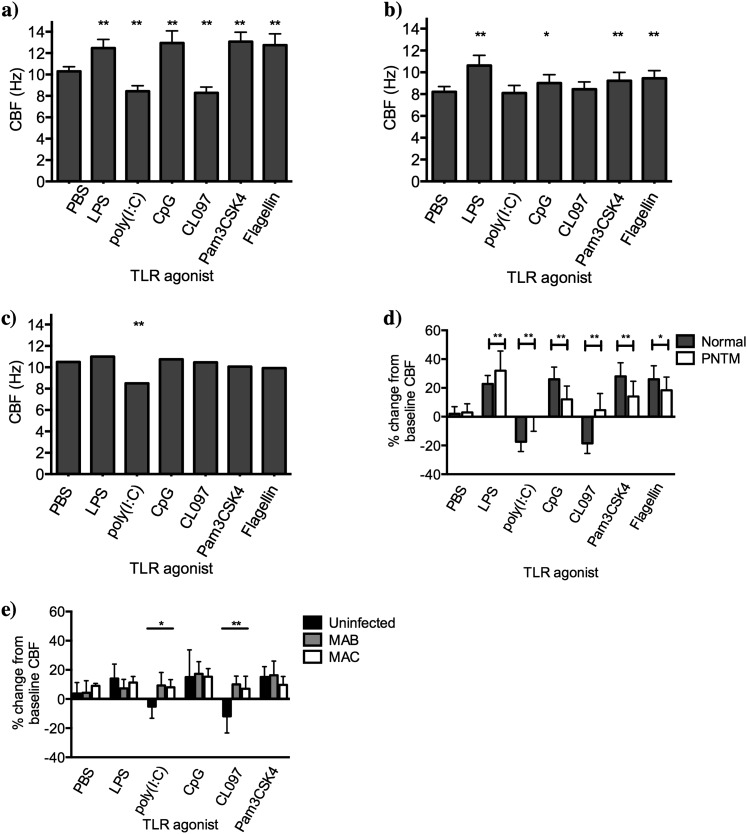
Figure 2.
Ciliary beat frequency (CBF) response to TLR agonists in day of collection (DOC) and air–liquid interface cultures. (a) Absolute CBF on DOC. Healthy control respiratory samples CBF was measured after 8 hours of exposure to no agonist (PBS; n = 10), Toll-like receptor (TLR4) (LPS; n = 9), TLR3 [poly(I:C); n = 12), TLR9 (CpG; n = 13), TLR7/8 (CL097; n = 11), TLR2 (Pam3CSK4; n = 12), and TLR5 (Flagellin; n = 10]. Healthy control subjects significantly increase CBF in response to the TLR4 (LPS), TLR9 (CpG), TLR2 (Pam3CSK4), and TLR5 (Flagellin) agonists; there is a significant decrease in CBF in response to the TLR3 [poly(I:C)] and the TLR7/8 (CL097) agonists (P < 0.0001 for all agonists, ANOVA). (b) Absolute CBF on DOC. Pulmonary nontuberculous mycobacteria (PNTM) respiratory samples CBF was measured after 8 hours of exposure to no agonist (PBS; n = 13), TLR4 (LPS; n = 20), TLR3 [poly(I:C); n = 18], TLR9 (CpG; n = 26), TLR7/8 (CL097; n = 22), TLR2 (Pam3CSK4; n = 22), and TLR5 (Flagellin; n = 11). Patients with PNTM have significant responses to the TLR4 (LPS), TLR9 (CpG), TLR2 (Pam3CSK4), and TLR5 (Flagellin) agonists (P < 0.0001, P < 0.009, P < 0.0006, P < 0.0005, respectively; ANOVA). (c) Absolute CBF on DOC. PNTM respiratory samples CBF was measured after 8 hours of exposure to no agonist (PBS), TLR4 (LPS), TLR3 [poly(I:C)], TLR9 (CpG), TLR7/8 (CL097), TLR2 (Pam3CSK4), and TLR5 (Flagellin) agonists. The TLR3 [poly(I:C)] agonist significantly decreased CBF (P < 0.002, ANOVA). (d) Percent change from preexposure baseline CBF for healthy control subjects and patients with PNTM exposed to 8 hours of TLR agonists TLR4 (LPS), TLR3 [poly(I:C)], TLR9 (CpG), TLR7/8 (CL097), TLR2 (Pam3CSK4), and TLR5 (Flagellin). PNTM were significantly different from healthy control subjects with respect to TLR2 (Pam3CSK4), TLR3 [poly(I:C)], TLR4 (LPS), TLR5 (Flagellin), TLR7/8 (CL097), and TLR9 (CpG) (P < 0.0006, P < 0.0001, P < 0.007, P < 0.03, P < 0.0001, P < 0.0001, respectively; two-tailed t test). (e) Comparison of normal human bronchial epithelial (NHBE) cultures’ response to TLR agonists in the presence of clinical concentrations of Mycobacterium abscessus (MAB) (n = 4), clinical concentrations of Mycobacterium avium (MAC) (n = 3), or uninfected (n = 9). NHBE cultures were infected (multiplicity of infection, 5:1) with MAB or MAC for 8 days before TLR stimulation. Data are expressed as percent change from preagonist CBF (uninfected or infected) to 8-hour post-TLR agonists: TLR4 (LPS), TLR3 [poly(I:C)], TLR9 (CpG), TLR7/8 (CL097), and TLR2 (Pam3CSK4). Significant change in response (i.e., reversal of response) was seen with poly(I:C) and CL097 (P < 0.01 and P < 0.005, respectively; ANOVA). Data are presented as means; error bars show SD. *P < 0.05; **P < 0.005.