Abstract
Periodontal disease is a chronic inflammatory disease which represents a primarily anaerobic Gram-negative oral infection that results in gingival inflammation, loss of attachment, bone destruction. Bacterial endotoxins in the form of lipopolysaccharides (LPS) that are instrumental in generating a host-mediated tissue destructive immune response by mobilizing their defensive cells and releasing cytokines like Interleukin-1β (IL-1β), Tumor Necrosis Factor-α (TNF-α), and Interleukin-6 (IL-6), which lead to tissue destruction by stimulating the production of the collagenolytic enzymes: Matrix metalloproteinases (MMPs). Since the host-mediated tissue destruction is to be controlled, various means have been employed for modulating this response. Statins, 3-hydroxy-3-methylglutarylcoenzyme A (HMG CoA) reductase inhibitors, besides having lipid-lowering abilities also have antioxidant, antithrombotic, anti-inflammatory, immunomodulatory and osteomodulatory properties. All of these pleiotropic effects of statins point out to it perhaps becoming the novel host modulation agent in periodontics.
Keywords: Anti-inflammatory, host modulation, immunomodulation, osseo-modulatory, periodontics, statins
INTRODUCTION
Periodontal disease is a chronic inflammatory disease which represents a primarily anaerobic Gram-negative oral infection that results in gingival inflammation, loss of attachment, bone destruction.[1] Certain organisms within the microbial flora of dental plaque are the major etiologic agents of periodontitis which produce endotoxins in the form of lipopolysaccharides (LPS) that are instrumental in generating a host-mediated tissue destructive immune response by mobilizing their defensive cells and releasing cytokines like Interleukin-1β (IL-1β), Tumor Necrosis Factor-α (TNF-α), and Interleukin-6 (IL-6), which lead to tissue destruction by stimulating the production of the collagenolytic enzymes: Matrix metalloproteinases (MMPs).[2]
Since the host-mediated tissue destruction is to be controlled, various means have been employed for modulating this response. These include -Inhibition of MMP's with antiproteinases, blocking the proinflammatory cytokines and prostaglandins by use of anti-inflammatory drugs, and by inhibiting the osteoclasts activity by use of bone sparing agents.[3]
Statins, 3-hydroxy-3-methylglutarylcoenzyme A (HMG CoA) reductase inhibitors, can be fermentation derived statins include simvastatin, pravastatin whereas atorvastatin, cerivastatin, fluvastatin, pitavastatin and rosuvastatin are synthetic stains. Synthetic statins have a higher potency as compared to the fermented statins. Statins were primarily approved as lipid lowering agent to prevent cardiovascular events. Statins lower low density lipoprotein-C (LDL-C), but recent studies provide compelling evidence that statins also possess anti-inflammatory activity, independent of their lipid-lowering effects.[4,5]
Statins differ in terms of their chemical structures, pharmacokinetic profiles, and lipid-modifying efficacy. The chemical structures of statins govern their water solubility, which in turn influences their absorption, distribution, metabolism and excretion. Lovastatin, pravastatin and simvastatin are derived from fungal metabolites and have elimination half-lives of 1-3 h. Atorvastatin, fluvastatin and rosuvastatin are fully synthetic compounds, with elimination half-lives ranging from 1 h for fluvastatin to 19 h for rosuvastatin. Atorvastatin, simvastatin, lovastatin and fluvastatin are relatively lipophilic compounds. Lipophilic statins are more susceptible to metabolism by the cytochrome P (450) system. Pravastatin and rosuvastatin are relatively hydrophilic and not significantly metabolized by cytochrome P (450) enzymes. All statins are selective for effect in the liver, largely because of efficient first-pass uptake. The bioavailability of the statins differs greatly, from 5% for lovastatin and simvastatin to 60% or greater for cerivastatin.[6]
These structures can be broadly divided into three parts: An analogue of the target enzyme substrate, HMG-CoA; a complex hydrophobic ring structure that is covalently linked to the substrate analogue and is involved in binding of the statin to the reductase enzyme; side groups on the rings that define the solubility properties of the drugs and therefore many of their pharmacokinetic properties.[7]
Potential pleiotropic effects of statins involve immunomodulatory, antioxidant, antithrombotic and endothelium stabilization actions,[8] as well as angiogenesis promotion and increase of osteoblastic differentiation, inducing bone formation.[9] In addition, statins can inhibit tumor cells growth and enhance intracellular calcium mobilization. It was observed that inhibitors of HMG-CoA reductase induce a reduction of the formation of osteoclasts in rodents.[10] Human subjects treated with statins have shown a reduction in the number of bone fractures.[11]
MECHANISM OF PLEIOTROPIC ACTION OF STATINS
Anti-inflammatory
Continuously growing evidences have recognized inflammation as a major component of atherosclerosis. When atherosclerotic process is at work, each characteristic lesion of atherosclerosis represents a different stage in a chronic inflammatory process in the artery; if unabated and excessive, this process will result in an advanced, complicated lesion.
Certain cell and cytokine mediated markers like C-reactive protein (CRP) are associated both with atherosclerosis and periodontal disease, proving a link between cardiovascular disease and periodontal disease.
CRP, a proinflammatory marker, is produced in liver and it induces release of IL-1, IL-6, and tumor necrosis factor by macrophages. CRP calcium-dependently binds to low density lipoproteins (LDL)[12] and induces foam cell formation. Kleemann and colleagues have shown that atorvastatin at doses higher than those required for cholesterol lowering, decrease basal and IL-1β-induced plasma human C-Reactive Protein (huCRP) levels.[13] Statins also inhibits Intercellular Adhesion Molecule-1 (ICAM-1) upregulation and chemotaxis in adherent human monocytes.[14]
Simvastatin lowers high sensitivity (hsCRP) by 14 days, independent of its effect on LDL cholesterol.[15] This rapid impact of a statin on hsCRP has potential implications in the management of acute coronary syndromes.
JUPITER trail showed that statins could be beneficial in the primary prevention of cardiovascular disease in patients with elevated hs CRP, but relatively low cholesterol levels and other cardiovascular risks.[16]
Effect of statin on bone
Statins have been found to be a potent activator of bone morphogenetic protein (BMP-2) which accounts for major osteoinductive potential of bone. Simvastatin, mevastatin and atorvastatin stimulates BMP-2 transcription.
Mechanism of action involves reduction in mevalonate pathway intermediates and inhibition of prenylation by statins is responsible for a large proportion of the pleiotropic effects of these drugs. Mevalonate, farnesyl pyrophosphate and geranyl-geranyl pyrophosphate all inhibited statin-stimulated bone formation. Furthermore, because geranylgeranyl pyrophosphate inhibited statin stimulated bone formation, inhibition of prenylation due to geranylgeranylation must play a major role in the stimulation of bone formation by these drugs.[17]
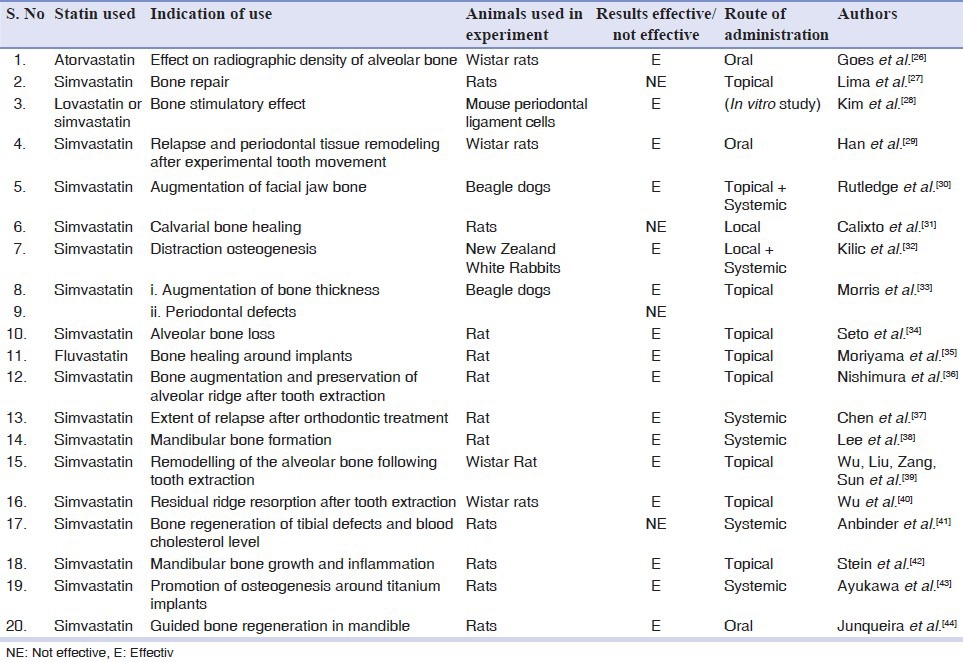
Also statins influence the production of Receptor activator of nuclear factor kappa-B ligand (RANKL) and Osteoprotegrin by human gingival fibroblasts to favor bone catabolism under non-inflammatory conditions [Table 1].[18]
Table 1.
Different studies done on animal to explore the beneficial effects of different statins in animal models of dental conditions
Immunomodulatory
Various experiments have shown statins to have immunomodulatory effects. Primary effects of statins include inhibition of major histocompatibility complex II expression. Antigen presenting cells such as endothelial cells and monocytes requires co-stimulation by Interferon gamma. This is done by inhibition of promoter IV of class II transcription activator which is an important regulator in this pathway. Another effect on immune system is mediated by binding of statins to leucocyte function associated antigen and preventing its binding to ICAM1. This leads to inhibition of its function in leucocyte adhesion and extravasation.[19]
Another mode of exerting immunomodulatory effects by statins include inhibition of release of proinflammatory cytokines like IFN-γ, TNF-α, IL-1β, IL-6 in various cell types like microglia, astrocytes, and mononuclear cells. These cytokines play an important role in T cell differentiation. Thus disrupting cytokine production can adversely affect the immune reactions of the body.[19]
Antioxidant effects of statins
Antioxidant effect of statins is proposed as mechanism of its various pleiotropic effects. Many studies done to assess the antioxidant potential of statins have concluded favorably. Various mechanisms of its antioxidant activity are being proposed. Production of Nicotinamide adenine dinucleotide phosphate (NADPH) oxidase, a major source of oxidant production is inhibited by statins. Simvastatin has been reported most effective in this regard.[20]
Few animal studies have demonstrated the upregulation and also increased activity of antioxidant enzyme catalase.[21] Studies with other antioxidant enzymes have shown inconsistent activity. Other studies have also demonstrated the free radical scavenging activity of statins.[22,23] Direct scavenging reactive oxygen species (ROS) prevents its interaction with lipids, proteins and deoxyribonucleic acid. In this regard simvastatin and atorvastatin were more active against hydroxyl radical, and that fluvastatin was more active against peroxyl radical.[24]
Statins have been shown in both human studies and animal models to upregulate Nitric oxide synthase-3 (NOS-3) expression[25] thereby increasing the levels of Nitric oxide (NO). Inhibition of formation of NO further inhibits conversion of superoxide ion to highly ROS peroxynitrite.
Implications of pleiotropic effects of statins in dental conditions
Various animal [Table 1] and human studies have been done to assess the effect of statins. A randomized controlled clinical trial on patients with chronic periodontitis showed that there was a greater decrease in gingival index (GI) and probing depth (PD) and more clinical attachment level gain with significant intrabony defect fill at sites treated with scaling and root planning (SRP) plus locally delivered simvastatin than with SRP alone.[45]
Another study showed beneficial effect of atorvastatin on bone alveolar loss and tooth mobility in subjects with periodontal disease.[46]
Few other cross sectional studies failed to conclusively state the beneficial effects of statin on periodontal conditions as such.[47,48]
Statins in implants
According to Takeshita, et al. (1993) a mesh-like woven bone structure was predominantly formed around the implant 5 days after implantation, and then diminished gradually.[46] Ayukawa, et al., showed that simvastatin promotes osteogenesis around titanium implants. Under the administration of statin, a similar mesh-like structure of bone was seen around the implant even at 30 days after the implantation which resulted in an improved implant fixation and that the bone network can successfully disperse the stress applied to the implant.[43] Also, topical application of statin affects bone healing around implants[35] [Table 1, S.No: 18, 10].
Adverse effects
Adverse effects of statin therapy includes myalgias and muscle cramps. SLCO1B1 gene, which participates in the absorption of statins, has been shown to significantly increase the risk of myopathy.[49] It is suggested that the risk of myopathy is lowest with pravastatin and fluvastatin probably because they are more hydrophilic and as a result have less muscle penetration. Coenzyme Q10 (ubiquinone) levels are decreased in statin use;[50] Q10 supplements are sometimes used to treat statin-associated myopathy.[51]
Liver enzymes derangement is seen in statin therapy which includes increased hepatic transaminases enzyme. Also an increase in creatine phosphokinase, up to 10 times higher than normal, has been reported.[52] Cerivastatin was withdrawn from the market in 2001 due to cases of rhabdomyolysis. Combining any statin with a fibrate or niacin, another category of lipid-lowering drugs, increases the risks for rhabdomyolysis to almost 6.0 per 10,000 person-years.[53] Consumption of grapefruit or bitter oranges inhibits the metabolism of statins.
Cruz, et al., attempted to describe the oral adverse effects of statins which are often underestimated. They identified dry mouth, itching or paresthesia in tongue, lips or throat, bitterness and cough as major complaints and all of them subsided with interruption of statin therapy. Insomnia was often associated with above mentioned symptoms.[54]
A study by Saxlin, et al., has also stated that in patients with no plaque or gingival bleeding statin medication has shown an increased likelihood of deepened periodontal pockets which could be attributed to disruption of immune homeostasis in periodontal tissues as a result of statin therapy predisposing the periodontal tissues to a breakdown.[47]
The frequency and severity of adverse effect due to statin treatment is related to their own potency. Atorvastatin being the most potent (per mg of active principle), is maximally associated with the adverse effects whereas Fluvastatin exhibits the lowest efficacy, which correlates with less adverse effect. Simvastatin, pravastatin and lovastatin pose intermediate risk of adverse effect.
CONCLUSION
Thus multiple effects of statins have been demonstrated in various experiments. The ultimate effect of statins on host is a combination of all these effects. Immunomodulation, anti-inflammatory effects and antioxidants effects are thought to contribute most towards its beneficial effects. Its effect on promotion of osteogenesis makes it a potential blockbuster in periodontics. Other systemic diseases where role of statins are being studied are Alzheimers, multiple sclerosis, vitiligo, osteoporosis, pulmonary hypertension and many more.
There is a great potential to explore the pleiotropic effects of statins. Various animal and few human studies have demonstrated the effects of statins and the underlying mechanisms thereof. Further controlled clinical trials are needed to establish these facts. Further studies with varying doses of statins in varying disease conditions can help us maximize the beneficial effects. Also studies regarding its long term safety will be needed when statins are prescribed more commonly and for longer duration of actions. Continuing research to first establish and secondly to understand the mechanism of these effects would help not only to effectively use statins for various disorders but also, it will provide an insight to the role of statins as a potential host modulating agent for treatment of periodontal diseases.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Flemmig TF. Periodontitis. Ann Periodontol. 1999;4:32–88. doi: 10.1902/annals.1999.4.1.32. [DOI] [PubMed] [Google Scholar]
- 2.Takashiba S, Naruishi K, Murayama Y. Perspective of cytokine regulation for periodontal treatment: Fibroblast biology. J Periodontol. 2003;74:103–10. doi: 10.1902/jop.2003.74.1.103. [DOI] [PubMed] [Google Scholar]
- 3.Reddy MS, Geurs NC, Gunsolley JC. Periodontal host modulation with antiproteinase, anti-inflammatory, and bone-sparing agents. A systematic review. Ann Periodontol. 2003;8:12–37. doi: 10.1902/annals.2003.8.1.12. [DOI] [PubMed] [Google Scholar]
- 4.Schonbeck U, Libby P. Inflammation, Immunity, and HMG-Co A reductase inhibitors: Statins as anti-inflammatory agents? Circulation. 2004;109:II18–26. doi: 10.1161/01.CIR.0000129505.34151.23. [DOI] [PubMed] [Google Scholar]
- 5.Jain MK, Ridker PM. Anti-inflammatory effects of statins: Clinical evidence and basic mechnasims. Nat Rev Drug Discov. 2005;4:977–87. doi: 10.1038/nrd1901. [DOI] [PubMed] [Google Scholar]
- 6.Schachter M. Chemical, pharmacokinetic and pharmacodynamic properties of statins: An update. Fundam Clin Pharmacol. 2005;19:117–25. doi: 10.1111/j.1472-8206.2004.00299.x. [DOI] [PubMed] [Google Scholar]
- 7.Rao SK, Prasad T, Mohanta GP, Manna PK. An overview of statins as hypolipidemic drugs. Int J Pharm Sci Drug Res. 2011;3:178–83. [Google Scholar]
- 8.Landmesser U, Bahlmann F, Mueller M, Spiekermann S, Kirchhoff N, Schulz S, et al. Simvastatin versus ezetimibe: Pleiotropic and lipid lowering effects on endothelial function in humans. Circulation. 2005;111:2356–63. doi: 10.1161/01.CIR.0000164260.82417.3F. [DOI] [PubMed] [Google Scholar]
- 9.Maeda T, Matsunuma A, Kurahashi I, Yanagawa T, Yoshida H, Horiuchi N. Induction of osteoblast differentiation indices by statins in MC3T3-E1 cells. J Cell Biochem. 2004;92:458–71. doi: 10.1002/jcb.20074. [DOI] [PubMed] [Google Scholar]
- 10.Bellosta S, Ferri N, Bernini F, Paoletti R, Corsini A. Non-lipid-related effects of statins. Ann Med. 2000;32:164–76. doi: 10.3109/07853890008998823. [DOI] [PubMed] [Google Scholar]
- 11.Meier CR, Schlienger RG, Kraenzlin ME, Schlegel B, Jick H. HMG-CoA reductase inhibitors and risk of fractures. JAMA. 2000;283:3205–10. doi: 10.1001/jama.283.24.3205. [DOI] [PubMed] [Google Scholar]
- 12.Chang MK, Binder CJ, Torzewski M, Witztum JL. C-reactive protein binds to both oxidized LDL and apoptotic cells through recognition of a common ligand: Phosphorylcholine of oxidized phospholipids. Proc Natl Acad Sci U S A. 2002;99:13043–8. doi: 10.1073/pnas.192399699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cano EA. How statins and fibrates lower CRP. Blood. 2004;103:3996–7. [Google Scholar]
- 14.Montecucco F, Burger F, Pelli G, Poku NK, Berlier C, Steffens S, et al. Statins inhibit C-reactive protein-induced chemokine secretion, ICAM-1 upregulation and chemotaxis in adherent human monocytes. Rheumatology. 2009;48:233–42. doi: 10.1093/rheumatology/ken466. [DOI] [PubMed] [Google Scholar]
- 15.Plenge JK, Hernandez TL, Weil KM, Poirier P, Grunwald GK, Marcovina SM, et al. Simvastatin lowers C-Reactive protein within 14 days an effect independent of low-density lipoprotein cholesterol reduction. Circulation. 2002;106:1447–52. doi: 10.1161/01.cir.0000029743.68247.31. [DOI] [PubMed] [Google Scholar]
- 16.Ridker PM. Rosuvastatin in the primary prevention of cardiovascular disease among patients with low levels of low-density lipoprotein cholesterol and elevated high-sensitivity C-reactive protein: Rationale and design of the JUPITER trial. Circulation. 2003;108:2292–7. doi: 10.1161/01.CIR.0000100688.17280.E6. [DOI] [PubMed] [Google Scholar]
- 17.Garrett R, Mundy GR. The role of statins as potential targets for bone formation. Arthritis Res. 2002;4:237–40. doi: 10.1186/ar413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stein SH, Dean IN, Rawal SY, Tipton DA. Statins regulate interleukin-1β-induced RANKL and osteoprotegerin production by human gingival fibroblasts. J Periodontal Res. 2011;46:483–90. doi: 10.1111/j.1600-0765.2011.01364.x. [DOI] [PubMed] [Google Scholar]
- 19.Chow SC. Immunomodulation by statins: Mechanisms and potential impact on autoimmune diseases. Arch Immunol Ther Exp (Warsz) 2009;57:243–51. doi: 10.1007/s00005-009-0038-5. [DOI] [PubMed] [Google Scholar]
- 20.Jeon SM, Bok SH, Jang MK, Lee MK, Nam KT, Park YB, et al. Antioxidative activity of naringin and lovastatin in high cholesterol-fed rabbits. Life Sci. 2001;69:2855–66. doi: 10.1016/s0024-3205(01)01363-7. [DOI] [PubMed] [Google Scholar]
- 21.Delbosc S, Morena M, Djouad F, Ledoucen C, Descomps B, Cristol JP. Statins, 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors, are able to reduce superoxide anion production by NADPH oxidase in THP-1-derived monocytes. J Cardiovasc Pharmacol. 2002;40:611–7. doi: 10.1097/00005344-200210000-00015. [DOI] [PubMed] [Google Scholar]
- 22.Suzumura K, Yasuhara M, Narita H. Superoxide anion scavenging properties of fluvastatin and its metabolites. Chem Pharm Bull (Tokyo) 1999;47:1477–80. doi: 10.1248/cpb.47.1477. [DOI] [PubMed] [Google Scholar]
- 23.Suzumura K, Yasuhara M, Tanaka K, Odawara A, Narita H, Suzuki T. An in vitro study of the hydroxyl radical scavenging property of fluvastatin, and HMG-CoA reductase inhibitor. Chem Pharm Bull (Tokyo) 1999;47:1010–2. doi: 10.1248/cpb.47.1010. [DOI] [PubMed] [Google Scholar]
- 24.Franzoni F, Quinones-Galvan A, Regoli F, Ferrannini E, Galetta F. A comparative study of the in vitro antioxidant activity of statins. Int J Cardiol. 2003;90:317–21. doi: 10.1016/s0167-5273(02)00577-6. [DOI] [PubMed] [Google Scholar]
- 25.Wassmann S, Nickenig G. Interrelationship of free oxygen radicals and endothelial dysfunction-modulation by statins. Endothelium. 2003;10:23–33. doi: 10.1080/10623320303357. [DOI] [PubMed] [Google Scholar]
- 26.Goes P, Lima AP, Melo IM, Rêgo RO, Lima V. Effect of Atorvastatin in radiographic density on alveolar bone loss in wistar rats. Braz Dent J. 2010;21:193–8. doi: 10.1590/s0103-64402010000300003. [DOI] [PubMed] [Google Scholar]
- 27.Lima CE, Calixto JC, Anbinder AL. Influence of the association between simvastatin and demineralized bovine bone matrix on bone repair in rats. Braz Oral Res. 2011;25:42–8. doi: 10.1590/s1806-83242011000100008. [DOI] [PubMed] [Google Scholar]
- 28.Kim IS, Jeong BC, Kim OS, Kim YJ, Lee SE, Lee KN, et al. Lactone form 3-hydroxy-3-methylglutaryl-coenzyme A reductase inhibitors (statins) stimulate the osteoblastic differentiation of mouse periodontal ligament cells via the ERK pathway. J Periodontal Res. 2011;46:204–13. doi: 10.1111/j.1600-0765.2010.01329.x. [DOI] [PubMed] [Google Scholar]
- 29.Han G, Chen Y, Hou J, Liu C, Chen C, Zhuang J, et al. Effects of simvastatin on relapse and remodeling of periodontal tissues after tooth movement in rats. Am J Orthod Dentofacial Orthop. 2010;138:550.e1–7. doi: 10.1016/j.ajodo.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 30.Rutledge J, Schieber MD, Chamberlain JM, Byarlay M, Killeen AC, Giannini PJ. Simvastatin application to augment facial jaw bone in a dog model: Pilot study. J Periodontol. 2011;82:597–605. doi: 10.1902/jop.2010.100214. [DOI] [PubMed] [Google Scholar]
- 31.Calixto JC, Lima CE, Frederico L, Lima RP, Anbinder AL. The influence of local administration of simvastatin in calvarial bone healing in rats. J Craniomaxillofac Surg. 2011;39:215–20. doi: 10.1016/j.jcms.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 32.Kilic E, Ozeç I, Yeler H, Korkmaz A, Ayas B, Gumuş C. Effects of simvastatin on mandibular distraction osteogenesis. J Oral Maxillofac Surg. 2008;66:2233–8. doi: 10.1016/j.joms.2008.05.362. [DOI] [PubMed] [Google Scholar]
- 33.Morris MS, Lee Y, Lavin MT, Giannini PJ, Schmid MJ, Marx DB, Reinhardt RA. Injectable simvastatin in periodontal defects and alveolar ridges: Pilot studies. J Periodontol. 2008;79:1465–73. doi: 10.1902/jop.2008.070659. [DOI] [PubMed] [Google Scholar]
- 34.Seto H, Ohba H, Tokunaga K, Hama H, Horibe M, Nagata T. Topical administration of simvastatin recovers alveolar bone loss in rats. J Periodontal Res. 2008;43:261–7. doi: 10.1111/j.1600-0765.2007.01024.x. [DOI] [PubMed] [Google Scholar]
- 35.Moriyama Y, Ayukawa Y, Ogino Y, Atsuta I, Koyano K. Topical application of statin affects bone healing around implants. Clin Oral Implants Res. 2008;19:600–5. doi: 10.1111/j.1600-0501.2007.01508.x. [DOI] [PubMed] [Google Scholar]
- 36.Nishimura K. Local application of simvastatin to rat incisor sockets augments bone. Kokubyo Gakkai Zasshi. 2008;75:49–54. doi: 10.5357/koubyou.75.49. [DOI] [PubMed] [Google Scholar]
- 37.Chen YP, Han GH, Jin CW, Shi RX, Hou JH. Effect of simvastatin on bone morphogenetic protein-2 expression in the periodontal tissue after rat tooth movement. Zhonghua Kou Qiang Yi Xue Za Zhi. 2008;43:21–5. [PubMed] [Google Scholar]
- 38.Lee Y, Schmid MJ, Marx DB, Beatty MW, Cullen DM, Collins ME, et al. The effect of local simvastatin delivery strategies on mandibular bone formation in vivo. Biomaterials. 2008;29:1940–9. doi: 10.1016/j.biomaterials.2007.12.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wu Z, Liu C, Zang G, Sun H. The effect of simvastatin on remodelling of the alveolar bone following tooth extraction. Int J Oral Maxillofac Surg. 2008;37:170–6. doi: 10.1016/j.ijom.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 40.Wu Z, Sun HC, Liu ST, Wang Y. Effect of simvastatin on residual ridge resorption after tooth extraction. Zhonghua Kou Qiang Yi Xue Za Zhi. 2006;41:747–50. [PubMed] [Google Scholar]
- 41.Anbinder AL, Junqueira JC, Mancini MN, Balducci I, Rocha RF, Carvalho YR. Influence of simvastatin on bone regeneration of tibial defects and blood cholesterol level in rats. Braz Dent J. 2006;17:267–73. doi: 10.1590/s0103-64402006000400001. [DOI] [PubMed] [Google Scholar]
- 42.Stein D, Lee Y, Schmid MJ, Killpack B, Genrich MA, Narayana N, et al. Local simvastatin effects on mandibular bone growth and inflammation. J Periodontol. 2005;76:1861–70. doi: 10.1902/jop.2005.76.11.1861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ayukawa Y, Okamura A, Koyano K. Simvastatin promotes osteogenesis around titanium implants. Clin Oral Implants Res. 2004;15:346–50. doi: 10.1046/j.1600-0501.2003.01015.x. [DOI] [PubMed] [Google Scholar]
- 44.Junqueira JC, Mancini MN, Carvalho YR, Anbinder AL, Balducci I, Rocha RF. Effects of simvastatin on bone regeneration in the mandibles of ovariectomized rats and on blood cholesterol levels. J Oral Sci. 2002;44:117–24. doi: 10.2334/josnusd.44.117. [DOI] [PubMed] [Google Scholar]
- 45.Pradeep AR, Thorat MS. Clinical effect of subgingivally delivered simvastatin in the treatment of patients with chronic periodontitis: A randomized clinical trial. J Periodontol. 2010;81:214–22. doi: 10.1902/jop.2009.090429. [DOI] [PubMed] [Google Scholar]
- 46.Fajardo ME, Rocha ML, Sánchez-Marin FJ, Espinosa-Chávez EJ. Effect of atorvastatin on chronic periodontitis: A randomized pilot study. J Clin Periodontol. 2010;37:1016–22. doi: 10.1111/j.1600-051X.2010.01619.x. [DOI] [PubMed] [Google Scholar]
- 47.Saxlin T, Suominen-Taipale L, Knuuttila M, Alha P, Ylöstalo P. Dual effect of statin medication on the periodontium. J Clin Periodontol. 2009;36:997–1003. doi: 10.1111/j.1600-051X.2009.01484.x. [DOI] [PubMed] [Google Scholar]
- 48.Saver BG, Hujoel PP, Cunha-Cruz J, Maupomé G. Are statins associated with decreased tooth loss in chronic periodontitis? J Clin Periodontol. 2007;34:214–9. doi: 10.1111/j.1600-051X.2006.01046.x. [DOI] [PubMed] [Google Scholar]
- 49.Takeshita F, Morimoto K, Suetsugu T. Tissue reaction to alumina implants inserted into the tibiae of rats. J Biomed Mater Res. 1993;27:421–8. doi: 10.1002/jbm.820270402. [DOI] [PubMed] [Google Scholar]
- 50.The SEARCH Collaborative Group. Link E, Parish S, Armitage J, Bowman L, Heath S, et al. SLCO1B1 variants and statin-induced myopathy-A genomewide study. N Engl J Med. 2008;359:789–99. doi: 10.1056/NEJMoa0801936. [DOI] [PubMed] [Google Scholar]
- 51.Marcoff L, Thompson PD. The role of coenzyme Q10 in statin-associated myopathy: A systematic review. J Am Coll Cardiol. 2007;49:2231–7. doi: 10.1016/j.jacc.2007.02.049. [DOI] [PubMed] [Google Scholar]
- 52.Thompson PD, Clarkson P, Karas R. Statin-associated myopathy. JAMA. 2003;289:1681–90. doi: 10.1001/jama.289.13.1681. [DOI] [PubMed] [Google Scholar]
- 53.Graham DJ, Staffa JA, Shatin D, Andrade SE, Schech SD, La Grenade L, et al. Incidence of hospitalized rhabdomyolysis in patients treated with lipid-lowering drugs. JAMA. 2004;292:2585–90. doi: 10.1001/jama.292.21.2585. [DOI] [PubMed] [Google Scholar]
- 54.Pascual Cruz M, Chimenos KE, García JA, Mezquiriz FX, Borrell TE, Lopez LJ. Adverse side effects of statins in the oral cavity. Med Oral Patol Oral Cir Bucal. 2008;13:E98–101. [PubMed] [Google Scholar]


