Abstract
Background: Clozapine is the most effective antipsychotic in treatment-resistant schizophrenia but its use portends with a high burden of adverse reactions. One adverse event reported both in case reports and cross-sectional surveys is the emergence or worsening of obsessive compulsive symptoms (OCS).
Objectives: This study presents a retrospective review of a UK cohort of clozapine-treated individuals with the aim to further investigate the complex relationship between clozapine and OCS.
Methods: An extensive review of the medical records of 49 patients receiving clozapine in the Southampton area was undertaken. We searched for a diagnosis of obsessive compulsive disorder, signs or symptoms of obsessive compulsive disorder or the prescribing of selected antidepressants the year before clozapine initiation and the year after.
Results: Fifteen patients (31%) had reports of OCS during the 2-year data collection period. Twelve patients (24%) had OCS before clozapine initiation while only 7 (14%) had symptoms after clozapine was initiated. De novo OCS were reported in three (6%) cases after 5–9 months of clozapine treatment.
Conclusions: As with previous studies it was not possible to establish a definitive link between clozapine and OCS. Clinicians should be mindful of the common comorbidity of OCS and schizophrenia and the possible increased risk incurred when starting clozapine.
Keywords: atypical antipsychotic, clozapine, obsessive behaviour, obsessive compulsive symptoms, obsessive compulsive disorder, obsessive compulsive personality disorder
Introduction
Clozapine is more effective than other drugs in treatment-resistant schizophrenia [Kane et al. 1988]. Clozapine, however, is arguably the most toxic of all antipsychotics and requires particular precautions and monitoring. Why clozapine is more effective in refractory schizophrenia is unclear, however it has a diverse and unique pharmacology affecting multiple receptors which may in part explain its wide range of adverse effects. These include agranulocytosis, constipation, tachycardia, hypersalivation and metabolic changes such as weight gain, diabetes and hyperlipidaemia. Even with this considerable burden of adverse events clozapine remains an essential treatment choice in schizophrenia and in those with an enduring, recurrent illness clozapine probably represents their best hope for recovery. One adverse event occasionally reported in the clinical literature with clozapine is the emergence or unmasking of obsessive compulsive disorder (OCD) or related symptoms.
The formal diagnosis of OCD is characterized by the presence of either obsessions, compulsions or both. An obsession is an unwanted thought, image or urge which repeatedly enters the mind and are usually unpleasant. A compulsion is a repetitive behaviour or mental act the person is driven to perform. To meet the diagnosis of OCD these obsessive compulsive symptoms (OCS) must cause significant distress or interfere with daily functioning and not be better explained by another mental illness [National Institute for Health and Clinical Excellence, 2006].
The relationship between clozapine and worsening or developing OCS is complex. Both OCS and OCD are common in schizophrenia even in the absence of the use of antipsychotics. Between 10% and 64% of those with schizophrenia are reported to have OCS while 7.8% and 29.8% have comorbid OCD [Bottas et al. 2005; Nolfe et al. 2010]. In comparison the individual lifetime prevalence rate for OCD in the general population lies between 2% and 3% [National Institute for Health and Clinical Excellence, 2006]. Those with OCS and schizophrenia have more pronounced symptoms [Cunil et al. 2009], poorer social functioning, more motor symptoms [Nolfe et al. 2010] and a higher incidence of depression than seen in the individual illnesses [Cunil et al. 2009]. Some authors have suggested there may be enough evidence for a special category of schizophrenia coined as schizo-obsessive and that the two disorders are merely different expressions of the same disease [Bottas et al. 2005]. However, reports from the last three decades have revealed higher comorbidity rates of schizophrenia and OCD than recognized previously [Bottas et al. 2005; Nolfe et al. 2010] and this coincides with the increasing use of the second-generation antipsychotics which may be a contributing factor.
Many second-generation antipsychotics (olanzapine, risperidone and quetiapine) have rare reports of worsening or developing OCS [Lykouras et al. 2003]. Clozapine has the most reports with over 30 individual cases published. The first two cases appeared in 1992 a year after clozapine received a UK licence [Patil, 1992] and since then there has been a number of more extensive studies. There have been five previous retrospective chart reviews published which investigated the relationship between clozapine and OCD. Ertugrul and colleagues from Hacettepe University in Turkey presented their investigation as a short communication in 2005. They reviewed 50 patients receiving clozapine for emerging OCS and found 10 (20%) had new onset OCS which was not related to severity of illness, dose or duration of clozapine [Ertugrul et al. 2005]. In a letter by De Hann and colleagues, of 41 patients, 4 (9.1%) developed de novo OCD while on clozapine [De Haan et al. 2004]. In a further report by De Haan and colleagues, 7 (20.6%) of 32 patients receiving clozapine reported an increase in obsessions after clozapine was started [De Haan et al. 1999]. Both studies by De Hann and colleagues included patients receiving other antipsychotics besides clozapine. Ghaemia and colleagues randomly selected 142 clozapine patients and reviewed medical records before and after clozapine treatment. They searched for symptoms of OCS and a diagnosis of OCD. Of 142 patients, 41 had schizophrenia and 52 had schizoaffective disorder, the remainder had a wide variety of disorders. No one in the study developed de novo OCD after starting clozapine, but two (1.4%) experienced a moderate worsening of OCS symptoms [Ghaemia et al. 1995]. Baker and colleagues in 1992 investigated 49 chronic patients with schizophrenia and noted that 5 (10.2%) had developed either de novo or exacerbation of pre-existing OCS [Baker et al. 1992].
From the current limited literature it is not possible to infer the exact relationship between clozapine and OCS. The incidence of de novo OCS while on clozapine is reported to be between 3.5% and 28.4% [Mahendran et al. 2007; Lin et al. 2006] a range which includes in it the naturally occurring incidence of comorbid schizophrenia and OCS described above. Some have been unable to establish any relationship [Mukhopadhaya et al. 2009; Ghaemia et al. 1995] and a small case series suggested clozapine may be beneficial in specific subgroups of patients with OCS and schizophrenia [Reznik et al. 2004] although this is disputed by others [McDougle et al. 1995].
The majority of the literature suggests a tentative increased risk of OCS associated with clozapine, which is possibly more likely at higher doses. Reasons for a possible link between clozapine and OCS include a dopaminergic / serotoninergic imbalance, supersensitivity at 5-HT2C receptors, specific neuromorphological abnormalities [Nolfe et al. 2010] or alterations in serotonin metabolism [Ma et al. 2007].
This study provides a valuable addition to the current literature and, the authors believe, is the first UK retrospective study investigating clozapine and its possible relationship with OCS. A retrospective review was considered the most appropriate method because it was not reliant on patient or doctor time and enabled data collection to be carried out by one individual.
Methods
Study design
A project protocol and pilot data collection form were developed. Information obtained included age, sex, diagnosis, date of clozapine initiation, ethnicity and non-compliance after clozapine initiation. Three markers of OCS were chosen:
any record of an International Classification of Disease (ICD) or Diagnostic Statistical manual (DSM) diagnosis of OCD;
any record of the follow symptoms (obsessions, obsessional thoughts, ruminations, repetitive impulses, compulsions, repetitive thoughts or actions, repetitive behaviour or rituals);
any prescribing of a selective serotonin reuptake inhibitor (SSRI), venlafaxine or clomipramine.
ICD and DSM are the formal diagnostic classification systems used in psychiatry. The symptoms of OCD were adopted from the NICE OCD guidelines [National Institute for Health and Clinical Excellence, 2006]. Prescribing of an SSRI or clomipramine was taken from the NICE guidelines as the principal pharmaceutical treatment options. Venlafaxine was added to the antidepressant markers, as we considered it to be the most likely antidepressant prescribed for OCD if an SSRI or clomipramine were not appropriate. A positive answer to any of the questions prompted the investigator to collect further information on clozapine dose, duration, plasma level and concurrent medication. The pilot phase of the study included the first 10 patients reviewed. After this time, the data collection tool was adjusted for ease of use and clarity. Southampton and South West Hampshire Research Ethics Committee B granted ethics approval for the project on 10 May 2010 (REC number 09/H0504/132). This was followed by trust research approval on 18 May 2010. Consent was also obtained from local psychiatrists and team managers.
Patients
All patients currently registered for clozapine in the Southampton Area were eligible for the study. All patients were required to give written consent before their records were accessed. Those who refused to give their consent were excluded. Patients who were unable to understand the study or patient information were also excluded. Other exclusions were those prescribed clozapine for less then 1 year, anyone who was out of the Southampton area during the data collection period or where the relevant case notes were unobtainable despite extensive searching. Names of all patients receiving clozapine in the Southampton area were obtained by searching the Clozaril Patient Monitoring Service (CPMS) database. All patients receiving clozapine in Hampshire are required to register with the CPMS before initiating clozapine for ongoing monitoring. Clozapine is also categorized as a red drug in the local health economy, meaning all prescribing and supply is retained by secondary care. Patients identified were approached for consent either directly by the lead author or by nursing colleagues. A patient information leaflet was designed based on National Ethics Research service recommendations. This outlined the study and was given to patients when requested. For consenting participants all secondary care records were sought from 1 year before clozapine to 1 year after clozapine initiation. A thorough review was undertaken including all medical progress notes, admission summaries, discharge summaries, outpatient letters, medication charts, case conference reports, psychology reports and tribunal reports. Only nursing notes were excluded due to time constraints. Online GP records were also viewed during the same time period. A time period of 1 year before clozapine initiation was chosen to ensure enough time and opportunity was available for any OCS to be recognized and recorded. We also chose 1 year after clozapine initiation based on previous studies which suggested the average development of OCS on clozapine was between 5 and 6 months. Results were entered onto an Excel spreadsheet and analysed for trends and clinical significance.
Results
Eighty-five patients were approached for consent to take part in the study; of these, 14 refused consent and 10 were considered unable to understand the information. A total of 61 patients, therefore, were eligible for data collection. During the review it was discovered that seven of these were treated outside the area during the period of data collection and five sets of notes could not be traced. This left the total number of patients entering the study as 49 (Figure 1).
Figure 1.
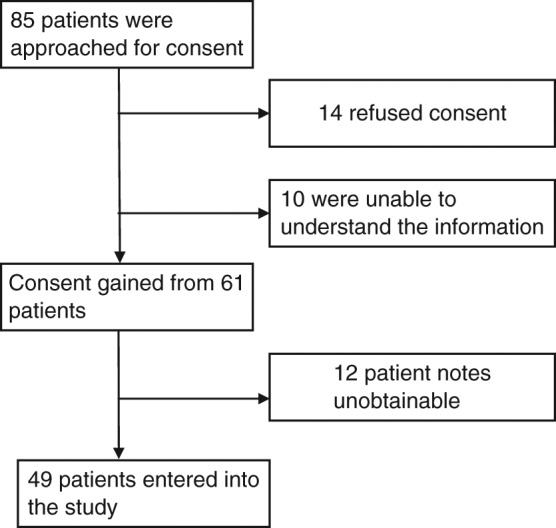
Data collection flow chart.
Demographic and clinical characteristics of the patients are presented in Table 1. A total of 69% of the study cohort were male, 94% were white and the average age of clozapine initiation was 34 years (age range 19–53). A total of 86% were diagnosed with treatment-resistant schizophrenia (see Table 1). No patient during the study had an ICD or DSM diagnosis of OCD. Fifteen patients (31%) had reports of OCS during the data collection period. Eight of these reported OCS only in the year before clozapine. Three patients appeared to have de novo OCS after starting clozapine and a further three had no change in OCS before or after clozapine. One patient’s OCS was reported to have improved after clozapine was initiated and there were no reports of worsening of pre-existing OCS after clozapine was prescribed (Figure 2). No significant difference was seen between those who reported OCS only before clozapine versus after clozapine (p = 0.57). Equally, there was no significant difference between the number of patients who were prescribed an antidepressant in the year before and year after cohorts (p = 0.59), see Table 2. In 81% of patients the primary diagnosis for prescribing an antidepressant was depression. In one patient the primary reason was to treat obsessions. One or more episodes of non-compliance of clozapine were reported in 17 patients (35%) in the year after starting clozapine.
Table 1.
Comparison of demographic and clinical characteristics of patients.
| Variable | Total study population (N = 49) | OCS reported before starting clozapine (N = 12) | OCS reported after starting clozapine (N = 7) |
|---|---|---|---|
| Sex | |||
| Men | 34 (69%) | 8 (67%) | 2 (29%) |
| Women | 15 (31%) | 4 (33%) | 5 (71%) |
| Age at clozapine initiation (mean) | 34 (19–53) | 37.5 (23–50) | 36 (24-48) |
| Ethnicity | White = 46 (94%) | White = 12 (100%) | White=7(100%) |
| Asian (non-Chinese) = 1 (2%) | |||
| Mixed race = 2 (4%) | |||
| Diagnosis | TR schizophrenia = 42 (86%) | TR schizophrenia = 9 (75%) | TR schizophrenia = 4 (57%) |
| Schizoaffective disorder = 2 (4%) | Schizoaffective disorder = 1 (8%) | Borderline PD = 2 (17%) | |
| Psychotic depressive disorder = 1 (2%) | Borderline PD = 1 (8%) | Mixed PD = 1 (14%) | |
| Borderline PD = 2 (4%) | Mixed PD = 1 (8%) | ||
| Mixed PD = 1 (2%) | |||
| Other = 1 (2%) | |||
OCS, obsessive compulsive symptoms; TR, treatment resistant; PD, personality disorder.
Figure 2.
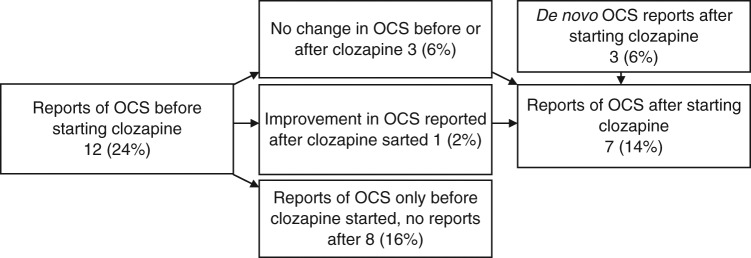
Changes in obsessive compulsive symptoms (OCS) during the year before and year after starting clozapine (n = 49).
Table 2.
Primary outcome measures: history of OCS before and after clozapine.
| Variable | Year before clozapine initiation (N = 49) | Year after clozapine initiation (N = 49) | p value (chi-squared, degrees of freedom) |
|---|---|---|---|
| Reports of OCS symptoms | 12 (24%) | 7 (14%) | 0.57 (0.316, 1) |
| Symptoms reported only before or after clozapine initiation. | 8 (16%) | 3 (6%) | 0.59 (0.287, 1) |
| Use of SSRI, venlafaxine or clomipramine | 25 (51%) | 23 (47%) | 0.77 (0.08, 1) |
SSRI, selective serotonin reuptake inhibitor.
Obsessions or ruminations were the most frequent symptoms reported in comorbid individuals (Table 3). Details of the patients who developed de novo OCS are given in Table 4. In general, they were initiated on clozapine at an early age, received a moderate dose of clozapine and developed OCS after many months of treatment.
Table 3.
Obsessive compulsive symptoms reported before and after clozapine initiation.
| Before clozapine initiation | Numbers of symptoms described = 21 (in 12 patients) |
|---|---|
| 10 × Obsessional symptoms 7 × Ruminations 3 × Repetitive thoughts 1 × Compulsions |
|
| After clozapine initiation | Number of symptoms described = 9 (in 7 patients) 7 × Obsessional symptoms 2 × Repetitive thoughts |
Table 4.
Details of patients who developed de novo OCS after starting clozapine.
| Patient number | 1 | 2 | 3 | Mean |
|---|---|---|---|---|
| Sex | M | F | F | - |
| Diagnosis | TR schizophrenia | Borderline PD | TR schizophrenia | - |
| Ethnicity | White | White | White | - |
| Age at clozapine initiation | 24 | 38 | 33 | 32 |
| Dose of clozapine at first onset of OCS (mg/day) | 550 | 400 | 500 | 483 |
| Most recent plasma level at time of OCS (mg/l) | 0.34 | 0.96 | 0.27 | 0.52 |
| Duration of clozapine before OCS reported | 5 months, 4 days | 8 months 17 days | 9 months 10 days | |
| Concurrent medication at the first report of OCS | Lithium Clonazepam | Salbutamol, Amitriptyline, Becotide, Montelucast, Levothyroxine, Docusate, Tolterodine, Hyoscine, Senna, Zuclopentixol acetate | Lithium, Quetiapine, Haloperidol, Omeprazole |
OCS, obsessive compulsive symptoms; TR, treatment resistant; PD, personality disorder
Discussion
This study failed to establish a definitive link between clozapine and OCS. Although this appears to be at odds with previous literature, two of the largest (n = 59 and n = 142) single-centre studies produced similar conclusions [Mukhopadhaya et al. 2009; Ghaemia et al. 1995]. Numerically, in our study, there were more reports of OCS in the year before clozapine was initiated than in the year after (24% versus 14%) and again this questions whether there is a direct link between clozapine causing OCS or if OCS is simply a common, late comorbidity of schizophrenia.
There are five previous retrospective chart reviews and these have varied in methodology and presentation making direct comparisons difficult. Two studies reported on patients recruited before 1995 when monitoring, dosing and experience of clozapine were limited and under development [Ghaemia et al. 1995; Baker et al. 1992]. Baker and colleagues reviewed 49 clozapine-treated patients with schizophrenia and identified 5 (10.2%) with de novo OCS or worsening OCS [Baker et al. 1992]. This could be considered similar to our result of 3 patients out of 49 (6%) developing de novo OCS. Details of how they conducted the review were not published, but the mean dose of those experiencing de novo symptoms was 650 mg for a mean duration of 7 months on clozapine. The three patients who developed de novo comorbidity in our study were receiving moderate to high doses of clozapine (mean dose 483 mg/day) and this concurs with Lin and colleagues who observed a higher incidence of OCS in patients on a higher dose of clozapine (mean dose 305.1 mg/day versus 268.9 mg/day) [Lin et al. 2006]. Although underreporting may account for the lower incidence of de novo OCS with clozapine observed in our study, it is similar to previous results. In the largest cross-sectional study to date [Mahendran et al. 2007] investigators actively interviewed patients using the Yale–Brown OCS checklist and uncovered an incidence of de novo OCS on clozapine of 3.5%. Ghaemia and colleagues published a large retrospective review (n = 142) and failed to establish a relationship between OCD symptoms and clozapine [Ghaemia et al. 1995]. In the latter study no patients experienced de novo OCS and only two (1.4%) experienced moderate worsening of OCS after clozapine was prescribed. This low incidence may in part be explained by the low dose (mean 291.2 mg/day), the inclusion of patients with other psychiatric disorders other than schizophrenia (29% of the total had schizophrenia) and perhaps an insufficient awareness of OCS in schizophrenia by treating physicians at that time. Although our study similarly failed to establish a definitive relationship, the majority of the cohort was diagnosed with schizophrenia (86%) and one would hope clinicians are now more familiar with the link between OCS and schizophrenia.
Of the remaining three retrospective chart reviews, one is published as a letter and the remaining two are published as short reports. In the letter by De Haan and colleagues, out of 41 patients on clozapine, 4 (9.8%) had OCD before clozapine and 4 (9.8%) developed de novo OCD [De Haan et al. 2004]. The four patients with pretreatment OCD all showed an improvement in symptoms after clozapine was initiated. This result is not dissimilar to that of our study where nine (18%) patients either experienced an improvement in symptoms or OCS was never recorded after clozapine was started. This would suggest that pre-existing OCS should not be considered as a contraindication for starting clozapine and in a subgroup of patients, comorbid OCS may improve or resolve. De Haan and colleagues also published a report in 1999 which predates their letter. In this report, 32 adolescents on clozapine were investigated for OCS. The average duration of clozapine treatment was 7.3 months and 7 patients (20.6%) reported an increase in obsessions after the start of clozapine. Five of these (16%) reported de novo OCS [De Hann et al. 1999]. This high percentage may suggest that younger patients are at higher risk of clozapine-induced OCS. Our study also showed a younger age of clozapine initiation in those who developed de novo OCS compared with the study population (mean 32 years versus 34 years) and suggests that the development of de novo OCS is a delayed adverse event with clozapine (between 5 and 9 months). This concurs with previous studies where a latent period before experiencing de novo OCS on clozapine is reported to be between 5 and 39 months. In the most recent chart review by Ertugrul and colleagues in 50 clozapine patients, 10 (20%) had new onset OCS while 9 (18%) had exacerbations of their pre-existing symptoms [Ertugrul et al. 2005].
Study limitations
This was a retrospective review conducted in a working clinical setting. There was no control group for comparison, reviews were not blind and data were collected entirely from reviewing the psychiatric and GP records. The handwriting in the psychiatric records was at times challenging but this was checked against typed letters and other printed documentation. Of particular note is the risk of underreporting of obsessive symptoms in the notes. This may be of particular concern before clozapine is initiated because many patients are mentally unwell and the focus of treatment is psychotic symptoms. Other acute symptoms may also have masked OCS which was then discovered when patients improved. In our study, however, more patients had OCS before clozapine was initiated so underreporting or masking of symptoms may have been less important. The study sample was largely white (96%) and male (69%) and this may prove a limitation if subsequent studies uncover an ethnicity or gender link in developing OCS with clozapine. Other limitations are the role of other medication and the time period chosen for the investigation. Medication was only recorded if the patient experienced de novo OCS or the listed antidepressants were found. Concurrent medication may have had an impact on comorbid symptoms. Finally, although the majority of previous studies reported the time for development of OCS is between 5 and 7 months this is by no means established. It is feasible to consider that future larger-scale prospective trials will suggest the development is beyond a year into clozapine treatment.
Implications for clinical practice
This is the first UK-based retrospective chart review into clozapine causing or worsening OCS. Combining this study with previous reports would suggest that there are four possible outcomes in the complex relationship between clozapine and OCS:
patients who have pre-exiting OCS may improve when clozapine is initiated;
patients with pre-existing symptoms may have no change in symptoms after clozapine initiation;
patients with pre-existing symptoms may see a worsening of symptoms when clozapine is started; and
de novo OCS may occur after many months of clozapine treatment.
Risk factors for developing de novo OCS identified from this and other studies point to a higher risk in younger patients and those who are on higher doses. This, however, would need replicating in large multicentre prospective trials to confirm.
Clinicians should be mindful of the link between obsessive compulsive symptomology and schizophrenia and the possible increased risk incurred when starting clozapine.
Extensive physical health checks are recommended before starting clozapine and periodically during treatment. Screening for OCS, using a formal rating scale, should become part of this routine health check.
Acknowledgments
The authors are grateful to Lindsey Stevens, Lynn Benham and the medicines management team at Southern Health NHS Foundation Trust for their support and assistance.
Footnotes
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
The authors have no conflicts of interest related to this study.
References
- Baker R.W., Changappa K.N., Baird J.W., Steingard S., Christ M., Schooler N. (1992) Emergence of obsessive compulsive symptoms during treatment with clozapine. J Clin Psychiatry 53: 439–442 [PubMed] [Google Scholar]
- Bottas A., Cooke R., Richter M. (2005) Comorbidity and pathophysiology of obsessive-compulsive disorder in schizophrenia: Is there evidence for a schizo-obsessive subtype of schizophrenia? J Psychiatr Neurosci 20: 187–193 [PMC free article] [PubMed] [Google Scholar]
- Cunil R., Castells X., Simeon D. (2009) Relationship between obsessive-compulsive symptomology of psychosis in schizophrenia: a systematic review and meta-analysis. J Clin Psychiatry 70: 70–82 [DOI] [PubMed] [Google Scholar]
- De Haan L., Oekeneva A., Van Amelsvoort T., Linszen D. (2004) Obsessive-compulsive disorder and treatment with clozapine in 200 patients with recent-onset schizophrenia or related disorders. Eur Psychiatry 19: 524. [DOI] [PubMed] [Google Scholar]
- De Hann L., Linszen D., Gorsira R. (1999) Clozapine and obsessions in patients with recent-onset schizophrenia and other psychotic disorders. J Clin Psychiatry 60: 364–365 [DOI] [PubMed] [Google Scholar]
- Ertugrul A., Yagcioglu E., Eni N., Yazici K. (2005) Obsessive-compulsive symptoms in clozapine-treated schizophrenia patients. Psychiat Clin Neuros 59: 219–222 [DOI] [PubMed] [Google Scholar]
- Ghaemi S., Zarate C., Popli A., Pillay S., Cole J. (1995) Is there a relationship between clozapine and obsessive-compulsive disorder? A retrospective chart review. Compr Psychiatr 36: 267–270 [DOI] [PubMed] [Google Scholar]
- Kane J., Honigfield G., Singer J., Meltzer H. (1998) Clozapine for treatment resistant schizophrenia- a double-blind comparison with chlorpromazine. Arch Gen Psychiatry 45: 789–796 [DOI] [PubMed] [Google Scholar]
- Lin S.K., Su S.F., Pan C.H. (2006) Higher plasma drug concentration in clozapine-treated schizophrenia patients with side effects of obsessive/compulsive symptoms. Ther Drug Monit 28: 303–307 [DOI] [PubMed] [Google Scholar]
- Lykouras L., Alevizos B., Michalopoulou P., Rabavilas A. (2003) Obsessive-compulsive symptoms induced by atypical antipsychotics. A review of the reported cases. Prog Neuro-Psychoph 27: 333–346 [DOI] [PubMed] [Google Scholar]
- Ma N., Tan L.-W., Wang Q., Li Z., Li L. (2007) Lower levels of whole blood serotonin in obsessive-compulsive disorder and in schizophrenia with obsessive-compulsive symptoms. Psychiat Res 150: 61–69 [DOI] [PubMed] [Google Scholar]
- Mahendran R., Liew E., Subramaniam M. (2007) De novo emergence of obsessive-compulsive symptoms with atypical antipsychotics in Asian patients with schizophrenia or schizoaffective disorder: a retrospective, cross-sectional study. J Clin Psychiatry 68: 542–545 [DOI] [PubMed] [Google Scholar]
- McDougle C.J., Barr L.C., Goodman W.K., Pelton G., Aranson S.C., Anand A., et al. (1995) Lack of efficacy of clozapine monotherapy in refractory obsessive-compulsive disorder. Am J Psychiatry 152: 1812–1814 [DOI] [PubMed] [Google Scholar]
- Mukhopadhaya K., Krishnaiah R., Taye T., Nigam A., Bailey A.J., Sivakumaran T., et al. (2009) Obsessive-compulsive disorder in UK clozapine-treated schizophrenia and schizoaffective disorder: a cause for clinical concern. J Psychopharmacol 23: 6–13 [DOI] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence (2006) Obsessive Compulsive Disorder. National Guideline 31. National Collaborating Centre for Mental Health http://www.nice.org.uk (accessed January 2011).
- Nolfe G., Milano W., Zontini G., Petrella C., De Rosa M., Rundle-Smith S., et al. (2010) Obsessive-compulsive symptoms in schizophrenia: Their relationship with clinical features and pharmacological treatment. J Psychiat Prac 16: 235–242 [DOI] [PubMed] [Google Scholar]
- Patil V.J. (1992) Development of transient obsessive-compulsive symptoms during treatment with clozapine. Am J Psychiatry 149: 272. [DOI] [PubMed] [Google Scholar]
- Reznik I., Yavin I., Stryjer R., Spivak B., Gonen N., Strous R., et al. (2004) Clozapine in the treatment of obsessive-compulsive symptoms in schizophrenia: a case series. Pharmacopsychiatry 37: 52–56 [DOI] [PubMed] [Google Scholar]


