Abstract
Objectives
The aim of this study was to evaluate differences in craniofacial morphology, head posture and hyoid bone position between mouth breathing (MB) and nasal breathing (NB) patients.
Methods
Mouth breathing patients comprised 34 skeletal Class I subjects with a mean age of 12.8 ± 1.5 years (range: 12.0–15.2 years). Thirty-two subjects with skeletal Class I relationship were included in the NB group (mean 13.5 ± 1.3 years; range: 12.2–14.8 years). Twenty-seven measurements (15 angular and 12 linear) were used for the craniofacial analysis. Additionally, 12 measurements were evaluated for head posture (eight measurements) and hyoid bone position (four measurements). Student’s t-test was used for the statistical analysis. Probability values <0.05 were accepted as significant.
Results
Statistical comparisons showed that sagittal measurements including SNA (p < 0.01), ANB (p < 0.01), A to N perp (p < 0.05), convexity (p < 0.05), IMPA (p < 0.05) and overbite (p < 0.05) measurements were found to be lower in MB patients compared to NB. Vertical measurements including SN-MP (p < 0.01) and PP-GoGn (p < 0.01), S-N (p <0.05) and anterior facial height (p < 0.05) were significantly higher in MB patients, while the odontoid proses and palatal plane angle (OPT-PP) was greater and true vertical line and palatal plane angle (Vert-PP) was smaller in MB patients compared to NB group (p < 0.05 for both). No statistically significant differences were found regarding the hyoid bone position between both groups.
Conclusions
The maxilla was more retrognathic in MB patients. Additionally, the palatal plane had a posterior rotation in MB patients. However, no significant differences were found in the hyoid bone position between MB and NB patients.
Keywords: Mouth breathing, Craniofacial morphology, Hyoid bone
1. Introduction
Nasal obstruction, chronic allergic rhinitis and hypertrophic adenoids decrease capacity for nasal breathing (NB) and compensating for this by mouth breathing (MB) might be necessary (Oulis et al., 1994). Respiratory airway function influences facial morphology and both craniofacial (Gungor and Turkkahraman, 2009) and cervical functions (Huggare and Laine-Alava, 1997; McNamara, 1981). The breathing pattern may influence the development of the transverse relationship between the maxilla mandible, resulting in the development of a posterior cross bite (Rubin, 1980). MB can affect the form of the jaw or cause malocclusions (Hartsook, 1946), and it has been shown to lead to the so-called “adenoid face”, which is characterized by a narrow upper dental arch, retroclined mandibular incisors, an incompetent lip seal, a steep mandibular plane angle and increased anterior facial height (Lessa et al., 2005; Peltomäki, 2007; Linder-Aronson, 1970). Ricketts (1968) suggested that head extension represents a functional response in MB patients to compensate for nasal obstruction.
MB has been reported to cause changes in human head posture (Cuccia et al., 2008). The treatment of hypertrophic adenoids (Linder-Aronson, 1970) and nasal obstruction (Vig et al., 1980) with a nasal clip has been shown to alter head posture. Children with MB who have enlarged tonsils can develop the extension of their head posture and the low position of hyoid bone position (Behlfelt et al., 1990a,b). However, some authors have concluded that the hyoid position is maintained in a stable position in children with MB (Bibby, 1984; Ferraz et al., 2007).
MB is associated with a low tongue posture and the absence of a contact surface between the tongue and soft palate; this latter factor was termed “posterior oral incompetence” by Ballard (1951). This problem is caused by enlarged adenoid tissue that reduces the airway space and leads to postural adaptations at the level of the oropharynx. The hyoid bone drops in relation to the mandible, and creates a relatively constant air-space diameter in the anteroposterior direction. This neuromuscular recruitment may cause changes in the mandibular resting position and neck extension (Tourné, 1991). Thus, the breathing pattern could represent a major factor that underlies the hyoid bone position (Graber, 1978).
The impact of MB in dentofacial growth remains unclear (Warren, 1990). The aim of this study was to evaluate differences in craniofacial morphology, head posture and hyoid bone position between MB and NB patients. The null hypothesis assumed that there were no significant differences in the craniofacial morphology, head posture and hyoid bone position between MB and NB children.
2. Materials and methods
This study was approved by the Regional Ethics Committee on Research of the Faculty of Dentistry, Erciyes University. A power analysis established by G*Power Ver. 3.0.10. (Franz Faul, Universität Kiel, Germany) software, based on 1:1 ratio between groups with a sample size of 33 patients would give more than 80% power to detect significant differences with an effect size of 0.33 [to detect a clinically meaningful difference of 1 mm (±3 mm) for the distance of the A to N perp] between two groups and at a significance level of α = 0.05.
In the present study, 155 MB and 50 NB skeletal Class I subjects were evaluated and 34 MB and 32 NB patients were selected by the sample selection criteria presented in Table 1. Sixty-seven pretreatment cephalometric radiographs of Class I patients taken by a standard technique formed the sample for this study. All children were admitted for orthodontic treatment to the Department of Orthodontics, University of Erciyes, with a Class I skeletal relationship (ANB: 2.2° ± 1.5° and 2.9° ± 0.9° in MB and NB, respectively). Prior to their participation in the study, written informed consent forms were signed by the parents of the patients.
Table 1.
Adopted criteria for sample selection.
| Inclusion criteria | Exclusion criteria |
|---|---|
| Age between 12–16 years | Age under 12 or older 16 years |
| Skeletal Class I relationship | Skeletal Class II/III relationship |
| Permanent dentition | Mixed/deciduous dentition |
| Lack of orthodontic treatment and/or maxillary functional orthopedic treatment | Young people had been under orthodontic treatment |
| No history of nasal respiratory complex surgery | Previous history of nasal respiratory complex surgery |
| No vestibular or equilibrium problems | Vestibular or equilibrium problems |
| No visual, hearing or swallowing disorders, and facial or spinal abnormalities (i.e., torticollis, scoliosis, or kyphosis) | Visual, hearing or swallowing disorders, and facial or spinal abnormalities (i.e., torticollis, scoliosis, or kyphosis) |
| No caries | Extensive carious lesions. |
| Enough sharpness and contrast for a good visualization of the bone structures on radiographs | Radiographs without sharpness and contrast for a good visualization of the bone structures |
| No allergic or acute rhinitis | Allergic or acute rhinitis |
| No sleeping disorders with mild apnea hypoapnea index (AHI) (5–15) | Severe sleeping disorders with moderate and severe apnea hypoapnea index (AHI)(15–30 and greater than 30) |
Patients were divided into two groups according to their breathing pattern as follows: Group I, MB children as the experimental group and Group II, NB children used as the control group. Group I comprised 16 boys and 18 girls (mean age, 12.8 ± 1.5 years; range: 12.0–15.2 years). On clinical examination, MB patients showed lip incompetence, dry lips at rest, dental crowding in the upper arch, an ‘adenoidal face’ (Fig. 1) and a reduced maxillary transverse dimension with a unilateral or bilateral cross bite. These factors were consistent with the diagnosis of MB according to Moyers’ criteria (1973). The evaluation of the breathing pattern was adapted from the study by Cuccia et al. (2008). MB was demonstrated by the presence of condensed water vapor on the surface of a mirror placed in front of the mouth Figs. 2–4).
Figure 1.

Typical case example from the mouth breathing group.
Figure 2.

(1) SNA angle (SNA), (2) SNB angle (SNB), (3) ANB angle (ANB), (4) Saddle/Sella angle (SN-Ar), (5) Articular angle, (6) Gonial/Jaw angle (Ar-Go/MP), (7) SN plane to mandibular plane angle (SN-MP), (8) Palatal-Mand angle (PP-GoGn), (9) Y-Axis, (10) SN-NPog, (11) NA-Apog (convexity), (12) FMA, (13) FMIA, (14) IMPA, (15) Mand Plane to Occ Plane (MP-OP).
Figure 3.
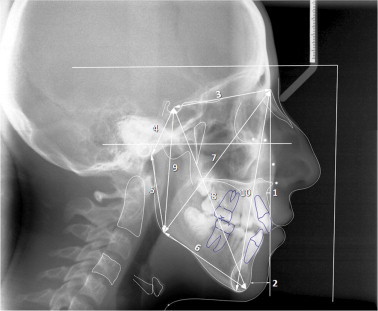
(1) A point to Nasion perpendicular (A to N perp), (2) Pogonion to Nasion perpendicular (Pog to N perp), (3) S-N: distance between sella and nasion point, (4) Posterior Cranial Base (S-Ar), (5) Ramus Height (Ar-Go), (6) Mandibular Body Length (Go-Gn), (7) Nasion-Gonion Length (N-Go), (8) Y-Axis Length (S-Gn), (9) Posterior Facial Height (S-Go), (10) Anterior Facial Height (Na-Me).
Figure 4.

(1) CVT-SN:angle between the CVT line and SN plane, (2) OPT-SN:angle between the OPT line and SN plane, (3) CVT-Hor: angle between the CVT line and horizontal line, (4) OPT-Hor: angle between the OPT line and horizontal line, (5) CVT-PP: angle between the CVT line and palatal plane, (6) OPT-PP: angle between the OPT line and palatal plane, (7) H-MP: distance to the H point measured perpendicular to the mandibular plane (MP), (8) H-Me: distance between the H point and menton, (9) H-MP: angle between the H-menton line and mandibular plane, (10) H-C4: distance between the H point and most inferior/posterior point on the fourth cervical vertebra corpus.
Group II (NB-control) comprised eight boys and 24 girls (mean 13.5 ± 1.3 years; age range: 12.2–14.8 years). This group was chosen at random from a group of children according to inclusion criteria (Table 1) with various orthodontic problems, but who did not have a past history or any clinical signs of MB.
2.1. Craniofacial measurements
Twenty-seven measurements (15 angular and 12 linear) (Figs. 2 and 3) were used for craniofacial analysis (Table 2). Additionally, 12 measurements were evaluated to assess head posture (eight measurements) and the hyoid bone (four measurements) Fig. 4, as described in Table 2.
Table 2.
Description of the measurements used in the study.
| Craniofacial analysis |
|---|
| Angular measurement |
| SNA angle (SNA): inward angle toward the cranium between the NA line and the SN plane |
| SNB angle (SNB): inward angle toward the cranium between the NB line and the SN plane |
| ANB angle (ANB): angle between the NA and NB lines, obtained by subtracting SNB from SNA |
| Saddle/sella angle (SN-Ar): inward angle toward the cranium between the S-Ar line and the SN plane |
| Articular angle: inward angle between the S-Ar line and the Ar-Go line |
| Gonial/jaw angle (Ar-Go/MP): inward angle toward the cranium between the Ar-Go line and the mandibular plane (MP) |
| SN plane to mandibular plane angle (SN-MP): angle between the SN plane and the MP |
| Palatal–mand angle (PP-GoGn): angle between the PP plane and the MP |
| Y-Axis: inward angle toward the cranium between the S-Gn line and the SN plane |
| SN-NPog: inward angle toward the cranium between the N-Pog line and the SN plane |
| NA-Apog (convexity): inward angle between the NA line and the APog line |
| FMA: angle between the frankfurt horizontal plane and the MP |
| FMIA: angle between the frankfurt horizontal plane and the mandibular incisor axis |
| IMPA: angle between the MP and the mandibular incisor axis |
| Mand plane to Occ plane (MP-OP): angle between the MP and occlusal plane (OP) |
| Linear measurements |
| A point to nasion perpendicular (A to N perp): distance between A point and N perpendicular line measured perpendicular to N perpendicular line |
| Pogonion to nasion perpendicular (Pog to N perp): distance between pogonion and N perpendicular line measured from the perpendicular to N perpendicular line |
| S-N: distance between sella and nasion point |
| Posterior cranial base (S-Ar): distance between sella and articular |
| Ramus height (Ar-Go): distance between articular and gonion |
| Mandibular body length (Go-Gn): distance between gonion and gnathion |
| Nasion–gonion length (N-Go): distance between nasion and gonion |
| Y-Axis length (S-Gn): distance between sella and gnathion |
| Posterior facial height (S-Go): distance between sella and gonion |
| Anterior facial height (Na-Me): distance between nasion and menton |
| Overjet: distance between labial surfaces of the upper and lower incisors |
| Overbite: distance between the upper and lower incisor margins |
| Head posture and hyoid bone |
| Vert-SN: inward angle toward the cranium between the true vertical line and sella-nasion (SN) plane |
| Vert-PP: inward angle between the true vertical line and palatal plane (PP) |
| CVT-SN: angle between the CVT line (an extended line from posterior extremity of the odontoid process of the second cervical vertebra to and the most inferior/posterior point on the fourth cervical vertebra corpus) and SN plane |
| OPT-SN: angle between the OPT line (connecting the tangent point at the superior, posterior extremity of the odontoid process of the second cervical vertebra and the most inferior/posterior point on the second cervical vertebra corpus) and SN plane |
| CVT-Hor: angle between the CVT line and horizontal line (Perpendicular to true vertical line) |
| OPT-Hor: angle between the OPT line and horizontal line |
| CVT-PP: angle between the CVT line and palatal plane (PP) |
| OPT-PP: angle between the OPT line and palatal plane (PP) |
| H-MP: distance to the H point (most superior and anterior point on the body of the hyoid bone) measured perpendicular to the mandibular plane (MP) |
| H-Me: distance between the H point and menton |
| H-MP: angle between the H-menton line and mandibular plane (MP) |
| H-C4: distance between the H point and most inferior/posterior point on the fourth cervical vertebra corpus |
2.2. Statistical analysis
All statistical analyses were performed using the Statistical Package for Social Sciences v.13.0 (SPSS Inc., Chicago, Illinois, USA). The normality test of Shapiro–Wilks and Levene’s variance homogeneity test was applied to the data. The data were found to be normally distributed, and there was homogeneity of variance between the groups. Arithmetic mean and standard deviation values were calculated for each measurement. Group differences were analyzed with Student’s t-test.
To determine the errors associated with radiographic measurements, 15 radiographs were selected at random. Their tracings and measurements were repeated 8 weeks after the first measurements. A paired sample t-test was applied to the first and second measurements, and the differences between the measurements were insignificant (0.849). Correlation analysis applied to the same measurements showed the highest r-value (0.988) for the overbite and the lowest r-value (0.867) for servical vertebra and sella-nasion plane angle (CVT-SN) and insicor mandibular plane angle (IMPA) measurements. Probability values less than 0.05 were accepted as significant.
3. Results
The descriptive statistics and statistical comparisons of angular and linear craniofacial measurements are shown in Table 3. Statistically significant differences were found between Group I and Group II in 10 out of 27 measurements. SNA (p < 0.01), ANB (p < 0.01), A to N perp (p < 0.05), convexity (p < 0.05), IMPA (p < 0.05) and overbite (p < 0.05) measurements were found to have smaller values; but SN-MP (p < 0.01) and PP-GoGn (p < 0.01) from angular measurements, and S-N (p < 0.05) and anterior facial height (p < 0.05) from linear measurements were higher in Group I than Group II. Thus, this part of the null hypothesis was rejected.
Table 3.
Descriptive statistics and statistical comparisons of angular and linear craniofacial measurements in mouth breathing and nasal breathing children.
| Craniofacial analysis | Mouth breathing (n = 34) |
Nasal breathing (n = 32) |
Sig. | ||
|---|---|---|---|---|---|
| Angular measurement (°) | Mean | SD | Mean | SD | |
| SNA | 78,503 | 3,287 | 80,415 | 2,709 | ** |
| SNB | 76,303 | 3,217 | 77,418 | 2,511 | NS |
| ANB | 2,209 | 1,572 | 2,997 | 0.931 | ** |
| SN-Ar | 124,944 | 6,261 | 125,221 | 5,704 | NS |
| Articular angle | 140,882 | 6,911 | 139,976 | 6,730 | NS |
| Ar-Go/MP | 128,691 | 8,223 | 126,939 | 5,332 | NS |
| SN-MP | 35,156 | 4,570 | 31,939 | 2,144 | ** |
| PP-GoGn | 27,335 | 6,118 | 23,324 | 3,756 | ** |
| Y-Axis | 70,797 | 3,141 | 69,961 | 2,237 | NS |
| SN-Npog | 77,179 | 2,733 | 78,145 | 2,481 | NS |
| NA-Apog | 2,729 | 4,008 | 5,061 | 3,348 | * |
| FMA | 27,032 | 5,747 | 24,945 | 3,805 | NS |
| FMIA | 63,779 | 7,682 | 61,885 | 6,005 | NS |
| IMPA | 88,926 | 6,015 | 92,755 | 5,892 | * |
| MP-OP | 18,765 | 4,403 | 18,424 | 3,796 | NS |
| Linear measurements (mm) | |||||
| A to N perp | −1,191 | 2,955 | 0.373 | 2,919 | * |
| Pog to N perp | −4,779 | 6,174 | -3,712 | 5,063 | NS |
| S-N | 68,815 | 4,836 | 65,964 | 4,594 | * |
| S-Ar | 37,088 | 4,274 | 35,848 | 3,985 | NS |
| Ar-Go | 45,274 | 4,356 | 46,588 | 4,232 | NS |
| Go-Gn | 76.19 | 8,389 | 72.5 | 6,777 | NS |
| N-Go | 113,009 | 8,602 | 110,024 | 7,271 | NS |
| S-Gn | 126,406 | 10,312 | 122,348 | 9,450 | NS |
| Posterior facial height | 75,076 | 6,090 | 75,127 | 5,653 | NS |
| Anterior facial height | 118,971 | 9,918 | 114,058 | 8,577 | * |
| Overjet | 2,938 | 32,074 | 3,236 | 1,234 | NS |
| Overbite | 0.335 | 25,650 | 1,400 | 1,244 | * |
Descriptive data for the variables that described head posture and hyoid bone are given for the MB and control group in Table 4. According to the statistical analysis, the OPT-PP measurement was significantly higher and the Vert-PP measurement was lower in MB patients compared to the controls (p < 0.05 for both). No significant difference was found for the other head posture measurements. According to the results regarding head posture, the null hypothesis regarding head posture was also rejected.
Table 4.
Descriptive statistics and statistical comparisons of head posture and hyoid bone measurements in mouth breathing and nasal breathing children.
| Head posture and hyoid bone | Mouth breathing (n = 34) |
Nasal breathing (n = 32) |
Mean difference | Sig. | ||
|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | |||
| Vert-SN | 81,876 | 3,309 | 83,006 | 2,664 | 0.129 | NS |
| Vert-PP | 89,674 | 3,957 | 91,609 | 3,677 | 0.042 | * |
| CVT-SN | 105,838 | 6,772 | 104,318 | 5,825 | 0.329 | NS |
| OPT-SN | 100,824 | 7,325 | 98,318 | 6,126 | 0.134 | NS |
| CVT-Hor | 95,309 | 6,160 | 94,636 | 5,936 | 0.651 | NS |
| OPT-Hor | 90,368 | 6,195 | 88,606 | 6,250 | 0.251 | NS |
| CVT-PP | 97,191 | 7,620 | 95,333 | 4,484 | 0.23 | NS |
| OPT-PP | 93,632 | 7,079 | 90,273 | 6,216 | 0.043 | * |
| H-MP | 15,265 | 5,609 | 14,121 | 3,988 | 0.341 | NS |
| H-Me | 42,324 | 9,237 | 44,061 | 4,981 | 0.344 | NS |
| H-MP | 20,765 | 6,651 | 18,788 | 6,204 | 0.213 | NS |
| H-C4 | 51,029 | 4,523 | 52,091 | 3,964 | 0.311 | NS |
No statistically significant differences were found for the hyoid bone position between the two groups, and consequently this part of the null hypothesis was accepted.
4. Discussion
MB alters the balance between the intra-oral and extra-oral neuromuscular regions. MB changes the muscle forces exerted by the tongue, cheeks, and lips upon the maxillary arch (Cuccia et al., 2008). In MB patients, it is generally expected that a narrow maxillary arch with a high palatal vault will be found, associated with a posterior cross bite, a Class II or III dental malocclusion, and an anterior open bite (Rubin, 1980; Hartsook, 1946; Lessa et al., 2005; Peltomäki, 2007; Linder-Aronson, 1970). The head is generally extended to compensate for the smaller airway space. It is important to notice that head extension increases the sagittal extension of the pharyngeal airway in patients with unobstructed airways and normal breathing function (Hellsing, 1989), but this compensatory mechanism is insufficient to alter the breathing pattern (Huggare and Laine-Alava, 1997).
It has been recognized that mandibular posture as it relates to the craniomaxillary complex is influenced by both proprioceptive intra- and extra-oral forces. Accommodative posture influences the load in several joints of the craniovertebral region, which results in unfavorable dentofacial and craniofacial growth (Darnell, 1983). The purpose of the present study was to evaluate the craniofacial morphology, hyoid bone position and head posture in MB and NB patients.
In this study, respiration types were evaluated according to the study of Cuccia et al. (2008), but for an objective evaluation of breathing mode, rhinomanometry was used to determine the degree of MB (Linder-Aronson, 1970). Furthermore, clinical evaluations might be insufficient and the degree of nasorespiratory obstruction may need to be identified and quantified (Vig, 1998).
All patients were selected for skeletal classification according to the ANB angle. Only Class I patients with a normal vertical growth pattern were included in the study sample. Thus, this study differed from previous studies as a standard and homogenous group of patients was used, divided into two groups only according to their breathing pattern.
When the maxillary sagittal skeletal relationship is evaluated, reduced SNA and A to N perp measurements in MB patients were determined. These values indicate a tendency for maxillary deficiency, which was consistent with the findings of Seto et al. (2001). However, Lowe et al. (1996) reported that the maxillary position did not show any major difference in MB patients compared to the control subjects. However, they also found that the maxillary skeletal position is retrognathic in the anteroposterior direction.
In the current study, we found that vertical measurements (PP-GoGn, SN-MP and anterior facial height) were higher in MB patients, which was consistent with the findings of previous studies (Hellsing et al., 1987). Patients in the MB group are likely to present with increased mandibular inclination, characterized by decreased posterior facial height and increased lower anterior facial height. These measurements suggest that respiratory function influences craniofacial development (Lessa et al., 2005). These skeletal measurements indicate a tendency for MB children to present with a dolichocephalic skeletal pattern. Frasson et al. (2006) found no difference between NB and MB patients when facial vertical patterns were assessed. Their study included an assessment of the FMA, SN-GoGn and Y-axis angle values, and they observed no significant alterations between the MB and NB groups in terms of posterior facial height measurements. We found higher values for SN-MP, PP-GoGn and anterior facial height (N-Me) in MB patients but no significant differences in posterior facial height between groups.
Pirilä-Parkkinen et al. (2010) stated that nocturnal sleeping disorders cause larger craniocervical angles (NSL–CVT and NSL–OPT), but their patients had a mean age of 7.3 years and a Class II skeletal pattern. In this age period, growth and development are still continuing and can further influence the craniocervical angles. Cuccia et al. (2008) suggested that a stable breathing pattern has not been established in growing patients and the natural head posture might be altered in MB patients. The MB and NB children in the current study had a mean age of 12.8 and 13.5 years, respectively, with a Class I skeletal relationship.
The present main finding was that MB patients have increased OPT-PP and reduced Vert-PP angles compared with the control group. Cuccia et al. (2008) found that a reduction of cervical lordosis and increased extension of the atlanto-occipital joint maintained the Frankfort horizontal plane. Their cohort included growing children and a natural head posture may develop after maxillofacial growth and development is complete.
Several studies have shown that MB is associated with head posture variation and increased craniocervical extension (Behlfelt et al., 1990a,b; Huggare and Laine-Alava, 1997) in order to increase the airway measurements (Warren, 1990) and the oropharyngeal permeability (Ricketts, 1968). Behlfelt et al. (1990a,b) found that extended head posture is associated with a low hyoid bone posture and MB. We cannot conclude from this current study that an extended craniocervical head posture occurs with nasorespiratory obstruction, due to the absence of data regarding nasal airflow resistance.
In mouth breathers, one might expect a different head posture to be adopted to facilitate breathing, especially where MB is due to an obstructed nasopharynx; however, Bibby (1984) indicated that, this was not reflected in the position of the hyoid. We found that the hyoid bone is maintained in a stable position, probably in order to protect the proper airway ratios, and it was not influenced by the respiratory pattern. This finding has been supported by other investigators (Bibby, 1984; Ferraz et al., 2007). However, some studies have found that the hyoid bone is located in a lower position in MB patients (Ozbek et al., 1998). According to the present data, MB has no effect on the hyoid bone position during rest, which indicates that there is no permanent alteration in skeletal morphology due to MB as far as the hyoid bone and its relation to the mandible are concerned.
This study was limited as the measurements were based on two-dimensional cephalometric radiographs. To overcome this weakness, all radiographs were taken by the same technician and the same author (F.I.U.) performed all measurements carefully to ensure they were consistent. Further 3D studies are needed to give a highly precise quantitative analysis.
5. Conclusions
Within the limitations of this cross-sectional study, the following conclusions can be drawn: (i) according to the craniofacial measurements, the maxillary skeletal base is positioned posteriorly in MB patients which affects facial convexity compared to a NB control sample. In general, vertical measurements were higher and lower incisors were retroclined in the MB group; (ii) the palatal plane showed a posterior rotation according to the second cervical vertebra in the MB group; and (iii) the position of the hyoid was stable in patients with MB.
Footnotes
Peer review under responsibility of King Saud University.

References
- Ballard C.F. The facial musculature and anomalies of the dentoalveolar structure. Trans. Eur. Orthod. Soc. 1951:137–148. [Google Scholar]
- Behlfelt K., Linder-Aronson S., McWilliam J., Neander P., Laage-Hellman J. Cranio-facial morphology in children with and without enlarged tonsils. Eur. J. Orthod. 1990;12(3):233–243. doi: 10.1093/ejo/12.3.233. [DOI] [PubMed] [Google Scholar]
- Behlfelt K., Linder-Aronson S., Neander P. Posture of the head, the hyoid bone, and the tongue in children with and without enlarged tonsils. Eur. J. Orthod. 1990;12(4):458–467. doi: 10.1093/ejo/12.4.458. [DOI] [PubMed] [Google Scholar]
- Bibby R.E. The hyoid bone position in mouth breathers and tongue-thrusters. Am. J. Orthod. 1984;85(5):431–433. doi: 10.1016/0002-9416(84)90164-7. [DOI] [PubMed] [Google Scholar]
- Cuccia A.M., Lotti M., Caradonna D. Oral breathing and head posture. Angle Orthod. 2008;78(1):77–82. doi: 10.2319/011507-18.1. [DOI] [PubMed] [Google Scholar]
- Darnell M.W. A proposed chronology of events for forward head posture. Cranio. 1983;1(4):49–54. doi: 10.1080/07345410.1983.11677844. [DOI] [PubMed] [Google Scholar]
- Ferraz M.J., Nouer D.F., Teixeira J.R., Bérzin F. Cephalometric assessment of the hyoid bone position in oral breathing children. Braz. J. Otorhinolaryngol. 2007;73(1):45–50. doi: 10.1016/S1808-8694(15)31121-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frasson J.M., Magnani M.B., Nouer D.F., de Siqueira V.C., Lunardi N. Comparative cephalometric study between nasal and predominantly mouth breathers. Braz. J. Otorhinolaryngol. 2006;72(1):72–81. doi: 10.1016/S1808-8694(15)30037-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graber L.W. Hyoid change following orthopedic treatment of mandibular prognathism. Angle Orthod. 1978;48(1):33–38. doi: 10.1043/0003-3219(1978)048<0033:HCFOTO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Gungor A.Y., Turkkahraman H. Effects of airway problems on maxillary growth: a review. Eur. J. Dent. 2009;3(3):250–254. [PMC free article] [PubMed] [Google Scholar]
- Hartsook J.T. Mouth breathing as a primary etiologic factor in the production of malocclusion. J. Dent. Child. 1946;13(4):91–94. [PubMed] [Google Scholar]
- Hellsing E. Changes in the pharyngeal airway in relation to extension of the head. Eur. J. Orthod. 1989;11(4):359–365. doi: 10.1093/oxfordjournals.ejo.a036007. [DOI] [PubMed] [Google Scholar]
- Hellsing E., McWilliam J., Reigo T., Spangfort E. The relationship between craniofacial morphology, head posture and spinal curvature in 8, 11 and 15-year-old children. Eur. J. Orthod. 1987;9(4):254–264. doi: 10.1093/ejo/9.4.254. [DOI] [PubMed] [Google Scholar]
- Huggare J., Laine-Alava M.T. Nasorespiratory function and head posture. Am. J. Orthod. Dentofacial Orthop. 1997;112(5):507–511. doi: 10.1016/s0889-5406(97)70078-7. [DOI] [PubMed] [Google Scholar]
- Lessa F.C., Enoki C., Feres M.F., Valera F.C., Lima W.T., Matsumoto M.A. Breathing mode influence in craniofacial development. Braz. J. Otorhinolaryngol. 2005;71(2):156–160. doi: 10.1016/S1808-8694(15)31304-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linder-Aronson S. Adenoids. Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the dentition. A biometric, rhinomanometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol. Suppl. 1970;265:1–132. [PubMed] [Google Scholar]
- Lowe A.A., Ono T., Ferguson K.A., Pae E.K., Ryan C.F., Fleetham J.A. Cephalometric comparisons of craniofacial and upper airway structure by skeletal subtype and gender in patients with obstructive sleep apnea. Am. J. Orthod. Dentofacial Orthop. 1996;110(6):653–664. doi: 10.1016/s0889-5406(96)80043-6. [DOI] [PubMed] [Google Scholar]
- McNamara J.A. Influence of respiratory pattern on craniofacial growth. Angle Orthod. 1981;51(4):269–300. doi: 10.1043/0003-3219(1981)051<0269:IORPOC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- Moyers R.E. third ed. Year Book Medical Publishers; Chicago, IL: 1973. Handbook of Orthodontics. 442. [Google Scholar]
- Oulis C.J., Vadiakas G.P., Ekonomides J., Dratsa J. The effect of hypertrophic adenoids and tonsils on the development of posterior crossbite and oral habits. J. Clin. Pediatr. Dent. 1994;18(3):197–201. [PubMed] [Google Scholar]
- Ozbek M.M., Miyamoto K., Lowe A.A., Fleetham J.A. Natural head posture, upper airway morphology and obstructive sleep apnoea severity in adults. Eur. J. Orthod. 1998;20(2):133–143. doi: 10.1093/ejo/20.2.133. [DOI] [PubMed] [Google Scholar]
- Peltomäki T. The effect of mode of breathing on craniofacial growth – revisited. Eur. J. Orthod. 2007;29(5):426–429. doi: 10.1093/ejo/cjm055. [DOI] [PubMed] [Google Scholar]
- Pirilä-Parkkinen K., Löppönen H., Nieminen P., Tolonen U., Pirttiniemi P. Cephalometric evaluation of children with nocturnal sleep-disordered breathing. Eur. J. Orthod. 2010;32(6):662–671. doi: 10.1093/ejo/cjp162. [DOI] [PubMed] [Google Scholar]
- Ricketts R.M. Respiratory obstruction syndrome. Am. J. Orthod. 1968;54(7):495–503. doi: 10.1016/0002-9416(68)90218-2. [DOI] [PubMed] [Google Scholar]
- Rubin R.M. Mode of respiration and facial growth. Am. J. Orthod. 1980;78(5):504–510. doi: 10.1016/0002-9416(80)90301-2. [DOI] [PubMed] [Google Scholar]
- Seto B.H., Gotsopoulos H., Sims M.R., Cistulli P.A. Maxillary morphology in obstructive sleep apnoea syndrome. Eur. J. Orthod. 2001;23(6):703–714. doi: 10.1093/ejo/23.6.703. [DOI] [PubMed] [Google Scholar]
- Tourné L.P. Growth of the pharynx and its physiologic implications. Am. J. Orthod. Dentofacial Orthop. 1991;99(2):129–139. doi: 10.1016/0889-5406(91)70115-D. [DOI] [PubMed] [Google Scholar]
- Vig K.W. Nasal obstruction and facial growth: the strength of evidence for clinical assumptions. Am. J. Orthod. Dentofacial Orthop. 1998;113(6):603–611. doi: 10.1016/s0889-5406(98)70219-7. [DOI] [PubMed] [Google Scholar]
- Vig P.S., Showfety K.Y., Phillips C. Experimental manipulations of head posture. Am. J. Orthod. 1980;77(3):258–268. doi: 10.1016/0002-9416(80)90081-0. [DOI] [PubMed] [Google Scholar]
- Warren D.W. Effect of airway obstruction upon facial growth. Otolaryngol. Clin. North Am. 1990;23(4):699–712. [PubMed] [Google Scholar]


