Abstract
Introduction
Measles is an acute, highly communicable viral disease, with measles outbreaks usually occurring in settings where there are unvaccinated populations. After being notified of a cluster of five measles cases in a Singapore public hospital in August 2011, the Ministry of Health Singapore conducted an outbreak investigation.
Methods
Active case detection was conducted, and all notified cases’ movement history within the hospital were reviewed to determine any common exposures in place and time. Cases were classified as nosocomial if they had contact with other measles cases in the hospital seven to 21 days before onset dates. Laboratory testing included serological and molecular diagnostic methods.
Results
Of the 14 cases, seven cases were nosocomial cases. Investigations identified two wards where cases were epidemiologically linked. Two cases in Ward A were of D8 genotype and genotypically 100% identical, thus confirming a common source of infection. The six cases in Ward B (including one transferred from Ward A) had overlapping periods of admission and three cases were of the same D8 genotype, with a single nucleotide difference.
Discussion
The epidemiological linkages of the cases and laboratory findings suggest nosocomial transmission in Wards A and B. As a result of this investigation, the hospital implemented a new policy of isolating suspected measles cases instead of waiting until they had been laboratory confirmed. This investigation emphasizes the importance of early identification and isolation of suspected measles cases within health care institutions and reinforces the requirement for high measles vaccination coverage of health care workers.
Introduction
Measles is an acute, highly communicable viral disease transmitted by droplet spread or direct contact with the nasal or throat secretions of an infected person. The average incubation period for measles is 14 days with a range of seven to 21 days.1 Outbreaks of measles are known to occur in settings where unvaccinated susceptible populations congregate such as boarding schools, colleges, universities, factories, offices and institutions.
Measles is a notifiable disease under the Infectious Diseases Act in Singapore. All medical practitioners/laboratories are required to notify the Ministry of Health of any persons suspected or confirmed to have measles. Measles is endemic in Singapore with the majority of cases being sporadic and in unvaccinated persons. The D9 genotype has been endemic and detected in Singapore since 2010. Other genotypes seen in Singapore include G3 and H1 in 2010, and D4, D8 and G3 in 2011.2,3
Measles vaccination has been compulsory in Singapore since 1985. Under the National Childhood Immunization Programme, the first dose of the trivalent measles, mumps and rubella (MMR) vaccine is to be administered by the age of two years and the second dose at six to seven years of age. However, in view of the large proportion of reported cases of measles among unvaccinated infants and preschoolchildren, the MMR immunization schedule was amended effective 1 December 2011, with the first dose to be given at 12 months of age and the second dose at 15 to 18 months of age. Over the past six years, the national vaccination coverage for the MMR vaccine has been consistently maintained at around 95% for the first dose and above 90% for the second dose.4
On 23 August 2011, the Ministry of Health was notified of a cluster of five measles cases in a public hospital. Of these cases, three had a previous admission to the institution within the past two weeks. We report herein the epidemiological investigations for the outbreak.
Method
A clinical case of measles was defined as a child presenting with rash, fever and one or more of the following symptoms: cough, coryza or conjunctivitis, who had been admitted to the hospital. A laboratory-confirmed case was defined as a clinical case with one or more of the following laboratory results: presence of measles immunoglobulin M or detection of measles virus either through immunofluorescence antigen testing or measles polymerase chain reaction (PCR). A nosocomial (intra-hospital) case was defined as a confirmed case who had contact with another confirmed case in the hospital seven to 21 days before the onset of symptoms with no other source identified. A community-acquired case was a confirmed case that had no prior history of being at the hospital during the 21 days before onset of symptoms or was known to have contact with another confirmed case (non-hospital).
As part of our investigations into the possibility of intra-hospital transmission of measles, we reviewed the movement history within the hospital for all 14 cases to determine any common exposures in place and time.
Genotyping was conducted from throat swabs collected from cases. These were sent to the laboratory at Kandang Kerbau Women’s and Children’s Hospital for testing by real-time PCR, and positive samples were forwarded to the National Public Health Laboratory for genotyping. Genotyping was conducted following the protocol provided by the WHO Western Pacific Regional Office at the training workshop in Hong Kong Special Administrative Region (China)in 2009. A 540-bp region of nucleoprotein (N) gene was amplified and sequenced. Sequences of N gene were submitted to Measles Nucleotide Surveillance5 to determine the genotypes.
Results
Active case detection revealed 14 laboratory-confirmed measles cases admitted to the same hospital between 2 August and 20 August 2011. Seven were female sand seven were males, with ages ranging from four months to three years. None of the cases has been vaccinated against measles; four had missed their vaccination and the other 10 were too young for vaccination. Two family clusters were detected: one involving a pair of siblings and the other, a pair of cousins. These cases were not in the nosocomial group as they were not linked to the hospital.
The epidemic curve for these 14 cases is shown in Fig. 1. Seven cases had been previously admitted to the hospital for unrelated illnesses approximately two to three weeks before their admission for measles and were therefore considered nosocomial cases; the other seven were considered community-acquired cases.
Fig. 1.
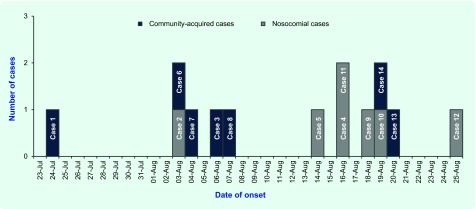
Onset of illness of 14 reported laboratory-confirmed cases of measles in a public hospital, 24 July to 25 August 2011
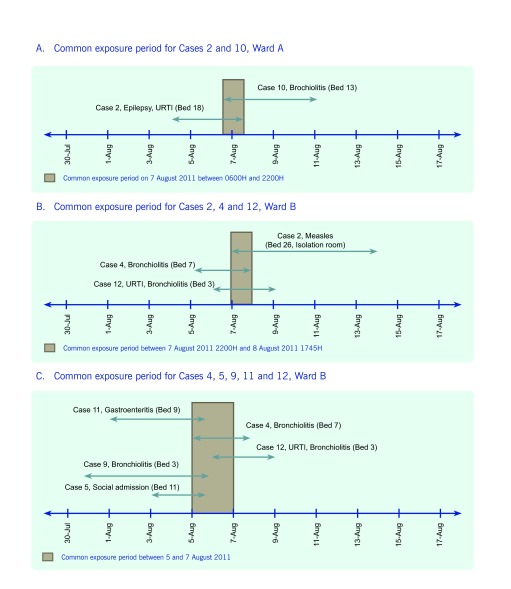
Our investigations at the hospital identified two general wards, Ward A and Ward B, as two areas where the seven nosocomial cases could be epidemiologically linked to each other in time and place. All patients are free to interact with each other in these wards except for those in isolation who are discouraged from leaving their room. The maximum capacity for either ward is 38, comprising 30 beds and eight infant cots. Genotyping of the measles virus for Cases 2, 4, 5, 10, 12 and 13 was performed while the rest of the samples were unsuitable or unavailable for genotyping.
Ward A
Case 2 was hospitalized in Ward A from 4 to 7 August 2011 and was subsequently diagnosed with measles on 7 August. Case 10 was admitted for bronchiolitis from 7 to 9 August 2011. Both their beds were in the same cubicle. They shared a common period of exposure of approximately 16 hours (Fig. 2). Case 10 was then readmitted on 21 August 2011 for measles – an onset date 10 days after the common exposure. The measles virus isolated from both cases was of D8 genotype and were genotypically 100% identical.
Fig. 2.
Common exposure for nosocomial cases in Kandang Kerbau Women and Children’s Hospital, Singapore, 2011
Ward B
Cases 2 (transferred from Ward A), 4, 5, 9, 11 and 12 were admitted to Ward B.
Cases 2, 4 and 12 had overlapping periods of hospitalization in Ward B, although their beds were situated in different cubicles and rooms. Case 2 was transferred to Bed 26 in the isolation room of Ward B on 7 August after being diagnosed with measles and was nursed in this room from 7 to 14 August 2011. Case 4 was hospitalized for bronchiolitis from 5 to 8 August 2011. Cases 2 and 4 shared an overlapping period in Ward B for approximately 21 hours (Fig. 2). Case 12 was hospitalized for upper respiratory tract infection and bronchiolitis from 6 to 8 August 2011. Cases 2 and 12 shared an overlapping period of hospitalization in Ward B for approximately 1.5 days.
Case 4 was subsequently readmitted on 21 August 2011 for measles with an onset date eight days after the patient’s overlapping period of hospitalization with Case 2. Case 12 was readmitted on 26 August 2011 for measles, 16 days after the patient’s overlapping hospital period with Case 2. Cases 2, 4 and 12 were infected with measles of the same genotype D8, with a single nucleotide difference found in Case 2.
Cases 5, 9 and 11 had no exposure to Case 2 while they were in Ward B, but had common exposure with each other and with Cases 4 and 12 (Fig. 2). The genotype for Case 5 was 100% identical to that of Cases 4 and 12. Cases 9 and 11 were unable to be genotyped.
One community-acquired case (Case 13) also had D8 genotype; however, there was no evidence of any contact with any of the nosocomial cases.
Discussion
The epidemiological linkages of the reported cases and laboratory findings suggest nosocomial transmission of measles in Wards A and B. Case 2 could have infected Case 10 while they were both in Ward A as their measles virus genotypes were 100% identical. They had a relatively close physical proximity within the ward, and the onset of symptoms for Case 10 was 10 days after the overlapping period of hospitalization, which falls within the known incubation period of measles (seven to 21 days).
There are two possible hypotheses for transmission within Ward B.
Case 2 was the index case infecting Cases 4 and 12 based on the assumption that Case 2 may not have been fully compliant with isolation while in the ward. As Cases 5, 9 and 11 did not have any exposure to Case 2 during the time they were in Ward B, they could have been community-acquired infections. Cases 2, 4 and 12 had similar genotype with only one nucleotide difference. Cases 4 and 12 also developed measles symptoms eight days and 15 days, respectively, after their overlapping period of hospitalization with Case 2, which is within the known incubation period for measles.
The index case was an unknown patient or visitor with measles (before the onset of rash) who was present in Ward B from 5 to 7 August 2011. This person could have infected Cases 4, 5, 9, 11 and 12, as they were in two neighbouring cubicles in the ward during the same period (5 to 7 August 2011) (Fig. 2). These five cases also developed measles symptoms between nine and 16 days after 5 to 7 August 2011, which falls within the known incubation period for measles.
Not all 14 cases were able to have their samples genotyped as they were either unavailable or unsuitable, including samples from both the nosocomial and community-acquired group. The one sample that was genotyped from the community-acquired group was for Case 13 who had the same D8 genotype as the nosocomial cases. As there was no epidemiological link between this case and any of the nosocomial cases, we consider this an incidental finding.
During the investigation we noted some cases were not immediately isolated at admission, even though they were suspected measles cases. Isolation occurred only after laboratory confirmation of measles, potentially exposing other susceptible children to the virus. As a result, the hospital implemented a new policy of isolating all suspected measles cases from admission and then de-isolating them once laboratory results were confirmed negative.
There were no reports of frontline health care workers from Wards A and B with measles in the months of July and August 2011. Therefore, health care workers as a source of infection for these cases were unlikely. All frontline health care workers in this hospital are required to prove their measles and rubella immunity by documentary evidence of vaccination or serology testing.
Conclusion
This report describes a possible nosocomial outbreak of measles occurring within a health care setting. Similar incidents have previously been reported in the Republic of Korea,6 Australia7 and in Pennsylvania8 and Indiana9 in the United States of America. The risk of measles transmission within health care settings emphasizes the importance of early identification and isolation of suspected measles cases and reinforces the requirement for high vaccination coverage of health care workers against measles. Other measures to prevent or reduce nosocomial transmission include maintaining high vaccination coverage and timely vaccination of children according to vaccination schedules.
Acknowledgements
Professor Goh Kee Tai, Ministry of Health Singapore
Conflict of interest
None declared.
Funding
None.
References
- 1.Manual for the surveillance of vaccine-preventable diseases (4th Edition, 2008). Atlanta: Centers for Disease Control and Prevention (CDC); 2008. http://www.cdc.gov/vaccines/pubs/surv-manual/chpt07-measles.html accessed 7 February 2012. [Google Scholar]
- 2.World Health Organization Western Pacific Region. Measles and Rubella Bulletin. 2012;6(1) http://www.wpro.who.int/immunization/documents/measles_rubella_bulletin_vol6_issue1.pdf accessed 10 October 2012. [Google Scholar]
- 3.World Health Organization Western Pacific Region. Measles and Rubella Bulletin. 2012;6(9) http://www.wpro.who.int/immunization/documents/MRBulletin_Vol6Issue9.pdf accessed 10 October 2012. [Google Scholar]
- 4.Communicable diseases surveillance in Singapore 2010. Singapore: Ministry of Health; 2011. [Google Scholar]
- 5.Measles Nucleotide Surveillance. http://www.hpa-bioinformatics.org.uk/Measles/Public/Web_Front/main.php accessed 10 October 2012.
- 6.Choi WS, et al. Outbreak of measles in the Republic of Korea, 2007: importance of nosocomial transmission. The Journal of Infectious Diseases. 2011;204(Suppl 1):S483–90. doi: 10.1093/infdis/jir087. [DOI] [PubMed] [Google Scholar]
- 7.Kelly HA, Riddell MA, Andrews RM. Measles transmission in healthcare settings in Australia. The Medical Journal of Australia. 2002;176:50–1. doi: 10.5694/j.1326-5377.2002.tb04278.x. [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention (CDC) Hospital-associated measles outbreak - Pennsylvania, March-April 2009. MMWR. Morbidity and Mortality Weekly Report. 2012;61:30–2. [PubMed] [Google Scholar]
- 9.Centers for Disease Control and Prevention (CDC) Import-associated measles outbreak–Indiana, May-June 2005. MMWR, Morbidity and Mortality Weekly Report. 2005;54:1073–5. [PubMed] [Google Scholar]