Figure 1. Possible scenarios of epilepsy surgery.
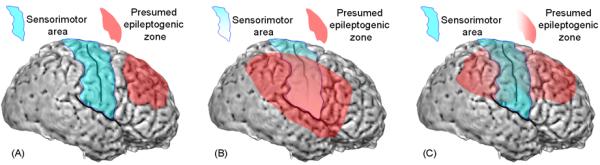
(A) The illustration shows a case in which the presumed epileptogenic zone (red) is localized to a region distant from eloquent cortex (blue). The primary intent of a surgeon would be to maximize removal of the presumed epileptogenic zone while preserving eloquent cortex. The symptomatogenic zone is dependent on the propagation pattern of ictal discharges. The sensorimotor cortex here may be considered as the symptomatogenic zone if the propagation of ictal discharges to it resulted in seizure-related symptoms characterized by jerking of the contralateral body.
(B) The illustration shows a case in which the presumed epileptogenic zone involves a large portion of eloquent cortex also serving as the symptomatogenic zone. The surgeon's intent would be to remove the symptomatogenic zone together with the presumed epileptogenic zone; for example, hemispherectomy including the sensorimotor area is a likely approach. The resulting functional losses due to hemispherectomy would include visual field loss, if the function was intact preoperatively, and a variable degree of enhancement in sensorimotor deficits.
(C) The illustration shows a case in which the presumed epileptogenic zone involves, to a lesser degree, eloquent cortex. This scenario is the case, for example, when the seizure onset zone is localized outside of eloquent cortex but very frequent interictal spike-wave discharges involve the eloquent cortex. One approach would be partial removal of the presumed epileptogenic zone along with maximal preservation of the eloquent cortex. An alternative approach would be maximal removal of the presumed epileptogenic zone together with eloquent cortex (serving as the symptomatogenic zone). With the later approach, a greater chance of seizure-freedom is plausible since resection includes the symptomatogenic zone responsible for generating the ictal symptom; the drawback of this more aggressive approach is a greater chance of development of a new or further enhancement of an existing functional deficit.
