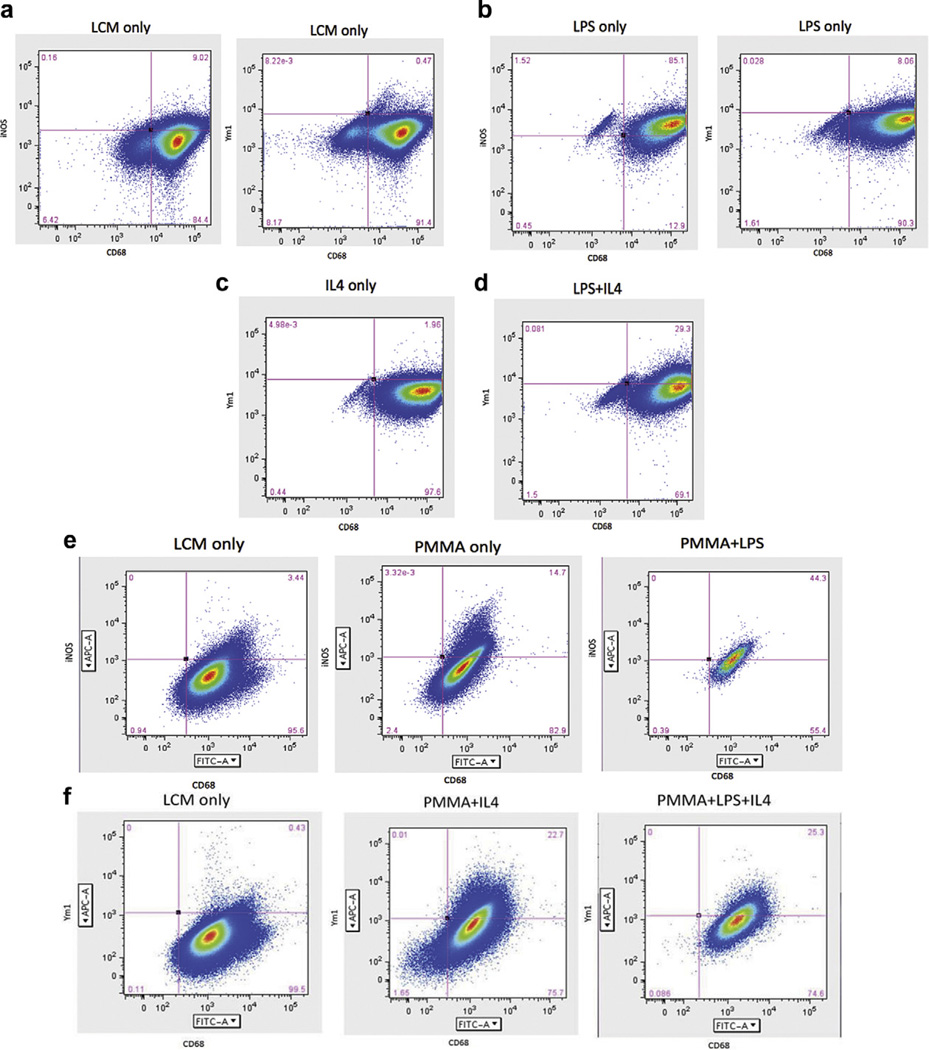
Fig. 3.
FACS analysis of macrophages cultured in vitro stimulated with LPS with/without PMMA and IL-4. Cells were gated using CD68 and either an M1 label (iNOS) or an M2 label (Ym1). (a) Macrophages stimulated with LCM sorted by CD68 and iNOS showed that LCM stimulation does not differentiate cells into M1 or M2 macrophages. (b) LPS stimulated macrophages gated for CD68 and iNOS showed that a majority of the cells differentiated into M1 macrophages. (c) IL-4 stimulation alone did not differentiate cells into M2 macrophages. (d) LPS stimulation for 3 days followed by LPS + IL-4 stimulation for 3 days resulted in an increase in M2 expression compared to IL-4 alone. (e) FACS sorting of macrophages stimulated with LCM showed an undifferentiated state. Stimulation with PMMA particles increased M1 expression. Addition of PMMA with LPS resulted in a greater increase in M1 expression. (f) FACS sorting of macrophages stimulated with LCM showed an undifferentiated state; however, stimulation with PMMA followed by IL-4 increased M2 expression. Similarly, stimulation with PMMA and LPS followed by IL-4 resulted in an increase in M2 expression. This suggests that macrophage polarization to the anti-inflammatory M2 phenotype is more successful if M1 rather than uncommitted, non-activated macrophages are administered IL-4. Both LPS and PMMA are sufficient to induce an M1 inflammatory state. Addition of IL-4 to M1 stimulated macrophages results in a conversion of 20–30% of the macrophages to an M2 phenotype.