Figure 2.
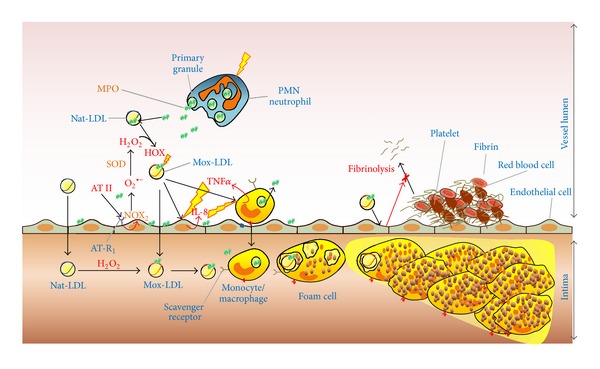
Role of myeloperoxidase and Mox-LDL in triggering inflammation and atherosclerosis plaque formation. Activation of neutrophils and monocytes leads to MPO release in the extracellular space, that is, the circulation. Due to its cationic properties, free MPO rapidly adsorbs at the surface of endothelial cells or native LDL (Nat-LDL). Angiotensin II (AT II) activates endothelial cells via angiotensin receptor 1 (AT-R1), which in turn produces superoxide anion (O2 •−) via the NADPH oxidase complex, (NOX2). O2 •− is rapidly transformed into hydrogen peroxide (H2O2) spontaneously or by the enzyme superoxide dismutase (SOD). Nat-LDL can be so directly oxidized by MPO/H2O2/chloride system in the circulation and form the so-called Mox-LDL. The latter can in turn pass through the endothelium (due to endothelial dysfunction) to the subendothelial space where it will be recognized by macrophages and eliminated. Accumulation of oxidized lipoproteins leads to foam cell formation and lipid accumulation in the subendothelial space. Nat-LDL, can also directly pass through the endothelial wall where they are oxidized by MPO in the subendothelial space. Finally, LDL oxidized by myeloperoxidase (Mox-LDL) activates endothelial cells and induces interleukine-8 (IL-8) secretion by these cells. Mox-LDL effects on monocyte are similar and activate tumor-necrosis factor-α (TNFα) secretion by these cells. In turn, IL-8 and TNFα activate monocytes and endothelial cells, respectively. Mox-LDL also inhibits fibrinolysis process via endothelial cell interaction.
