Abstract
Maxilla is one of the facial bones with rich vascular supply. Necrosis of maxillary bone is rare and may occur due to infection, trauma and rare metabolic disorders. Maxilla is essential bone forming the roof of oral cavity. Mucormycosis is one of the most common fungal infection, which affects maxilla especially in diabetes and immunocompromised patients. We report a case of maxillary necrosis due to mucormycosis in an uncontrolled diabetic patient. Early diagnosis and prompt treatment can reduce the mortality and morbidity of this lethal fungal infection.
KEY WORDS: Maxilla, mucormycosis, prosthesis, rehabilitation
The maxilla rarely undergoes necrosis due to its rich vascularity. Maxillary necrosis can occur due to bacterial infections such as osteomyelitis, viral infections such as herpes zoster or fungal infections such as mucormycosis, aspergillosis other causes other than infections such as trauma, radiation, use of long-term corticosteroids, disorders of lipid metabolism such as Gaucher disease, etc., Mucormycosis is an opportunistic fulminant fungal infection, which mainly infects immunocompromised patients. Most individuals are exposed to these fungi on a daily basis, but people with weakened immune systems are more susceptible to infection. The infection begins in the nose and para nasal sinuses due to inhalation of fungal spores.[1,2] The infection can spread to orbital and intracranial structures either by direct invasion or through the blood vessels.[3,4] The fungus invades the arteries leading to thrombosis that subsequently causes necrosis of hard and soft tissues. We report a case of maxillary necrosis due to mucormycosis in an uncontrolled diabetic patient. Early diagnosis and prompt treatment can reduce the mortality and morbidity of this lethal fungal infection.
Case Report
A 65-year-old male patient came to our hospital with the complaint of pain and difficulty in taking food of 6 months duration. Patient was apparently normal 1 year before this, he developed pain and swelling in the upper jaw region which gradually increased in size to present size. Pain was continuous and radiating to the temporal region had aggravated with movement of the head, patient was febrile. He gave a history having undergone extraction of mobile maxillary teeth 6 months before. He reported to our clinic with present symptoms. Apparently following the extraction, the socket never healed completely.
Patient was a known diabetic on irregular treatment with oral hypoglycemics for the last 10 years. On general examination, middle aged man conscious and co-operative, febrile, no signs of anemia and jaundice. Intraoral oral examination showed [Figure 1] exposure of black bare bone with the loss of mucoperiosteum over the entire maxillary alveolar process of palate up to the soft palate region with palatal fistula in the soft palate region.
Figure 1.

Intra-oral photograph
On radiological examination [Figure 2], computed tomography scan revealed erosion of the anterolateral wall of right maxillary antrum with thickening of the sinus lining with moth eaten appearance of the maxillary bone seen.
Figure 2.

Computed tomography of maxilla
Discussion
Opportunistic fungal infections such as mucormycosis usually occur in immunocompromised patients, but can infect healthy individuals as well.[2] The predisposing factors for mucormycosis are uncontrolled diabetes (particularly in patients with ketoacidosis), malignancies such as lymphomas and leukemia's, renal failure, organ transplant, long-term corticosteroid and immunosuppressive therapy, cirrhosis, burns, protein energy malnutrition and acquired immune deficiency syndrome. Our patient had uncontrolled diabetes, which is a well-known predisposing factor for mucormycosis.[1,2,3,4,5,6,7,8]
Mucormycosis (Zygomycosis, phycomycosis) is an acute opportunistic infection caused by a saprophytic fungus that belongs to the class of phycomycetes. Although several genera are associated with this disease, the most common forms are Rhizopus, Rhizomucor and Absida. Rhizopus is the predominant pathogen accounting for 90% of the cases of rhinocerebralmucormycosis. This microbe may be cultured from the oral cavity, nasal passages, throat and stool of healthy patients without clinical signs of infection.
Uncontrolled diabetes mellitus can alter the normal immunologic response of patients to infections. Such patients have decreased granulocyte phagocytic ability with altered polymorphonuclear leukocyte response.
This fungal infection usually originates from the para nasal sinuses. The fungus invades the blood vessels and subsequently spreads through them. Once fungal hyphae enter into the blood stream they can disseminate to other organs such as cerebrum or lungs, which can be fatal for patient. Mucor hyphae form thrombi within the blood vessels that reduce vascularity to the tissues and cause necrosis. Peripheral vascular disease (due to microangiopathy and atherosclerosis) in diabetic patients also causes local tissue ischemia and increased susceptibility to infections.[5] Therefore, thrombosis of the internal maxillary artery or descending palatine artery caused by mucormycotic infection[4] as well as chronic diabetes in this patient had resulted in necrosis of the maxilla.
Usually mucormycosis occurs as a pulmonary, gastrointestinal, disseminated or rhinocerebral infection. In our patient, infection was only localized to the maxilla and it underwent necrosis without any other symptoms. Disseminated involvement of mucormycosis is observed in diabetics with ketoacidosis, which favors rapid proliferation of fungus and its invasion into orbit and cerebrum.[6] Mucormycosis is aggressive and potentially fatal in diabetic patients because of impaired host defense mechanism and increased availability of micronutrients such as iron.[5] The general health of this patient was good and he did not develop ketoacidosis hence the infection did not disseminate to other organs. Therefore, in this case the patient had a localized rhino-maxillary form of the disease which is a subdivision of well-documented rhinocerebral mucormycosis.[7,8] However, the infection may spread to involve the cranium, orbit and other organs if left untreated, which can prove fatal.
In the early stages of the disease, patients exhibit facial cellulits, paresthesia over the face, nasal discharge, necrotic turbinates, fever, headache and lethargy.[5] However, in contrast to other reports many of these symptoms were not present in this patient.
Among the clinical differential diagnosis we can consider squamous cell carcinoma of maxillary sinus. Such cases present as chronic ulcers with raised margins causing exposure of underlying bone. A malignant salivary gland tumor arising from the accessory glands of the palate can also be considered in the differential diagnosis. Other features seen in cases of antral carcinoma are local pain, swelling, epistaxis, nasal discharge, epiphora, diplopia or numbness. In this patient there were no symptoms suggestive of any malignancy and histopathological picture ruled out carcinoma.
There is a close histopathological resemblance between mucormycosis and aspergillosis. Microscopically, aspergillosis has septate branching hyphae, which can be distinguished from mucormycotic hyphae by a smaller width and prominent acute angulations of branching hyphae.[5] Moreover, the fungal organism produces conidiophores, which were absent in this case. A definitive diagnosis of mucormycosis can be made by tissue biopsy that identifies the characteristic hyphae, by positive culture or both. Initial culture of diseased tissue may be negative and histopathologic examination is essential for early diagnosis. In this case, the fungus was identified and confirmed with periodic acid schiff stain. The tissue involved in this section showed variable amount of necrosis. The organism appears non-septate hyphae with branching at obtuse angle showing in Figure 3.
Figure 3.
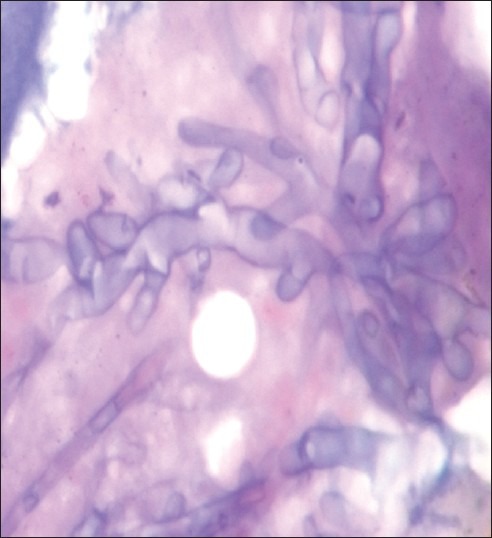
Histopathologic appearance of septae
Mucormycosis was long regarded as a fatal infection with poor prognosis. However, with early medical and surgical management survival rates are now thought to exceed 80%.[6] This patient survived because of an early diagnosis and prompt treatment.
In conclusion, an immunocompromised or immunosuppressed patient having bone necrosis following tooth extraction should alert a clinician of possible mucormycotic infection.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.Leitner C, Hoffmann J, Zerfowski M, Reinert S. Mucormycosis: Necrotizing soft tissue lesion of the face. J Oral Maxillofac Surg. 2003;61:1354–8. doi: 10.1016/s0278-2391(03)00740-7. [DOI] [PubMed] [Google Scholar]
- 2.Pogrel MA, Miller CE. A case of maxillary necrosis. J Oral Maxillofac Surg. 2003;61:489–93. doi: 10.1053/joms.2003.50095. [DOI] [PubMed] [Google Scholar]
- 3.Del Valle Zapico A, Rubio Suárez A, Mellado Encinas P, Morales Angulo C, Cabrera Pozuelo E. Mucormycosis of the sphenoid sinus in an otherwise healthy patient. Case report and literature review. J Laryngol Otol. 1996;110:471–3. doi: 10.1017/s0022215100134012. [DOI] [PubMed] [Google Scholar]
- 4.Jones AC, Bentsen TY, Freedman PD. Mucormycosis of the oral cavity. Oral Surg Oral Med Oral Pathol. 1993;75:455–60. doi: 10.1016/0030-4220(93)90170-9. [DOI] [PubMed] [Google Scholar]
- 5.Tugsel Z, Sezer B, Akalin T. Facial swelling and palatal ulceration in a diabetic patient. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:630–6. doi: 10.1016/j.tripleo.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 6.Buhl MR, Joseph TP, Snelling BE, Buhl L. Temporofacial zygomycosis in a pregnant woman. Infection. 1992;20:230–2. doi: 10.1007/BF02033066. [DOI] [PubMed] [Google Scholar]
- 7.Greenberg MS. Ulcerative vesicular and bullous lesions. In: Greenberg MS, Glick M, editors. Burket's oral medicine diagnosis and Treatment. India: Elsevier; 2003. p. 79. [Google Scholar]
- 8.Hazarika P, Ravikumar V, Nayak RG, Rao PS, Shivananda PG. Rhinocerebral mycosis. Ear Nose Throat J. 1984;63:464–8. [PubMed] [Google Scholar]


