Fig. 10.
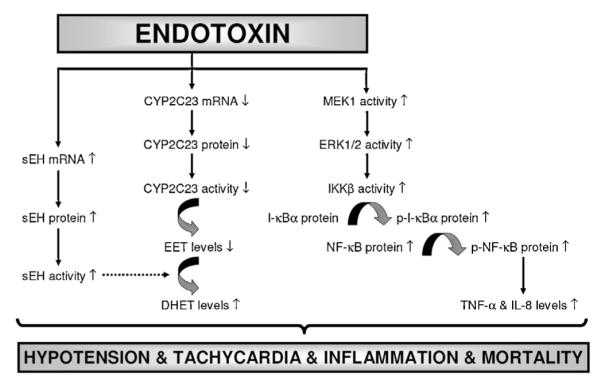
Schematic diagram showing the involvement of sEH, CYP2C23, MEK1/ERK1/2/IKKβ/IκB-α/NF-κB pathway, and proinflammatory cytokine production in endotoxin-induced hypotension, tachycardia, inflammation, and survival based on the current study. Endotoxin, the lipid A part of LPS which is the most potent microbial mediator of the pathogenesis of sepsis and septic shock, induces sEH expression and activity associated with decreased expression and activity of CYP2C23. In addition, endotoxin increases activity of MEK1/ERK1/2/IKKβ/IκB-α/NF-κB pathway associated with proinflammatory cytokine production leading to hypotension, tachycardia, inflammation, and mortality in the rodent model of septic shock. 5,14-HEDGE prevents the effects of endotoxin on the increase in expression and/or activity of sEH, MEK1, ERK1/2, IKKβ, IκB-α, and NF-κB associated with proinflammatory mediator production, and thus, restores blood pressure, prevents tachycardia and proinflammatory mediator formation, and improves survival during rodent endotoxemia. It should be noted that a competitive antagonist of vasoconstrictor effects of 20-HETE, 20-HEDE, prevents the effects of 5,14-HEDGE on blood pressure and HR associated with expression and/or activity of sEH, CYP2C23, and ERK1/2 as well as TNF-α and IL-8 levels in rats treated with LPS. It can be concluded that decreased expression and/or activity of sEH and MEK1/ERK1/2/IKKβ/IκB-α/NF-κB pathway as well as proinflammatory cytokine production associated with increased CYP2C23 expression and antiinflammatory mediator formation (e.g., EETs) participate in the protective effect of 5,14-HEDGE against hypotension, tachycardia, inflammation, and mortality in the rodent model of septic shock. ( ) stimulation; (
) stimulation; ( ) inhibition.
) inhibition.
