Abstract
Gastrobronchial fistula is a rare but serious complication of laparoscopic sleeve gastrectomy with significant morbidity and mortality. We present the case of a 30-year-old man who underwent laparoscopic sleeve gastrectomy for morbid obesity and presented later with a history of chronic productive cough. Upper gastrointestinal series showed the presence of a communicating fistula between the stomach and the left lung bronchial tree.
Keywords: Gastric leak, gastrobronchial fistula, laparoscopic sleeve gastrectomy, subphrenic collection
Obesity, which is a chronic disease associated with comorbidities, should be controlled by physical exercise and changes in dietary habits, and surgical treatment is indicated when clinical measures are inefficient.[1] Laparoscopic sleeve gastrectomy is a relatively new and evolving surgical technique indicated in the treatment of morbid obesity. This procedure has been gaining widespread popularity among both patients and surgeons alike.[2] Post-operative complications are mainly represented by gastric fistula, with an occurrence rate of 0-5.1% in the literature. This complication is difficult to manage and requires multiple radiological, endoscopic and surgical procedures.[3]
Case Report
A 30-year-old male patient with morbid obesity underwent a laparoscopic sleeve gastrectomy in another hospital. During the post-operative course, the patient experienced abdominal pain and vomiting. An upper gastrointestinal contrast study was performed, which showed gastric leak and left subphrenic collection. The patient underwent percutaneous drainage of the left subphrenic collection, and was discharged home after improvement with oral antibiotic.
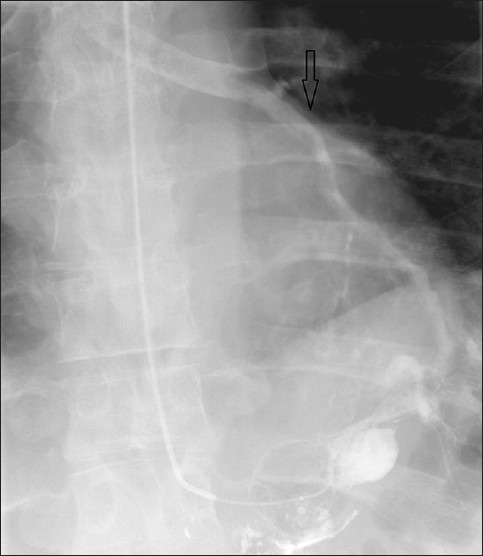
About 4 months later, the patient was referred to our hospital. He had persistent cough with yellowish sputum, which aggravated with drinking, and on and off fever for 3 weeks. Physical examination was unremarkable. Chest radiograph was performed and showed elevated left hemidiaphragm with basal atelectasis otherwise unremarkable. An upper gastrointestinal contrast study was performed, which showed gastric leak, subphrenic collection, and gastrobronchial fistula [Figure 1 and Figure 2].
Figure 1.

Upper gastrointestinal water-soluble contrast study showed gastric leak and fistula tract “arrow”
Figure 2.
Upper gastrointestinal water-soluble contrast study showed evidence of gastrobronchial fistula evidence communication and contrast opacification of the left lung bronchial tree “arrow”
The patient was managed conservatively with wide-spectrum antibiotic, CT-guided percutaneous drainage of the left subphrenic collection, endoscopic covered stent of gastric fistula and nasojejunostomy feeding. The patient was discharged home after clinical improvement, with a surgical outpatient clinic appointment.
Discussion
Gastric fistula following bariatric surgery occurs in 0.9-2.6% of the cases, reaching 8% in second operations, and is most often located at the level of the angle of His.[1] It has been postulated that most gastric fistulas and leaks occur not because of staple line dehiscence but because of ischemia in the gastric wall next to the staple line.[2] Stenosis of the gastric pouch increased the pressure and directed the food to the fistula at the angle of His, leading to the appearance of recurrent subphrenic infection.[1] Gastrobronchial fistula is caused secondary to subphrenic abscess. Infection may spread by lymphatic flow from below to above the diaphragm or by directly eroding through the diaphragm, causing a lung abscess that eventually drains into a bronchus.[4]
The clinical presentation of gastrobronchial fistula includes a cough upon swallowing, fever, dyspnea, hemoptysis and recurrent pneumonia.[3] A contrast study of the upper gastrointestinal tract is the most successful means of diagnosing gastrobronchial fistula. Other methods that have been used include methylene blue staining and measurement of the pH of the bronchial secretion.[4] The fistula may connect at any site in the respiratory tract so as to be difficult to locate, and may not be visualized during bronchoscopy.[3]
The treatment of gastrobronchial fistulas should be tailored to the clinical state of the patient. In the absence of major signs of sepsis, an initial conservative management can be tried.[2]
Treatment with antibiotics is important in managing the coexistent lung infection. In cases of response failure, CT-guided aspiration and drainage of the abscess can be tried. Endoscopic balloon dilatation, self-expanding plastic stent placement and stricturotomy or septoplasty along with adequate nutritional support are minimally invasive and effective techniques in resolving gastric stenosis, which is considered the leading cause of perpetuation of the fistula.[2]
Reoperation may provide little benefit because of the difficult access to the region of the upper abdomen with adhesions and fibrosis. In addition to the complexity of major abdominal and thoracic reoperations, with its high morbidity rate, it is often not efficient to completely heal gastrobronchial fistula.[5]
Conclusion
Gastrobronchial fistula is a very rare but serious complication post laparoscopic sleeve gastrectomy, and is difficult to diagnose. Clinicians should have a high suspicion of whether patients have persistent pulmonary or abdominal symptoms in spite of optimal management.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Campos JM, Siqueira LT, Meira MR, Ferraz AA, Ferraz EM, Guimarães MJ. Gastrobronchial fistula as a rare complication of gastroplasty for obesity: A report of two cases. J Bras Pneumol. 2007;33:475–9. doi: 10.1590/s1806-37132007000400018. [DOI] [PubMed] [Google Scholar]
- 2.Abraham A, Virdi RP, Rajan D, Singh J, Mustacchia P, Iqbal J, et al. Gastrobronchial fistula following laparoscopic sleeve gastrectomy. BMJ Case Rep. 2012 doi: 10.1136/bcr-2012-006789. doi:10.1136/bcr-2012-006789. (http://casereports.bmj.com/content/2012/bcr-2012-006789 .) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fuks D, Dumont F, Berna P, Verhaeghe P, Sinna R, Sabbagh C, et al. Case report-complex management of a postoperative bronchogastric fistula after laparoscopic sleeve gastrectomy. Obes Surg. 2009;19:261–4. doi: 10.1007/s11695-008-9643-3. [DOI] [PubMed] [Google Scholar]
- 4.Jha PK, Deiraniya AK, Keeling-Roberts CS, Das SR. Gastrobronchial fistula: A recent series. Interact Cardiovasc Thorac Surg. 2003;2:6–8. doi: 10.1016/S1569-9293(02)00065-8. [DOI] [PubMed] [Google Scholar]
- 5.Campos JM, Pereira EF, Evangelista LF, Siqueira L, Neto MG, Dib V, et al. Gastrobronchial fistula after sleeve gastrectomy and gastric bypass: Endoscopic management and prevention. Obes Surg. 2011;21:1520–9. doi: 10.1007/s11695-011-0444-8. [DOI] [PubMed] [Google Scholar]


