Abstract
The purpose of this study was to analyze the effects of 2 days/week versus 4 days/week of Whole Body Vibration (WBV) during eight weeks of WBV training on health-related quality of life (SF-36), balance and lower body strength, as well as short-term detraining (3 weeks) on balance and lower body strength among older adults. Thirty-four older adults were randomly assigned to a control group (Control; n = 11) or to one of the vibration training groups: WBV 2 days/week (WBV_2d; n = 11) or WBV 4 days/week (WBV_4d; n = 12). The WBV groups exercised for 8 weeks, following 3 weeks of detraining. Lower body strength increased significantly (p < 0.05) for both groups, WBV_2d and WBV_4d, after 8-week training. A significant reduction in strength was observed following 3 weeks of detraining only in WBV_2d group (p < 0.05). All variables of the SF-36 and the balance test did not change after intervention in any group. 2 days/week and 4 days/week of WBV during 8 weeks showed the same improvements on muscle strength. 3 weeks of detraining did not reverse the gains in strength made during 32 sessions of WBV.
Key points.
2 days and 4 days per week of WBV training during 8 weeks showed the same improvements on muscle strength.
3 weeks of detraining did not reverse the gains in strength made during 32 sessions of WBV exercise.
3 weeks of detraining did reverse the gains in strength made during 16 sessions of WBV exercise.
Key words: Whole-body vibrations, posturography, dose-response, equilibrium
Introduction
The aging process is associated with loss of muscle mass, reduced strength, and impairment of physical functioning (Abellan Van Kan, 2009). Although some declines with age are inevitable, considerable evidence indicates that physically active older individuals maintain healthy functioning longer than their sedentary peers (Landi et al., 2007). Maintenance of muscular function into old age is critical to sustaining normal daily activity and functional independence (Reid et al., 2008). Moreover, poor balance is frequently associated with reduced muscle strength in community-dwelling older adults (Wolfson et al., 1995).
Conventional resistance training (CRT) is a preferred intervention to decrease the effects of sarcopenia, as CRT has been shown to induce muscle hypertrophy and enhance strength, power, and motor function (Hunter et al., 2004). Much research has been devoted to the development of muscular strength and older adults (Peterson et al., 2010) with various methods used to stimulate adaptations. CRT has involved the use of weights, weight- machines, body-weight, resistance bands, and other devices designed to provide mechanical resistance. However, whole-body vibration (WBV) training has gained considerable attention lately (Jordan et al., 2005). Published research on WBV training in older adults is increasing and available data seem to indicate changes in hormonal profile (Cardinale et al., 2010) and improvements on postural control (Bogaerts et al., 2007a; 2007b), mobility (Rees et al., 2007), balance (Cheung et al., 2007; Rees et al., 2008; 2009), muscle power (Marin et al., 2010a; Roelants et al., 2004) as well as muscle strength (Machado et al., 2010; Marin et al., 2010b).
For WBV, the dose-response relationship is vital to prescription on proper doses of training and optimizing the effort to benefit ratio. Over-prescription of WBV exercise may result in over-stress injuries, whereas under prescription will result in a failure to achieve the necessary or desired strength and balance improvements. According to a recent meta- analysis (Marin et al., 2010b) training volume appears to alter treatment effects with a general increase in strength adaptation as greater training volumes are employed. Maximum gains were measured with volumes around 12-15 minutes of vibration stimulus per training session. However, training frequency may be defined as the occurrence per unit of time (e.g., days per week), Marin and Rhea, 2010b reported that 3 days per week is the value that occurs the most frequently in studies analyzed (a total of 18 studies were included about chronic effects; elderly n = 7). However, more research is necessary to identify the effect of different training volumes and frequencies and the dose- response relationship for aged populations. Moreover, there is limited information on strength and balance changes after vibration training cessation.
To our knowledge, no previous studies have measured the effects of training frequency of WBV on muscle performance and balance in community-dwelling older adults. Thus, this study aimed to analyze the effects of two days/week versus four days/week of WBV during 8 weeks of WBV on health-related quality of life, balance and lower body strength, as well as short-term detraining (3 weeks) on balance and lower body strength.
Methods
Participants
Thirty-four community-dwelling older adults (18 women and 16 men; mean age: 84.3 ± 7.4 years) took part in this study. People suffering from epilepsy, gallstones, kidney stones, neuromuscular or neurodegenerative diseases, stroke, serious heart sicknesses or having an implant, bypass or stent were excluded. After participants were carefully informed about the design of the study, they signed a written informed consent before participation. All subjects were randomly assigned to a control group (Control; n = 11) or to one of the vibration training groups: WBV 2 days per week (WBV_2d; n = 11) or WBV 4 days per week (WBV_4d; n = 12). The control group did not participate in any training program, and these subjects were instructed not to change their lifestyle. Participants had no previous experience with WBV training or CRT. The study was approved by the University's Human Ethics Committee according to the declaration of Helsinki.
In the WBV groups, no subject reported any adverse side effects. Subjects generally reported a moderate degree of muscle fatigue at the end of each session. Thirty of the 34 subjects completed the study. Four (control = 1; WBV_2d = 1; WBV_4d = 2) subjects dropped out voluntarily in the first weeks of training because of conflicts in time between the test/training program and other life commitments. Hence, outcome data were obtained from the remaining 30 subjects (Figure 1).
Figure 1.
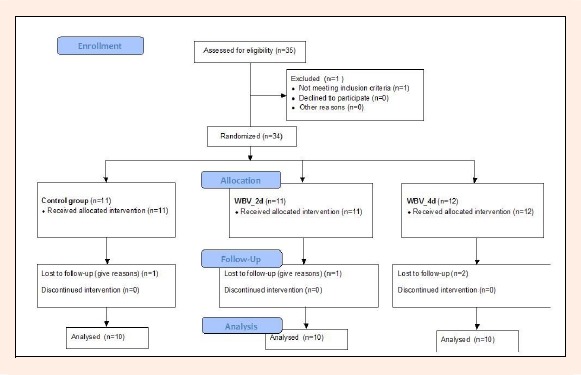
Flow diagram for randomized subject assignment in this study.
Vibration equipment
The vibration stimulus consisted of uniform vertical oscillations Power Plate® Next Generation (Power Plate North America, Northbrook, Illinois). The vertical component of the acceleration was measured using an accelerometer in accordance with ISO2954, (VM-6360, Hong Kong, China). Measured accelerations were from 20.44 m·s-2 (at 30 Hz and 1.05 mm [peak to peak]) to 63.8 m·s-2 (at 40 Hz and 2.11 mm [peak to peak]) with 70 kg on platform. During all sessions, subjects wore the same athletic shoes to standardize the damping of the vibration due to the footwear (Marin et al., 2009).
Intervention
The WBV groups exercised for 8 weeks on a vibration platform, following three weeks of detraining. The WBV training performed a lower-body-training program consisting of six different types of squats (Table 1). The order of exercises is shown in Table 1. Frequency of training (sessions/week) was different for each group, 2 and 4 sessions per week for WBV_2d and WBV_4d group, respectively. The training volume session was increased systematically over the 8 week training period by increasing the number of series of one exercise, or the number of different exercises (Table 1). The training intensity was increased by increasing the amplitude (1.05-2.11 mm) or the frequency (35-40 Hz) of the vibration (Table 1). Each WBV training session was preceded by a 10- min warm-up that included aerobic exercise and stretching.
Table 1.
Vibration exercise protocol.
| Week | Order of exercise | Duration (s) | Frequency (Hz) | Amplitude peak-to-peak (mm) | Rest (s) |
|---|---|---|---|---|---|
| 1 | a, a, a, b | 30 | 35 | 1.05 | 60 |
| 2 | a, c, a, a, a | 30 | 35 | 1.05 | 60 |
| 3 | a, d, c, a, a, a | 30 | 35 | 1.05 | 60 |
| 4 | a, f, d, c, a, a, e | 30 | 40 | 1.05 | 60 |
| 5 | a, f, d, c, a, a, e | 30 | 35 | 1.05 | 60 |
| 6 | a, f, d, c, a, a, e | 30 | 35 | 2.11 | 60 |
| 7 | a, f, f, d, c, a, a, e | 30 | 35 | 2.11 | 60 |
| 8 | a, f, f, d, c, a, a, e | 30 | 40 | 2.11 | 60 |
Exercise: a= squat (static -30º knee angle flexion-with grip); b= deep squat (static -60º knee angle flexion-with grip); c= alternating squat (dynamic, 3s each side -30º knee angle flexion-with grip); d= squat (static-without grip); e=squat (dynamic -with grip); f= squat+ bilateral biceps (static- hands in the straps).
Measurements
All groups were tested on three occasions, before training (pre-training, week 0), after the eight weeks of training (post-training, week 8), after three weeks of detraining (week 11). On the test day, subjects first completed a 10 minute warm-up, and then completed the balance and strength assessments. The health-related quality of life was measured one day before and one day after eight weeks of training.
Health-related quality of life (HrQoL)
HrQoL was assessed before training (pre-training, week 0), after the eight weeks of training (post-training, week8) using the SF-36 questionnaire (Ware et al., 1993). The Spanish version of the SF-36 is a validated instrument (Alonso et al., 1995), comprised of 36 questions assessing physical and mental health domains: 1) physical functioning scale that captures abilities to deal with the physical requirement of life, such as walking and flexibility; 2) role-physical evaluates the extent to which physical capabilities limit activity; 3) bodily pain scale evaluates the perceived amount of pain experienced during the previous 4 weeks; 4) general health scale evaluates general health in terms of personal perception; 5) vitality scale evaluates feelings of energy and fatigue; 6) social functioning scale evaluates how physical health and emotional problems interfered with social interactions during the previous 4 weeks; 7) role-emotional reflects the extent to which emotional factors interfere with activities; 8) mental health evaluates feelings of anxiety and depression. All eight scales are assessed quantitatively and scores between 0 and 100 are calculated, with a higher score indicating better health status.
Balance assessment
In order to assess balance, a Romberg test (standing with the eyes closed) (Fabunmi, et al., 2008) was carried out by all subjects (week 0, week 8 and week 11). Variations concerning the position of the centre of pressure were sampled at 100 Hz using a force plate system (ATMI Inc., Watertown, MA, USA). These variations were analyzed through, mediolateral (ML) dispersion (mm), anteroposterior (AP) dispersion (mm), displacement area (mm2), and mean velocity (m·s-1). The test was carried out with subjects standing on the force platform, with their heels together and toes spread lightly apart, in a comfortable position. The body was kept upright, with arms along the sides of the body. Subjects were asked to stand as still as possible for 30 s. If any type of external perturbation occurred during the test, the sample was discarded and another one was recorded.
Strength assessment
The chair stand test assesses lower body strength in older populations. Each subject completed two practice repetitions and one 30 seconds test trial. The score was the total number of stands executed correctly within 30 seconds. The test was administered in accordance with the protocol described by Riki and Jones (1999).
Statistical analysis
All analyses were conducted using the SPSS for Windows software, Version 17.0 (SPSS Inc., Chicago, IL, USA), and statistical significance level was set at p <0.05. All measures were normally distributed, as determined by the Shapiro-Wilks test. One-way analysis of variance (ANOVA) was used to test for differences between the groups at baseline. The changes over time in all dependent variables were analyzed by repeated-measures ANOVA. When a significant F-value was achieved, pair-wise comparisons were performed using a Tukey post-hoc procedure. From the two familiarization trials, intra-class correlation coefficients were calculated for each dependent variable to determine test-retest reliability, obtaining values always greater than 0.91. Values are expressed as mean ± SEM.
Results
The 30-s chair stand performance increased significantly (p < 0.05) for both groups, WBV_2d and WBV_4d, after 8-week training (Figure 2). There was a significant reduction (p < 0.05) after the 3-week detraining period for 30-s chair stand performance only in the WBV_2d group.
Figure 2.
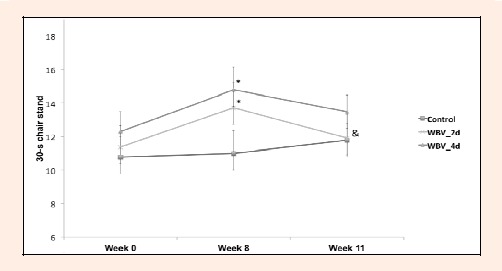
30-s chair stand (number of stands). * p < 0.05: significanty different from week 0. & p < 0.05: significantly different from week 8 (same group).
All variables of the SF-36 and the Romberg test did not change after intervention in any group (Table 2 and Table 3).
Table 2.
SF36 descriptive data. Data are means (±SEM).
| Pre-Training | Post-Training | ||
|---|---|---|---|
| PF | Control | 56.8 (8.6) | 50.5 (7.8) |
| WBV_2d | 43.6 (8.3) | 47.7 (10.5) | |
| WBV_4d | 64.0 (6.1) | 73.5 (7.2) | |
| RP | Control | 54.6 (13.4) | 61.4 (13.2) |
| WBV_2d | 59.1 (11.3) | 61.4 (11.4) | |
| WBV_4d | 82.5 (11.8) | 77.5 (12.1) | |
| BP | Control | 48.6 (7.8) | 59.5 (8.5) |
| WBV_2d | 58.4 (8.1) | 59.6 (7.9) | |
| WBV_4d | 67.7 (7.2) | 63.6 (6.1 | |
| GH | Control | 48.5 (6.8) | 34.1 (6.1) |
| WBV_2d | 55.3 (3.8) | 54.2 (3.6) | |
| WBV_4d | 55.6 (5.9) | 58.5 (8.3) | |
| VT | Control | 44.2 (7.2) | 47.9 (9.3) |
| WBV_2d | 49.6 (3.3) | 51.1 (7.1) | |
| WBV_4d | 65.2 (4.9) | 66.7 (8.0) | |
| SF | Control | 76.1 (6.2) | 63.6 (8.0) |
| WBV_2d | 61.4 (4.9) | 64.8 (7.9) | |
| WBV_4d | 76.3 (5.7) | 75.0 (6.5) | |
| RE | Control | 48.5 (15.2) | 48.5 (13.8) |
| WBV_2d | 42.4 (15.0) | 57.6 (11.1) | |
| WBV_4d | 76.7 (13.2) | 63.3 (10.5) | |
| MH | Control | 47.9 (8.2) | 49.6 (7.1) |
| WBV_2d | 56.4 (5.7) | 52.3 (7.4) | |
| WBV_4d | 69.6 (5.4) | 71.9 (7.4) | |
| PCS | Control | 41.8 (2.3) | 40.5 (2.2) |
| WBV_2d | 41.4 (3.5) | 41.7 (2.7) | |
| WBV_4d | 44.6 (2.1) | 46.4 (2.7) | |
| MCS | Control | 38.3 (4.1) | 37.8 (4.2) |
| WBV_2d | 38.6 (3.5) | 40.2 (4.0) | |
| WBV_4d | 48.0 (3.6) | 45.8 (4.1) |
PF: physical function, RP: role- physical, BP: bodily pain, GH: general health, VT: vitality, SF: social functioning, RE: role emotional, MH: mental health, PCS: Physical, MCS: Mental. Pre- Training (week 0); Post-Training (week 8).
Table 3.
Romberg test descriptive data.Data are means (±SEM).
| Week 0 | Week 8 | Week 11 | ||
|---|---|---|---|---|
| ML Dispersion (mm) | Control | .94 (.26) | .98 (.27) | 1.93 (.63) |
| WBV_2d | .98 (.17) | .82 (.21) | 1.26 (.20) | |
| WBV_4d | .87 (.20) | 1.40 (.27) | 1.27 (.40) | |
| AP Dispersion (mm) | Control | 2.73 (.60) | 2.39 (.38) | 2.15 (.38) |
| WBV_2d | 1.87 (.40) | 1.32 (.35) | 2.47 (.73) | |
| WBV_4d | 2.31 (.40 | 1.86 (.38) | 1.95 (.44) | |
| Displacement area (mm2) | Control | 55.91 (5.88) | 59.44 (4.27) | 45.58 (5.15) |
| WBV_2d | 57.22 (5.57) | 46.30 (3.65) | 49.63 (4.66) | |
| WBV_4d | 53.13 (7.48) | 44.38 (4.25) | 47.10 (4.83) | |
| Mean velocity (m·s-1) | Control | 3.08 (.37) | 3.15 (.22) | 3.03 (.55) |
| WBV_2d | 2.86 (.28) | 2.93 (.48) | 2.85 (.42) | |
| WBV_4d | 2.66 (.37) | 2.22 (.21) | 2.35 (.24) |
Discussion
To our knowledge, this is the first study to quantitatively evaluate the effects of two versus four days/week of WBV on HrQoL, balance and lower body strength, as well as short-term detraining effects (3 weeks) on balance and lower body strength.
The major finding of this study was that 4 days per week was equally effective when compared to 2 sessions per week in improving strength in community-dwelling older adults. However, in WBV_2d group performance in chair stand test was significantly lower after 3 weeks of detraining than at the end of the 8 weeks training program. These findings bear clinical significance, considering the exaggerated strength decline that occurs among sedentary individuals after the age of 50 years (Lynch et al., 1999). Four days of training appears to create a greater enhancement of strength when considering long-term improvements from WBV exercise.
In the present study, 8 week of WBV programs (4 and 2 days per week) with the use of a vertical vibration platform did not show any improvement of balance. In this sense, studies of 4 and 8-months employing the same vibration platform as in the present study, reported data similar to ours (Torvinen et al., 2002; 2003). In contrast, 6 week WBV programs with the use of a reciprocating vibration plate 3 days per week may reduce the decline in balance in the elderly (Bautmans et al., 2005; Gusi et al., 2006). According to Gusi and colleagues (2006) this difference between platforms (vertical vs. Reciprocating) could be explained in several ways: 1) the balance of lower limbs declines with age, particularly in the lateral direction (Mille et al., 2005), the direction in which the reciprocating plate has shown greater mechanical acceleration; 2) the studies differed in the frequency and amplitude used, as well as the methodology of balance assessment. Consequently, further research is required to determine the adequate dose-response of vibration needed to improve balance with consideration of different WBV platforms utilized.
In the present study, the use of the selected vibration frequencies as well as the progressive increase in frequency were done according to Marín et al. (2010a) have shown that the mean overall training frequencies of 35-40 Hz were most appropriate on vertical platforms, like used this study. Furthermore, the same authors described that alteration in that prescription throughout a chronic training program is vital to fully achieve the benefits of WBV.
Although previous investigations reported that strength is maintained after 5-27 weeks in the elderly (Hakkinen et al., 2000; Ivey et al., 2000; Sforzo et al., 1995), little is known about the effects of WBV on the magnitude and rate of strength loss during detraining.
On the other hand, in the present study, lower extremity strength decreased after 3 weeks of detraining but in WBV_4d group the values remained significantly higher than those before training, a finding that is consistent with previous studies of elderly individuals (Elliott et al., 2002; Sforzo et al., 1995). In contrast, our finding that strength reverted to the pre-training values in WBV_2d group after two weeks of detraining, a 13% loss of strength after 2 weeks of detraining. Fiatarone and colleagues (1990) reported a 32% loss of strength after 4 weeks of detraining in seven frail elderly subjects who had previously shown dramatic gains in strength after eight weeks of conventional strength training. In contrast, these data oppose other reports showing maintenance of training induced increases in muscular strength after 24 weeks (Hakkinen et al., 2000) and 31 weeks (Ivey et al., 2000) of detraining in older men.
The current investigation appears to suggest that, while 2 days per week is sufficient to begin to stimulate strength improvements, those adaptations diminish more rapidly than when WBV is conducted 4 days per week. Additional physiological testing and evaluation would be needed to verify and examine the detraining issue; however, these data may suggest that a greater training frequency is needed to stimulate longer lasting strength improvements.
SF-36 scores did not change during this study, neither control nor experimental groups. Two studies found significant improvements in 8 of 9 items (Bruyere et al., 2005) and in all scores (Furness et al., 2009) from the SF-36 after 6 weeks of vibration training. The absence of significant differences in SF-36 in our study could be given by the used training protocol.
Conclusion
Two days/week and 4 days/week of WBV training during 8 weeks showed the same improvements on muscle strength. Three weeks of detraining did not reverse the gains in strength made during 32 sessions of WBV exercise (4 per week during 8 weeks). However, three weeks of detraining did reverse the gains in strength made during 16 sessions of WBV exercise (2 per week during 8 weeks). It is plausible to hypothesize that 4 days per week is more beneficial than 2 days per week for long lasting positive adaptations of functional status in the elderly.
Acknowledgments
We thank Dr. Matthew Rhea for research assistance; also we thank Edzard Zeinstra and Power Plate International for their kindly assistance with vibration platform. The authors have no financial or personal conflicts of interest.
Biographies
Pedro J. Marín
Employement
Associate Professor, Laboratory of Physiology, European University Miguel de Cervantes, Valladolid, Spain. ResearchCenter on Physical Disability, ASPAYM Castilla y León, Spain.
Degree
PT, PhD
Research interests
Vibration training, resistance training and exercise physiology.
E-mail: pjmarin@uemc.es
Aurora Martín-López
Employement
Physiotherapist, Residence of the Third Age "Grupo Los Nogales - Santa Eugenia".
Degree
MSc
Research interests
Physical activity epidemiology and preventive medicine.
E-mail: martinlopez.a@gmail.com
Davinia Vicente-Campos
Employement
Associate Professor, School of Nursing, Complutense University of Madrid, Spain. University Francisco de Vitoria, Madrid, Spain.
Degree
PhD
Research interests
Sports science, and health promotion.
E-mail: davi_vic@hotmail.com
MT Angulo-Carrere
Employement
Associate Professor, Schoolof Nursing, Complutense University of Madrid, Spain.
Degree
MSc
Research interests
Biomechanics and sport science
E-mail: anguloca@enf.ucm.es
Teresa García-Pastor
Employement
Associate Professor, University Camilo José Cela, Madrid, Spain
Degree
MSc
Research interests
Biomechanics and sport science
E-mail: teresagarciap@yahoo.es
Nuria Garatachea
Employement
Associate Professor, Faculty of Health and Sport Science, University of Zaragoza, Spain.
Degree
PhD
Research interests
Physical activity and health as well as aging
E-mail: nugarata@unizar.es
José L. Chicharro
Employement
Professor, School of Nursing, Complutense University of Madrid, Spain
Degree
MD, PhD
Research interests
Exercise physiology.
E-mail: jlchicharro@enf.ucm.es
References
- Abellan Van Kan G. (2009) Epidemiology and consequences of sarcopenia. The Journal of Nutrition, Health & Aging 13, 708-712 [DOI] [PubMed] [Google Scholar]
- Alonso J., Prieto L., Anto J.M. (1995) [The Spanish version of the SF-36 Health Survey (the SF-36 health questionnaire): an instrument for measuring clinical results]. Medicina Clínica 104, 771-776 [PubMed] [Google Scholar]
- Bautmans I., Van Hees E., Lemper J.C., Mets T. (2005) The feasibility of Whole Body Vibration in institutionalised elderly persons and its influence on muscle performance, balance and mobility: a randomised controlled trial [ISRCTN62535013]. BMC Geriatrics 5, 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bogaerts A., Delecluse C., Claessens A. L., Coudyzer W., Boonen S., Verschueren S.M. (2007a) Impact of whole-body vibration training versus fitness training on muscle strength and muscle mass in older men: a 1-year randomized controlled trial. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 662, 630-635 [DOI] [PubMed] [Google Scholar]
- Bogaerts A., Verschueren S., Delecluse C., Claessens A. L., Boonen S. (2007b) Effects of whole body vibration training on postural control in older individuals: a 1 year randomized controlled trial. Gait Posture 26, 309-316 [DOI] [PubMed] [Google Scholar]
- Bruyere O., Wuidart M.A., Di Palma E., Gourlay M., Ethgen O., Richy F., Reginster J.Y. (2005) Controlled whole body vibration to decrease fall risk and improve health-related quality of life of nursing home residents. Archives of Physical Medicine and Rehabilitation 886, 303-307 [DOI] [PubMed] [Google Scholar]
- Cardinale M., Soiza R.L., Leiper J. B., Gibson A., Primrose W.R. (2010) Hormonal responses to a single session of wholebody vibration exercise in older individuals. British Journal of Sports Medicine 44, 284-288 [DOI] [PubMed] [Google Scholar]
- Cheung W.H., Mok H.W., Qin L., Sze P.C., Lee K.M., Leung K.S. (2007) High-frequency whole-body vibration improves balancing ability in elderly women. Archives of Physical Medicine and Rehabilitation 88, 852-857 [DOI] [PubMed] [Google Scholar]
- Elliott K.J., Sale C., Cable N.T. (2002) Effects of resistance training and detraining on muscle strength and blood lipid profiles in postmenopausal women. British Journal of Sports Medicine 36, 340-344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fabunmi A.A., Gbiri C.A. (2008) Relationship between balance performance in the elderly and some anthropometric variables. African Journal of Medicine and Medical Science 37, 321-326 [PubMed] [Google Scholar]
- Fiatarone M.A., Marks E.C., Ryan N.D., Meredith C.N., Lipsitz L.A., Evans W.J. (1990) High-intensity strength training in nonagenarians. Effects on skeletal muscle. JAMA: The Journal of the American Medical Association 263, 3029-3034 [PubMed] [Google Scholar]
- Furness T.P., Maschette W.E. (2009) Influence of whole body vibration platform frequency on neuromuscular performance of community-dwelling older adults. Journal of Strength and Conditioning Research 23, 1508-1513 [DOI] [PubMed] [Google Scholar]
- Gusi N., Raimundo A., Leal A. (2006) Low-frequency vibratory exercise reduces the risk of bone fracture more than walking: a randomized controlled trial. BMC Musculoskeletal Disorders 7, 92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hakkinen K., Alen M., Kallinen M., Newton R.U., Kraemer W.J. (2000) Neuromuscular adaptation during prolonged strength training, detraining and re-strength-training in middle-aged and elderly people. European Journal of Applied Physiology 883, 51-62 [DOI] [PubMed] [Google Scholar]
- Hunter G.R., Mccarthy J.P., Bamman M.M. (2004) Effects of resistance training on older adults. Sports Medicine 334, 329-348 [DOI] [PubMed] [Google Scholar]
- Ivey F.M., Tracy B.L., Lemmer J.T., Nessaiver M., Metter E.J., Fozard J.L., Hurley B.F. (2000) Effects of strength training and detraining on muscle quality: age and gender comparisons. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 555, B152-157; discussion B158-159 [DOI] [PubMed] [Google Scholar]
- Jordan M.J., Norris S.R., Smith D.J., Herzog W. (2005) Vibration training: an overview of the area, training consequences, and future considerations. Journal of Strength and Conditioning Research 119, 459-466 [DOI] [PubMed] [Google Scholar]
- Landi F., Onder G., Carpenter I., Cesari M., Soldato M., Bernabei R. (2007) Physical activity prevented functional decline among frail community-living elderly subjects in an international observational study. Journal of Clinical Epidemiology 660, 518-524 [DOI] [PubMed] [Google Scholar]
- Lynch N.A., Metter E.J., Lindle R.S., Fozard J.L., Tobin J.D., Roy T.A., Fleg J.L., Hurley B.F. (1999) Muscle quality. I. Age-associated differences between arm and leg muscle groups. Journal of Applied Physiology 886, 188-194 [DOI] [PubMed] [Google Scholar]
- Machado A., Garcia-Lopez D., Gonzalez-Gallego J., Garatachea N. (2010) Whole-body vibration training increases muscle strength and mass in older women: a randomized-controlled trial. Scandinavian Journal of Medicine & Science in Sports 220, 200-207 [DOI] [PubMed] [Google Scholar]
- Marin P.J., Bunker D., Rhea M.R., Ayllon F.N. (2009) Neuromuscular activity during whole-body vibration of different amplitudes and footwear conditions: implications for prescription of vibratory stimulation. Journal of Strength and Conditioning Research 223, 2311-2316 [DOI] [PubMed] [Google Scholar]
- Marin P.J., Rhea M.R. (2010a) Effects of vibration training on muscle power: a meta-analysis. Journal of Strength and Conditioning Research 224, 871-878 [DOI] [PubMed] [Google Scholar]
- Marin P.J., Rhea M.R. (2010b) Effects of vibration training on muscle strength: a meta-analysis. Journal of Strength and Conditioning Research 224, 548-556 [DOI] [PubMed] [Google Scholar]
- Mille M.L., Johnson M.E., Martinez K.M., Rogers M.W. (2005) Age-dependent differences in lateral balance recovery through protective stepping. Clinical Biomechanics (Bristol, Avon) 220, 607-616 [DOI] [PubMed] [Google Scholar]
- Peterson M.D., Rhea M.R., Sen A., Gordon P.M. (2010) Resistance exercise for muscular strength in older adults: a meta-analysis. Ageing Research Reviews 99, 226-237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rees S., Murphy A., Watsford M. (2007) Effects of vibration exercise on muscle performance and mobility in an older population. Journal of Aging and Physical Activity 115, 367-381 [DOI] [PubMed] [Google Scholar]
- Rees S.S., Murphy A.J., Watsford M.L. (2008) Effects of whole-body vibration exercise on lower-extremity muscle strength and power in an older population: a randomized clinical trial. Physical Therapy 888, 462-470 [DOI] [PubMed] [Google Scholar]
- Rees S.S., Murphy A.J., Watsford M.L. (2009) Effects of whole body vibration on postural steadiness in an older population. Journal of Science and Medicine in Sport 112, 440-444 [DOI] [PubMed] [Google Scholar]
- Reid K.F., Naumova E.N., Carabello R.J., Phillips E.M., Fielding R.A. (2008) Lower extremity muscle mass predicts functional performance in mobility-limited elders. The Journal of Nutrition, Health & Aging 112, 493-498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rikli R.E., Jones C.J. (1999) Development and validation of a functional fitness test for community-residing older adults. Journal of Aging and Physical Activity 77, 129-161 [Google Scholar]
- Roelants M., Delecluse C., Verschueren S.M. (2004) Whole-body-vibration training increases knee-extension strength and speed of movement in older women. Journal of the American Geriatrics Society 552, 901-908 [DOI] [PubMed] [Google Scholar]
- Sforzo G.A., Mcmanis B.G., Black D., Luniewski D., Scriber K. C. (1995) Resilience to exercise detraining in healthy older adults. Journal of the American Geriatrics Society 443, 209-215 [DOI] [PubMed] [Google Scholar]
- Torvinen S., Kannus P., Sievanen H., Jarvinen T. A., Pasanen M., Kontulainen S., Jarvinen T.L., Jarvinen M., Oja P., Vuori I. (2002) Effect of four-month vertical whole body vibration on performance and balance. Medicine and Science in Sports and Exercise 334, 1523-1528 [DOI] [PubMed] [Google Scholar]
- Torvinen S., Kannus P., Sievanen H., Jarvinen T.A., Pasanen M., Kontulainen S., Nenonen A., Jarvinen T.L., Paakkala T., Jarvinen M., Vuori I. (2003) Effect of 8-month vertical whole body vibration on bone, muscle performance, and body balance: a randomized controlled study. Journal of Bone and Mineral Research 118, 876-884 [DOI] [PubMed] [Google Scholar]
- Ware J.E., Snow K.K., Kosinski M., Gandek B. (1993). SF-36 Health Survey Manual and Interpretation Guide. (New England Medical Center, The Health Institute,, Boston). [Google Scholar]
- Wolfson L., Judge J., Whipple R., King M. (1995) Strength is a major factor in balance, gait, and the occurrence of falls. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences 550, 64-67 [DOI] [PubMed] [Google Scholar]


