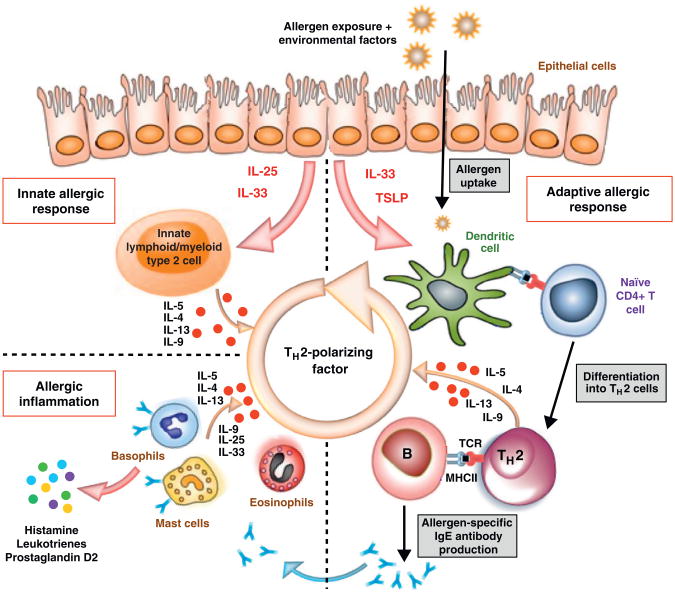
Figure 1.
Schematic representation of pathogenic processes in allergic disease. The hallmark of Type I allergic immune response is production of allergen-specific IgE and activation of mast cells, basophils and eosinophils. Recent literature suggests that TH2 cytokines are induced after allergen exposure, even before the establishment of an allergen-specific adaptive immune response. Thus both innate immunity and adaptive immunity are instrumental in establishing Type I allergic immune response. The upper strata of the figure depicts that upon allergen exposure in a suitable environmental milieu, IL-25, IL-33 and TSLP are produced by epithelial cells. For the innate arm, these cytokines act on innate lymphoid/myeloid type 2 cells that are capable of producing large amounts of TH2 cytokines, such as IL-4, IL-5, IL-9 and IL-13. For the adaptive arm, allergens are taken up and processed by TSLP and IL-33 primed DCs and presented to naïve allergen-specific T cells in a TH2 milieu that drives their differentiation into TH2 cells. Dominant TH2 responses to allergens during the sensitization phase lead to immunoglobulin class switching to IgE as well as recruitment and activation of pro-inflammatory cells such as mast cells, basophils and eosinophils.