE to soy has been examined. The patient was allowed to treat himself with a low potency topical corticosteroid. No other anti-inflammatory substances nor UV-therapy were applied.
Skin prick test
Commercial food extracts Alyostal (Stallergens, France) with soy was used for skin prick tests.
SPTs were placed on the volar side of the forearm according to the extent of atopic dermatitis. SPTs were carried out by a standardized method using lancets with a 1 mm tip. The results were read after 15 mins and were assessed by comparison with the wheal induced by histamine (10 mg/ml) and negative control. A wheal with a diameter greater than 3 mm in comparison with a negative control was scored as positive.
Specific IgE
The serum level of the sIgE to soy has been measured with the method of CAP (system FEIA - Pharmacia Diagnostics, Uppsala, Sweden). The level of specific IgE higher than 0.35 U/ml was assessed as positive.
Atopy patch tests
Atopy patch tests were performed on non-lesional, non-abraded, untreated skin of the back during a remission.
The technique similar to conventional patch tests has been used in performing of atopy patch testing - CURATEST F strip (Lohmann and, Rauscher International GmbH and Co.KG D-56579, Rengsdorf, Germany) with 12 mm cup size. Atopy patch tests were performed with soy flour. Soy powder was dissolved in distillated water (1g/10 ml) The occlusion time of atopy patch tests was 48 hours, the first results were evaluated 30 min after removal of the tests and the second results were analysed 72 hrs after the application of the tests. Grading of positive APTs reactions was similar to the criteria used in conventional contact allergy patch testing with the modifications of the European task force on atopic dermatitis consensus meetings.[9] Only reactions from erythema, infiltration onwards were designated positive.
The evaluation of peanut allergy
Allergy to peanut was def ined as having a clear history of allergic reaction after peanuts ingestion in patients with the positive results in SPT or/in sIgE to peanuts. The serum level of the sIgE to peanuts has been measured with the method of CAP (system FEIA - Pharmacia diagnostics, Uppsala, Sweden), sIgE level to peanut more than 0,35 U/ml was assessed as positive. Commercial food extracts Alyostal (Stallergens, France) with peanuts was used for skin prick tests. A wheal with a diameter greater than 3 mm in comparison with a negative control was scored as positive.
The patients included in the study were divided according the history about reaction after soy ingestion and according the results of examinations to soy (sIgE, APT, SPT) into four groups.
Patients with the clear clinical symtoms after soy ingestion and with the positive result at least at one of the diagnostic method (sIgE and/or APT and/or SPT to soy).
Patients without clinical symptoms after soy ingestion, but with the positive results to soy in two or more diagnostic methods.
Patients without clinical symptoms after soy ingestion, but with the positive results to soy only in one from diagnostic method.
Patients without clinical symptoms after soy ingestion and without the positive results to soy in performed examinations.
The occurence of pollen and peanut allergy and the occurence of asthma bronchiale was evaluated in above mentioned groups of patients.[1,2,3,4]
Results
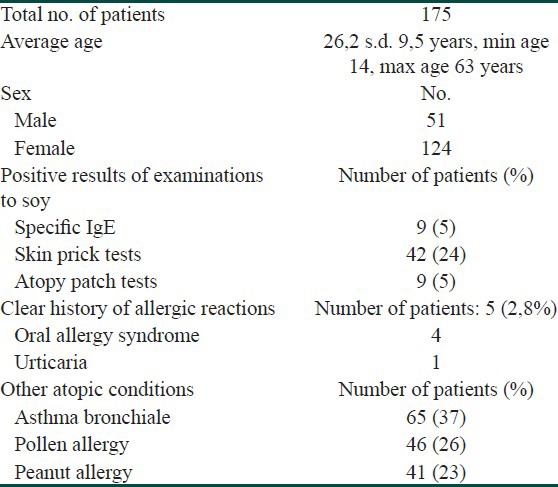
Altogether 175 persons suffering from atopic dermatitis were included in the study: 51 men, 124 women entered the study with the average age of 26.2 (s.d. 9.5 yrs), min. 14 max. 63 yrs; with the median SCORAD 31.6 points, s.d. 13.3 (max. 79.5 points, min. 12.5 points) at the beginning of the study. The patients characteristics are demonstrated in Table 1.
Table 1.
Patient older 14 yrs of age suffering from atopic dermatitis-characteristics
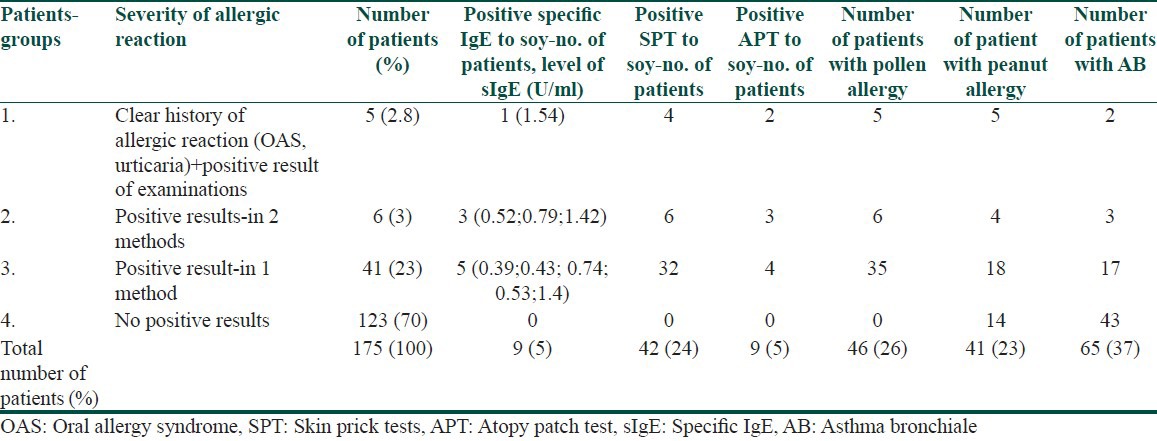
175 patients were divided into four groups according the results of examinations and according the history. This dividing is demonstrated in Table 2.
Table 2.
Patients divided into four groups according their history about soy allergy and according the results of examinations (specific IgE, SPT, APT)
-
Patients with the clear clinical symtoms after soy ingestion and with the positive result at least at one of the diagnostic method (sIgE, APT, SPT to soy)
-
5 patients – 2.8%Four of them described orall allergic syndrome after ingestion of soy from childhood, urticaria within 1 hour after ingestion of soy products is described in other one patient. All these patients suffer from pollen allergy and from peanut allergy (orall alergy syndrome). Only in one patient is positive specific IgE to soy (the level is 1,54 U/ml), SPT is positive in four of them as moderate reaction. APT reactions were evaluated as erythema, infiltration and papules in two patients in this group (one suffer from oral allergy syndrome, another from urticaria).
-
-
Patients without without clinical symptoms after soy ingestion, but with the positive results to soy in more than one of diagnostic methods
-
6 patients – 3%They did not observe any clear reaction after soy ingestion. All of them suffer from pollen allergy, four of them suffer from peanut allergy with the symptoms of oral allergy syndrome. The positive results of examinations to soy were recorded in all of them in two of diagnostic methods (specific IgE and/or SPT and/or APT). The results of specific IgE to soy are demonstrated in Table 2.
-
-
Patients without clinical symptoms after soy ingestion, but with the positive result to soy only in one of diagnostic method
-
41 patients – 23%The positive result in SPT to soy was recorded in 32 of them, positive specific level of IgE to soy in five patients and positive results in APT in four patients were recorded. The pollen allergy is observed in 35 of them, allergy to peanut in 18 of them with the clinical symptoms of orall allergy syndrome. The results of specific IgE to soy are demonstrated in Table 2.
-
-
Patients without without clinical symptoms after soy ingestion and without the positive results to soy in performed examination in the diagnostic work – up of food allergy
-
123 patients – 70%Pollen allergy was not recorded in these patients, but 15 patients suffer from allergy to peanuts.
-
The level of specific IgE to soy was recorded from 0,39 to 1,42 U/ml in our study in patients without clinical symptoms after soy ingestion (altogether eight patients from 2 and 3 group).
The reactions in atopy patch test were evaluated as erythema and infiltration in patients without clinical symptoms after soy ingestion (altogether seven patients from 2 and 3 group).
The reactions in SPT to soy were mild or moderate in all patients without clinical symtoms (altogether 38 patients from 2 and 3 group).
The pollen allergy was recorded in 46 patients (26%) in our study.
The penaut allergy was observed in 41 patients (23%) in our study.
Statistics
The Fisher's exact test was used for the correlation between the dividing the patients into four groups and between the occurence of pollen allergy: P = 0,0000. The dependency between this dividing and the occurence of pollen alergy was confirmed.
The Fisher's exact test was used for the correlation between the dividing the patients into four groups and between the occurence of peanut allergy: P = 0,0000. The dependency between this dividing and the occurence of peanut allergy was confirmed.
Discussion
Atopic dermatitis is a chronic intermittent inflammatory skin disease that may be in some cases associated with food allergies. Other numerous trigger factors for atopic dermatitis have been identified, including inhalable respiratory allergens, irritative substances and infectious microorganism such as Staphylococcus aureus. Psychogenic and climatic factors may also cause the exacerbation of atopic dermatitis.
The epidermal barrier plays a crucial role in protecting the body against infection and other exogenous insults through both minimizing trans-epidermal water loss and conferring immunological protection.[10] Filaggrin gene defects substantially increase the risk of atopic dermatitis. The increased skin permeability may increase the risk of sensitization to food and other allergens, this pointing to the possible role of cutaneous allergen avoidance in early life to prevent the onset of atopic dermatitis and food allergy.[10]
Despite the fact that soy is an important nutrient worldwide, just a few papers on clinical aspects of soy allergy have been published within the recent years. A large population with Ig-E mediated soy allergy and with a convincing history of an allergic reaction to soy was evaluated in the Savage's study. According this study, the great part of children with soy allergy will become tolerant over time, but this does not happen as early as previously thought, with only 69% outgrowing their allergy by age 10 yrs.[4] In this study, the most common presenting symptoms of soy allergy were gastrointestinal (vomiting, diarrhea, bloody stool and amdominal pain) in 41%, skin related (urticaria, angioedema and noneczematous rash) in 28%, eczema in 11%, lower respiratory tract (wheezing, coughing, and difficulty breathing) in 5% and upper respiratory tract (rhinitis and nasal congestion) in 4%. There was found a strong correlation between soy IgE and peanut IgE levels in this study.[4]
Recently, a retrospective review by Komata et al.,[11] suggested that soy-specific IgE levels of between 20 and 30 kU/L predicted a 50% chance of passing soy challenge.
Despite the considerable amount of IgE reactive soy proteins described so far, just a few allergens have been thoroughly characterized, and there is still a considerable lack of knowledge. To date, only the hydrophobic soybean hull protein Gly m 1, the soybean hull protein Gly m 2, soybean profilin Gly m 3 and the Bet v 1-homologous pathogenesis-related PR-10 protein Gly m 4 are officially accepted as soybean allergens according to the criteria of the international union of immunological societies allergen nomenclature sub-committee.[12,13,14,15] However, only the latter two allergens represent food allergens, whereas soy hull proteins have been described to be relevant in respiratory soy allergy acquired through inhalation of soy particles.
In our study, the positive results in diagnostic methods to soy are recorded in 30% of patients (52 patients from 175) suffering from atopic dermatitis, but the clinical symptoms with the early reaction are recorded only in five patients - 2.8%. Four of them suffered from oral allergy syndrome. Another one patient suffered from urticaria and early skin noneczematous reactions, these symptoms developed within one hour after the ingestion of soy or soy products in her history repeatedly. Other patients included in our study with positive results in examinations to soy (27-2%) did not observe any early nor late reaction after the common ingestion of soy, usually in a form of some concentrated soy products in home setting in their history. Six patients with the positive results in two diagnostic methods to soy suffer from pollen allergy and four of them suffer from oral allergy syndrome to peanut. The positive results in one diagnostic method were recorded in 41 patients (23%) – the majority of them had the positive results in skin prick tests, 18 from these patients suffer from allergy to peanut (with the clinical symptoms of oral allergy syndrome) and 35 patients suffer from pollen allergy. These patients did not observe any early nor late reactions after soy ingestion in their history. Nevertheless, all patients with positive results in skin prick tests to soy, who tolerated soy in their history, but suffered from allergy to peanuts and suffered as well from asthma bronchiale were instructed about possible reaction after soy ingestion. Our statististical evaluation showes, that there is the strong correlation between our division of patients into four groups according the results of their history and according the results of examinations with regard to the occurrence of pollen allergy and allergy to peanuts.
Soy has not been shown to be a common cause of severe/fatal reactions until a recent report of severe food-allergic reactions in Sweden collected by Foucard and Malmheden Yman.[16,17] The recent report of severe food-allergic reactions in Sweden has raised new concern over soy allergy in peanut-allergic individuals.[17] The authors concluded that soy allergy has probably been underestimated as a cause of food anaphylaxis, and that those at risk seem to be young people with asthma and peanut allergy so severe that they notice symptoms after indirect contact.
Oral allergy syndrome, which was observed in our study, is defined as the symptoms of IgE-mediated immediate allergy localized in the oral mucosa. Another term used for this syndrome is pollen-food allergy; the patient is sensitized with pollen via the airways and exhibits an allergic reaction to food antigen with a structural similarity to the pollen (class two food allergy).[18]
Recently, two publications have demonstrated that in Central Europe soy allergy is another clinically relevant birch pollen-related allergenic food.[12,15] Birch pollen-related food allergies are mainly mediated by crossreactions between the PR-10-protein Bet v 1 or the profilin Bet v 2 and homologous proteins in plant food.[19] While the majority of symptoms of pollen-food allergy are indeed mild, such as the oral allergy syndrome, caution is necessary, because systemic and severe reactions may be observed by some pollen-related food allergens (as Gly m 4 in soy). A follow-up study by Mittag[12] confirmed that Gly m 4 - specific IgE was positive in 21 of 22 birch pollinosis patients who developed soybean allergy, and that it inhibited the binding of IgE to soybean protein by 60% or more in 9 of 11 patients, indicating that Gly m 4 was the major allergen. Three patients with alder/birch pollinosis who developed oral allergy syndrome (1 case) or anaphylaxis (2 cases) after the intake of soymilk have been reported, and an involvement of Gly m 4 is suspected (20) in Japan, too.[20]
In our study, we did not record any patients with the worsening of atopic dermatitis after the ingestion of soy or soy products in their history repeatedly. Generally, in patients with suspected food allergy, which is thought to be aggravating eczema, it is important that any food avoidance measures suggested are based on a detailed history and supportive evidence from objective allergy tests. Key here is the role of skin prick testing and measure of specific IgE. Patch testing may have a role in those in whom delayed cell-mediated hypersensitivity reactions are thought to be implicated. In cases of diagnostic doubt, oral food challenge may be performed. In this provocation test, early clinical responses are those reactions observed within two hrs after the last administered dose, late - phase reactions are those occurring between 2 and 48 hrs. The food challenge test was not performed in our study, but the detailed history was taken from all patients included in this study and none skin reaction was observed after the ingestion of soy or soy products in their history. In the Savage's study, where the natural history of soy allergy is evaluated, the tolerance of soy is defined as tolerating concentrated soy at a food challenge or successful home introduction of concentrated soy products[4]; in our study the tolerance to soy was evaluated in the same way.
According to Sicherer[6] there are many unanswered questions in food allergy, and the issues of cross-reacting proteins and botanically related foods, and the significance of positive tests for IgE (prick skin test, RAST) are all at work in the dilemma of peanut and soy allergy. Most allergists would not stop an individual from ingesting a tolerated food on the basis of a positive prick skin test. It does not appear that there are enough data to recommend soy avoidance in soy-tolerant, peanut-allergic patients at this time. Further studies on the natural history of these allergies are needed.[6] But considering, that systemic and severe reactions may be observed by some pollen-related food allergens as Gly m 4, all patients with positive results in skin prick tests or specific IgE to soy, who tolerated soy, but suffered from allergy to peanuts and suffered as well from severe form of asthma bronchiale should be instructed about possible early reaction after soy ingestion.
Conclusion
The positive results to soy in specific IgE, SPT or APT can be observed in 30% of atopic dermatitis patients. But only a minority of these patients suffers from early allergic reaction after the soy ingestion (as oral allergy syndrome and urticaria). Majority of patients are sensitized to soy without clinical symptoms after the soy ingestion and they suffer from pollen or peanut allergy.
What is new?
The positive results to soy in specific IgE, skin prick test or atopy patch test can be observed in 30 % of atopic dermatitis patients. But only a minority of these patients suffers from early allergic reaction after the soy ingestion (as oral allergy syndrome and urticaria). Majority of patients are sensitized to soy without clinical symptoms after the soy ingestion, but they suffer from pollen or peanut allergy.
Footnotes
Source of Support: This work was supported by grant from Charles University in Prague, Czech republic
Conflict of Interest: Nil.
References
- 1.Sampson HA, Ho DG. Relationship between food-specific IgE concentrations and the risk of positive food challenges in children and adolescents. J Allergy Clin Immunol. 1997;100:444–51. doi: 10.1016/s0091-6749(97)70133-7. [DOI] [PubMed] [Google Scholar]
- 2.Niggemann B, Sielaff B, Beyer K, Binder C, Wahn U. Outcome of double-blind, placebo-controlled food challenge tests in 107 children with atopic dermatitis. Clin Exp Allergy. 1999;29:91–6. doi: 10.1046/j.1365-2222.1999.00454.x. [DOI] [PubMed] [Google Scholar]
- 3.Sicherer SH, Morrow EH, Sampson HA. Dose-response in double-blind, placebo-controlled oral food challenges in children with atopic dermatitis. J Allergy Clin Immunol. 2000;105:582–6. doi: 10.1067/mai.2000.104941. [DOI] [PubMed] [Google Scholar]
- 4.Savage J, Kaeding A, Matsui E, Wood R. The natural history of soy allergy. J Allergy Clin Immunol. 2010;126:683–6. doi: 10.1016/j.jaci.2009.12.994. [DOI] [PubMed] [Google Scholar]
- 5.Besler M, Helm R, Ogawa T. Allergen data collection-update: Soybean. ISFA. 2000;2(Suppl 3):1–35. [Google Scholar]
- 6.Sicherer S, Sampson H, Burks A. Peanut and soy allergy: A clinical and therapeutic dilemma. Allergy. 2000;55:515–21. doi: 10.1034/j.1398-9995.2000.00119.x. [DOI] [PubMed] [Google Scholar]
- 7.Ballmer W, Barbara K, Vieths S. Soy allergy in perspective. Curr Opin Allergy Clin Immunol. 2008;8:270–5. doi: 10.1097/ACI.0b013e3282ffb157. [DOI] [PubMed] [Google Scholar]
- 8.Hanifin J, Rajka G. Diagnostic features of atopic dermatitis. Acta Derm Venereol. 1980;(Suppl 92):44–7. [Google Scholar]
- 9.Darsow U, Laifaoui J, Kerschenlohr K, Wollenberg A, Przybilla B, Wüthrich B, et al. The prevalence of positive reactions in the atopy patch test with aeroallergen and food allergens in subjects with atopic dermatitis: A European multicenter study. Allergy. 2004;59:1318–25. doi: 10.1111/j.1398-9995.2004.00556.x. [DOI] [PubMed] [Google Scholar]
- 10.Worth A, Shaikh A. Food allergy and atopic eczema. Curr Opin Allergy Clin Immunol. 2010;10:226–30. doi: 10.1097/ACI.0b013e3283387fae. [DOI] [PubMed] [Google Scholar]
- 11.Komata T, Soderstrom L, Borres M, Tachimoto H, Ebisawa M. Usefulness of wheat and soybean specific IgE antibody titres for the diagnosis of food allergy. Allergol Int. 2009;58:599–603. doi: 10.2332/allergolint.09-OA-0096. [DOI] [PubMed] [Google Scholar]
- 12.Mittag D, Vieths S, Vogel L. Soybean allergy in patients allergic to birch pollen: Clinical investigation and molecular characterization of allergens. J Allergy Clin Immunol. 2004;113:148–54. doi: 10.1016/j.jaci.2003.09.030. [DOI] [PubMed] [Google Scholar]
- 13.Gonzalez R, Polo F, Zapatero L, Caravaca F, Carreira J. Purification and characterization of major inhalant allergens from soybean hulls. Clin Exp Allergy. 1992;22:748–55. doi: 10.1111/j.1365-2222.1992.tb02814.x. [DOI] [PubMed] [Google Scholar]
- 14.Rihs HP, Chen Z, Rueff F, Petersen A, Rozynek P, Heimann H, et al. IgE binding of the recombinant allergen soybean profilin (rGly m 3) is mediated by conformational epitopes. J Allergy Clin Immunol. 1999;104:1293–301. doi: 10.1016/s0091-6749(99)70027-8. [DOI] [PubMed] [Google Scholar]
- 15.Kleine-Tebbe J, Vogel L, Crowell DN, Haustein UF, Vieths S. Severe oral allergy syndrome and anaphylactic reactions caused by a Bet v 1 : Related PR-10 protein in soybean, SAM22. J Allergy Clin Immunol. 2002;110:797–804. doi: 10.1067/mai.2002.128946. [DOI] [PubMed] [Google Scholar]
- 16.Sampson H, Mendelson L, Rosen J. Fatal and near-fatal anaphylactic reactions to food in children and adolescents. N Engl J Med. 1992;327:380–4. doi: 10.1056/NEJM199208063270603. [DOI] [PubMed] [Google Scholar]
- 17.Foucard T, Malmheden Yman I. A study on severe food reactions in Sweden: Is soy protein an underestimated cause of food anaphylaxis? Allergy. 1999;54:261–5. doi: 10.1034/j.1398-9995.1999.00924.x. [DOI] [PubMed] [Google Scholar]
- 18.Breiteneder H, Ebner C. Molecular and biochemical classification of plant-derived food allergens. J Allergy Clin Immunol. 2000;106:27–36. doi: 10.1067/mai.2000.106929. [DOI] [PubMed] [Google Scholar]
- 19.Vieths S, Scheurer S, Ballmer-Weber B. Current anderstanding of cross-reactivity of food allergens and pollen. Ann N Y Acad Sci. 2002;964:47–68. doi: 10.1111/j.1749-6632.2002.tb04132.x. [DOI] [PubMed] [Google Scholar]
- 20.Harada S, Nakamura A, Matsunaga A. Three cases of soy milk allergy. J Environ Dermatol Cutan Allergol. 2007;1:31–8. [Google Scholar]


