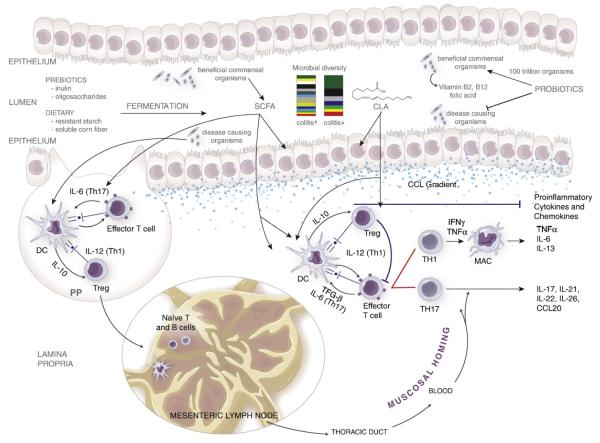
Fig. 1.
Mucosal immune mechanisms of nutritional protection against colitis. The disruption of the epithelial barrier or the infiltration of pathogenic bacteria into the LP or Peyer’s patches (PP) activates DC and macrophages (MAC), which process the antigen and present it on their surfaces through the MHC class II complex. These APC either stay in the PP or are transported to the MLN, where they promote the differentiation of naïve T cells into effector and regulatory T cells. The cytokine environment secreted in part by the APC skews the differentiation of naïve CD4+ T cells into T helper (Th1 and Th17) or Treg subsets. Th1 cells differentiate in the presence of IL-12; IL-6 and TGF-β induce a Th17 phenotype, whereas IL-10 induces a Treg cell differentiation. These mature T cells migrate back to the LP following a chemokine gradient (CCL), where they start the adaptive immune response towards the antigen, resulting in the production of effector and proinflammatory cytokines. The administration of prebiotics (inulin, oligofructose), dietary fibers (resistant starch, soluble corn fiber) and probiotics decreases effector responses and proinflammatory cytokine expression by the production of SCFAs. Dietary compounds such as CLA, PUA, ESA and ABA, as well as probiotic-derived SCFA, can activate PPARγ to suppress inflammation.