Abstract
Introduction
Focused assessment with sonography for trauma (FAST) is commonly used to facilitate the timely diagnosis of life threatening hemorrhage in injured patients. Most patients with positive findings on FAST require laparotomy. Though it is assumed that an increasing time to operation leads to higher mortality, this relationship has not been quantified. This study sought to determine the impact of time to operation (T-OR) on survival in patients with a positive FAST that required emergent laparotomy.
Methods
We retrospectively analyzed patients from the Prospective Observational Multicenter Major Trauma Transfusion (PROMMTT) study that underwent laparotomy within 90 minutes of presentation and had a FAST performed. Cox proportional hazards models including Injury Severity Score (ISS), age, base deficit and hospital site were created to examine the impact of increasing T-OR on in-hospital survival at 24 hours and 30 days. The impact of time from the performance of the FAST exam to operation (TFAST-OR) on in-hospital mortality was also examined using the same model.
Results
One hundred and fifteen patients met study criteria and had complete data. Increasing T-OR was associated with increased in-hospital mortality at 24 hours (hazard ratio [HR] 1.50 for each 10 minute increase in T-OR, confidence interval [CI] 1.14-1.97, p = 0.003) and 30 days (HR 1.41, CI 1.18-2.10, p = 0.002). Increasing TFAST-OR was also associated with higher in-hospital mortality at 24 hours (HR 1.34, CI 1.03-1.72, p = 0.03) and 30 days (HR 1.40, CI 1.06-1.84, p = 0.02).
Conclusion
In patients with a positive FAST who required emergent laparotomy, delay in operation was associated with increased early and late in-hospital mortality. Delays in time to operation in trauma patients with a positive FAST should be minimized.
Keywords: time to operation, laparotomy, FAST examination, PROMMTT
Introduction
Trauma is one of the leading causes of death worldwide.1 In the last few decades, extensive efforts have been made to develop and improve trauma systems in an effort to improve outcomes after injury.2-4 It is commonly assumed that the time to definitive surgical care of life threatening injuries is an important determinant of mortality. This has been demonstrated in patients with subdural hematomas5-7 but data for other types of operations are sparse.
Few studies have directly examined the impact of time to the operating room (T-OR) on survival in patients requiring emergent laparotomy for trauma. A longer time to operation has been shown to increase mortality in patients with traumatic hollow viscus injury, largely due to delays in diagnosis.8,9 Clarke et al published a retrospective study in 2002 that used logistic regression to demonstrate that increasing time in the emergency department increased the probability of death by 0.35% per minute in hypotensive trauma patients.10 In general, for operations performed in the acute setting, an association between a longer T-OR and increased mortality has been difficult to demonstrate. This may be in part due to indication bias, since patients that have a longer T-OR may have less severe injuries and therefore a lower expected mortality.
The recently completed PRospective Observational Multicenter Major Trauma Transfusion (PROMMTT) study was designed primarily to examine issues related to blood product transfusion in trauma patients.11 The extensive data collected by the PROMMTT investigators made it possible to study other aspects of trauma care as well. The purpose of this study was to determine the impact of T-OR on mortality in trauma patients requiring emergent laparotomy that present with a positive focused assessment with sonography for trauma (FAST). Our hypothesis was that increasing T-OR would lead to decreased survival. The primary endpoints were 24-hour and 30-day mortality.
Materials and Methods
Data were obtained from a database created by the PROMMTT Data Coordinating Center at the University of Texas Health Science Center at Houston for the PROMMTT study. PROMMTT enrolled 1245 injured patients who required the highest level activation at one of ten level 1 trauma centers and who subsequently received one or more units of red blood cells (RBC) within six hours of hospital admission. Exclusion criteria included age less than 16, transfer from another hospital, pregnancy, more than 20% burn injury, inhalation injury, incarceration, cardiopulmonary resuscitation lasting more than five minutes prehospital or in the first 30 minutes after admission, and death within 30 minutes of hospital admission.11 Data were collected in real time on a wide variety of patient characteristics, treatments, including fluid and blood product infusions, diagnostic studies, and surgical intervention. The time of mortality or hospital discharge was recorded. Approval was obtained from the Institutional Review Board at each center and from the US Army Human Research Protections Office.
Our study examined the subset of patients that had a FAST performed and underwent laparotomy within the first 90 minutes after hospital admission. This time point was selected because we sought to exclude patients that underwent operation in a delayed fashion for missed injury or failure of planned nonoperative management. Examination of the distribution of T-OR for the entire database suggested that 90 minutes from initial presentation was a natural cutoff point for this. The time intervals from hospital admission to the FAST and to the operating room were recorded. Cox proportional hazards models were created including Injury Severity Score (ISS), age, base deficit, hospital site, and T-OR. We also generated the same models using the time interval between performance of the FAST and the operating room (TFAST-OR). In-hospital mortality at 24 hours and 30 days was studied. Hazard ratios were expressed in terms of 10-minute intervals in T-OR or TFAST-OR. For each model, the proportional hazards assumption was tested with Schoenfeld residuals. Statistical analyses were carried out with Stata 12.1 (StataCorp, College Station, TX 2012). P values of less than 0.05 were considered significant.
Results
The overall PROMMTT study enrolled 1245 patients. FAST studies were obtained in 838 patients, of which 255 were positive (30.4%). Among these, 72% (n=184) underwent laparotomy within the first 24 hours (mean T-OR = 64 ± 92 min). T-OR was ≤ 90 min in 147 patients (79.8%); 115 patients had complete data and comprised the study group. Baseline demographic and injury severity scoring data are shown in Table 1. Physiologic and biochemical data obtained upon hospital arrival are shown in Table 2. The mean time to performance of the FAST was 8.2 ± 9.7 minutes.
Table 1.
Baseline characteristics among 115 PROMMTT patients with positive FAST who underwent emergent laparotomy
| Age(yr) | 37±16 |
| ISS | 29 (17-38) |
| AIS head | 0 (0-2) |
| AIS chest | 3 (0-4) |
| AIS abdomen | 3 (3-4) |
| AIS extremity | 2 (0-3) |
| Sex | 77.3% male |
| Mechanism | 64.3% blunt |
Values are mean ± SD or median (IQR)
Table 2.
Initial physiologic and biochemical data among 115 PROMMTT patients with positive FAST who underwent emergent laparotomy
| SBP (mmHg) | 100 ± 30 |
| DBP (mmHg) | 64 ± 23 |
| HR | 106 ± 27 |
| Hemoglobin (g/dl) | 11.2 ± 2.5 |
| pH | 7.23 ± 0.13 |
| Base deficit | 7.8 ± 5.7 |
| INR | 1.5 ± 1.0 |
| PTT | 32.7 ± 20.0 |
Values are mean ± SD
The operative procedures conducted are listed in table 3. Damage control operations were done in 76 cases (66%). Forty-seven patients (40.8%) had a bowel resection or repair; 42 patients (36.5%) underwent splenectomy or splenorrhaphy and 41 patients (35.6%) had some form of operative hemostasis of the liver. A concomitant thoracic operation was performed in 23 cases (20%) and a craniotomy was performed in 1 patient (0.8%). Three patients had nontherapeutic laparotomies (2.6%). All laparotomies in patients with initial SBP < 90 mmHg (n=43) were therapeutic.
Table 3.
Operative procedures performed upon patients with a positive FAST undergoing laparotomy in ≤ 90 minutes (n=115)
| Operation | N (%) |
|---|---|
| Splenectomy | 39 (34) |
| Small bowel resection | 29 (25) |
| Hemostasis of liver | 25 (22) |
| Repair small bowel | 23 (20) |
| Perihepatic packing | 21 (18) |
| Repair of artery | 16 (14) |
| Colon resection | 15 (13) |
| Repair colon | 13 (11) |
| Repair of vein | 11 (10) |
| Genitourinary procedure | 9 (8) |
| Nephrectomy or other kidney procedure | 6 (5) |
| Colostomy or ileostomy | 6 (5) |
| Pancreatic procedure | 5 (4) |
| Partial hepatectomy | 4 (3) |
| Cholecystectomy | 4 (3) |
| Splenorrhaphy | 3 (3) |
*Percentages add to greater than 100 due to multiple procedures in some patients
Blood product requirements for the cohort are listed in Table 4. Massive transfusions (defined as ≥ 10 units RBC given in the first 24 hr) were required in 51 cases (44.3%). In 39 of these cases (76.4%), the threshold for massive transfusion was reached within the first 6 hours.
Table 4.
Blood product requirements among patients with a positive FAST undergoing laparotomy in ≤90 minutes (n=115)
| Blood product (units) | 6 hours | 24 hours |
|---|---|---|
| RBC | 10.5 ± 11.0 | 13.1 ± 11.0 |
| Plasma | 7.9 ± 8.6 | 10.7 ± 10.7 |
| Platelets | 5.8 ± 9.8 | 7.2 ± 11.3 |
Values are mean ± SD
Unadjusted in-hospital mortality at different time points is shown in Table 5. Overall in- hospital mortality for the cohort was 20%, with slightly more than half of the deaths occurring within the first 24 hours (Table 5). Fifty-seven percent of deaths were due to hemorrhage. Head injury was listed as one of the causes of death in 4 patients (3.6%).
Table 5.
Mortality at different time points among patients with a positive FAST undergoing laparotomy in ≤90 minutes (n=115)
| Time | % mortality |
|---|---|
| 2 hr | 3.5 |
| 6 hr | 5.2 |
| 12 hr | 10.4 |
| 24 hr | 11.3 |
| 72 hr | 12.1 |
| 30 days | 20.0 |
The mean T-OR was 36 ± 21 minutes. The multivariable Cox proportional hazards model showed that increased T-OR was associated with increased in-hospital mortality at 24 hours (HR for each 10 minute increase 1.50, CI 1.14-1.97, p = 0.003) and 30 days (HR 1.58, CI 1.18-2.10, p = 0.002). Increased TFAST OR was also associated with increased mortality at 24 hours (HR 1.34, CI 1.03-1.72, p = 0.03) and 30 days (HR 1.40, CI 1.06-1.84, p = 0.02). For each model, the proportional hazards assumption was verified by analysis of Schoenfeld residuals (data not shown). Graph 1 shows the theoretical survival curve for the T-OR model in which each variable in the model is fixed at its mean value. Separate curves for T-OR = 36 minutes (the mean value for the cohort) and T-OR = 56 minutes (meant to represent the mean value plus 20 minutes) are shown.
Discussion
Common sense dictates that patients that require an emergent laparotomy for trauma should do better if the operation is done in an expedient fashion. This concept is deeply ingrained in the trauma community. Trauma systems and clinical protocols are designed to minimize the time required to obtain definitive surgical control of hemorrhage. The time from hospital arrival to emergent surgical intervention has been used as an audit filter for assessment of trauma systems in several different countries.4,12
Despite this, a direct correlation between time to operation and mortality has been difficult to demonstrate. One study by Clarke et al showed a correlation between increased time in the ED and mortality in hypotensive trauma patients.10 In contrast, another study reported that patients examined using an audit filter of 2 hours to laparotomy showed decreased mortality in the >2 hour group.13 A similar phenomenon has been seen in studies showing a lower overall mortality in patients with longer times to evacuation of acute subdural hematoma.14,15 Indication bias was present in each study, in that patients with more severe injuries tended to undergo operation sooner.
We attempted to minimize this bias by creating a Cox proportional hazards model and by using a highly selected group of patients. The cohort represents the subset of trauma patients with severe injuries in whom the need for laparotomy is identified on initial evaluation in the emergency department. Since this study was limited to patients that required an operation in the first 90 minutes after arrival, it is unlikely that patients with delayed recognition of bowel injury or failure of planned nonoperative management of solid organ injuries were included. We controlled for other factors that are known to affect mortality, such as ISS and age. Base deficit was included as a surrogate for shock. Hospital site was also included in the model.
One important caveat for this study is that findings on FAST did not correlate well with the need for an emergent operation. Only 72% of patients with a positive FAST received a laparotomy within the first 24 hours. Although a few patients may have had significant injuries that were initially not detected, we presume that these instances were rare, and that the majority of patients that did not undergo operation were found on subsequent workup to have injuries that were amenable to nonoperative management. Therefore, it would be premature to proceed directly to the operating room in all patients with positive FAST studies. This would lead to a significant number of nontherapeutic laparotomies, which are thought to be associated with significant morbidity,16-18 though this has been questioned.1 In this study, only three patients underwent non-therapeutic laparotomy.
When an injured patient is noted to have a positive FAST, a choice must be made between obtaining additional diagnostic studies or proceeding to the operating room. Since delays in operation in this group are associated with higher mortality, efforts to minimize the time to the operating room are justified. In many hospitals, much of the delay is accounted for by the length of time needed to obtain CT scans. This typically requires a number of ancillary tasks including transporting the patient to the CT scanner, transfer to the gantry, manipulation of lines and devices, injection of contrast, programming the scanner, and so forth. This is rarely accomplished in less than 20 minutes, and may take an hour or more in many centers. Selection of patients with positive FAST scans that should go directly to the operating room without obtaining a CT scan is therefore important. It is generally accepted that hypotensive patients with a positive FAST should undergo immediate laparotomy.20 No other specific indications for deferring the CT scan have been described. Scoring systems have been developed,21-23 but none have been widely adopted. There are other ways to minimize the time to operation in patients with a positive FAST exam. Trauma center protocols could be modified so that all FAST positive patients would be upgraded to the highest level of trauma team activation. This would result in earlier mobilization of the attending surgeon, as well as the anesthesiologist and OR staff. In non-trauma hospitals, a FAST should prompt immediate surgical consultation. Clinicians in hospitals without surgical capabilities should consider arranging for transfer of all patients with a positive FAST to a trauma center before obtaining a confirmatory CT scan.
This study has a variety of limitations. The database contained only patients who received at least one unit of RBCs, so our findings may not apply to the entire population of trauma patients. Also, many of the factors that may contribute to variations in T-OR are not captured in the original PROMMTT database. We were not able to quantify the time required to obtain diagnostic studies and mobilize the anesthesia and OR staff and thus could not determine the relative impact of these factors. There may also be a degree of imprecision in recording exactly when a patient arrived in the OR. The time from initial OR arrival to the actual start of the surgical procedure and the time to definitive hemorrhage control were also not recorded.
In conclusion, this is the only study to date that utilizes survival analysis to demonstrate that increasing time to operation is associated with increased mortality in patients with a positive FAST that undergo emergent laparotomy. The established standard that hypotensive patients should proceed directly to operation should be maintained. Additional criteria that would mandate immediate laparotomy in the presence of a positive FAST should be sought in future studies. Efforts to allocate resources so as to minimize the time to operation in patients with a positive FAST are justified.
Figure 1.
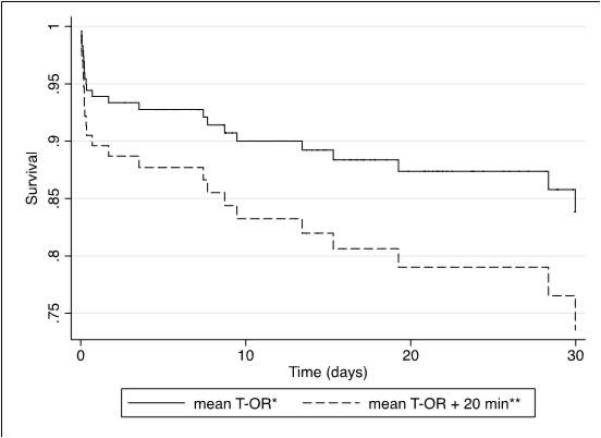
Survival curve for FAST(+) patients undergoing laparotomy in ≤ 90 minutes
* Mean T-OR for the cohort was 36 minutes
** Theoretical curve for patients with T-OR = 56 minutes
Acknowledgments
Funding/Support: This project was funded by the U.S. Army Medical Research and Materiel Command subcontract W81XWH-08-C-0712. Infrastructure for the Data Coordinating Center was supported by CTSA funds from NIH grant UL1 RR024148.
Role of the Sponsor: The sponsors did not have any role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review or approval of the manuscript; or the decision to submit this manuscript for publication.
Footnotes
Conflict of Interest Disclosures: Dr Holcomb reported serving on the board for Tenaxis, the Regional Advisory Council for Trauma, and the National Trauma Institute; providing expert testimony for the Department of Justice; grants funded by the Haemonetics Corporation, and KCI USA, Inc. and consultant fees from the Winkenwerder Company. Dr Wade reported serving on the Science Board for Resuscitation Products, Inc. and the Advisory Board for Astrazeneca. No other disclosures were reported.
Disclaimer: The views and opinions expressed in this manuscript are those of the authors and do not reflect the official policy or position of the Army Medical Department, Department of the Army, the Department of Defense, or the United States Government.
Previous Presentation of the Information Reported in the Manuscript: These data were presented at the PROMMTT Symposium held at the 71st Annual Meeting of the American Association for the Surgery of Trauma (AAST) on September 10-15, 2012 in Kauai, Hawaii.
AUTHOR CONTRIBUTIONS
Study concept and design: Barbosa, Rowell, Fox, Holcomb, del Junco, Rahbar
Acquisition of data: Alarcon, Brasel, Bulger, Cohen, Cotton, Holcomb, Muskat, Myers, Phelan, Schreiber
Analysis and interpretation of data: Barbosa, Rowell, Fox, Schreiber
Drafting of the manuscript: Barbosa, Rowell
Critical revision of the manuscript for important intellectual content: Barbosa, Rowell, Fox, Bulger, Brasel, Schreiber, del Junco, Holcomb, Rahbar, Wade, Alarcon, Cohen, Cotton, Muskat, Myers, Phelan
Obtained funding: Rahbar
Administrative, technical, or material support: Rahbar, Holcomb, Fox, del Junco, Alarcon, Brasel, Bulger, Cohen, Cotton, Muskat, Myers, Phelan, Schreiber, Wade
Study supervision: Rahbar, Holcomb
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Committee on Injury Prevention and Control; Institute of MedicineBonne RJ, Fulco CE, Liverman CT, editors. Reducing the Burden of Injury: Advancing Prevention and Treatment. National Academy Press; Washington, DC: 1999. pp. 42–43. [PubMed] [Google Scholar]
- 2.American College of Surgeons Committee on Trauma . Resources for Optimal Care of the Injured Patient. American College of Surgeons; Chicago: 2006. [Google Scholar]
- 3.Hemmila MR, Nathens AB, Shafi S, et al. The Trauma Quality Improvement Program: pilot study and initial demonstration of feasibility. J Trauma. 2010;68(2):253–262. doi: 10.1097/TA.0b013e3181cfc8e6. [DOI] [PubMed] [Google Scholar]
- 4.Stelfox HT, Bobranska-Artiuch B, Nathens A, et al. Quality indicators for evaluating trauma care. A scoping review. Arch Surg. 2010;145:286–295. doi: 10.1001/archsurg.2009.289. [DOI] [PubMed] [Google Scholar]
- 5.Wright KD, Knowles CGH, Coats TJ, et al. Efficient timely evacuation of intracranial haematoma – the effect of transport direct to a specialist centre. Injury. 1996;27:719–721. doi: 10.1016/s0020-1383(96)00119-2. [DOI] [PubMed] [Google Scholar]
- 6.Seelig JM, Becker DP, Miller JD, et al. Traumatic acute subdural hematoma. N Engl J Med. 1981;304:1511–1518. doi: 10.1056/NEJM198106183042503. [DOI] [PubMed] [Google Scholar]
- 7.Tian HL, Chen SW, Xu T. Risk factors related to hospital mortality in patients with isolated traumatic acute subdural haematoma: analysis of 308 patients undergoing surgery. Chin Med J. 2008;20:1080–1084. et a. [PubMed] [Google Scholar]
- 8.Malinoski DJ, Patel MS, Yakar DO, et al. A diagnostic delay of 5 hours increases the risk of death after blunt hollow viscus injury. J Trauma. 2010;69:84–87. doi: 10.1097/TA.0b013e3181db37f5. [DOI] [PubMed] [Google Scholar]
- 9.Fakhry SM, Brownstein M, Watts DD, et al. Relatively short diagnostic delays (<8 hours) produce morbidity and mortality in blunt small bowel injury: an analysis of time to operative intervention in 198 patients from a multicenter experience. J Trauma. 2000;48:408–414. doi: 10.1097/00005373-200003000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Clarke JR, Trooskin SZ, Doshi PJ, et al. Time to laparotomy for intra-abdominal bleeding from trauma does affect survival for delays up to 90 minutes. J Trauma. 2002;52:420–425. doi: 10.1097/00005373-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Rahbar MH, Fox EE, del Junco DJ, et al. Coordination on management of multicenter clinical studies in trauma: Experience from the Prospective Observational Multicenter Major Trauma Transfusion (PROMMTT) study. Resuscitation. 2012;83:459–464. doi: 10.1016/j.resuscitation.2011.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yates DW, Woodford M, Hollis S. Preliminary analysis of the care of injured patients in 33 British hospitals: first report of the United Kingdom major trauma outcome study. BMJ. 305(6856):737–740. doi: 10.1136/bmj.305.6856.737. 1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nayduch D, Moylan J, Snyder BL, et al. American College of Surgeons trauma quality indicators: an analysis of outcome in a statewide trauma registry. J Trauma. 1994;37:565–573. doi: 10.1097/00005373-199410000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Tien HCN, Jung V, Pinto R, et al. Reducing time-to-treatment decreases mortalityof trauma patients with acute subdural hematoma. Ann Surg. 2011;253:1178–1183. doi: 10.1097/SLA.0b013e318217e339. [DOI] [PubMed] [Google Scholar]
- 15.Rifai MHS, Stone JL, Sugar O, et al. Subdural hematomas. 1. Acute subdural hematoma: progress in definition, clinical pathology and therapy. Surg Neurol. 1983;19:216–231. doi: 10.1016/s0090-3019(83)80005-6. [DOI] [PubMed] [Google Scholar]
- 16.Renz BM, Feliciano DV. Unnecessary laparotomies for trauma: a prospective study of morbidity. J Trauma. 1995;38:350–356. doi: 10.1097/00005373-199503000-00007. [DOI] [PubMed] [Google Scholar]
- 17.Morrison JE, Wisner DH, Bodai BI. Complications after negative laparotomy for trauma: long-term follow-up in a health maintenance organization. J Trauma. 1996;41:509–513. doi: 10.1097/00005373-199609000-00021. [DOI] [PubMed] [Google Scholar]
- 18.Ross SE, Dragon M, O'Malley KF, et al. Morbidity of negative coeliotomy in trauma. Injury. 1995;26:393–394. doi: 10.1016/0020-1383(95)00058-h. [DOI] [PubMed] [Google Scholar]
- 19.Crookes BA, Shackford SR, Gratton J, et al. “Never be wrong”: the morbidity of negative and delayed laparotomies after blunt trauma. J Trauma. 2010;69:1386–1391. doi: 10.1097/TA.0b013e3181fd6977. [DOI] [PubMed] [Google Scholar]
- 20.Hoff WS, Holevar M, Nagy KK, et al. Practice management guidelines for the evaluation of blunt abdominal trauma: the EAST Practice Management Guidelines work group. J Trauma. 2002;53:602–615. doi: 10.1097/00005373-200209000-00038. [DOI] [PubMed] [Google Scholar]
- 21.McKenney KL, McKenney MG, Cohn SM, et al. Hemoperitoneum score helps determine need for therapeutic laparotomy. J Trauma. 2001;50:650–656. doi: 10.1097/00005373-200104000-00009. [DOI] [PubMed] [Google Scholar]
- 22.Huang MS, Liu M, Wu JK, et al. Ultrasonography for the evaluation of hemoperitoneum during resuscitation: a simple scoring system. J Trauma. 1994;36:173–177. doi: 10.1097/00005373-199402000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Manka M, Moscati M, Raghavendran K, et al. Sonographic scoring for operating room triage in trauma. West J Emerg Med. 2010;11:138–143. [PMC free article] [PubMed] [Google Scholar]


