Abstract
Background:
Haemangioma (HM) and venous malformations of the head and neck are formidable lesions as they cause cosmetic deformity and psychological problems. Their surgical excision is difficult and fraught with problems like operative blood loss, incomplete excision, disfigurement and recurrence. Endovascular techniques like sclerotherapy and embolization are increasingly being used in the treatment of these difficult lesions.
Objectives:
This study was undertaken to analyse the efficacy and safety of endovascular techniques in the treatment of HM and slow flow vascular malformations.
Materials and Methods:
We retrospectively reviewed the records and clinical photographs of 358 patients of HM and slow flow vascular malformations treated in our institute by endovascular approach over a 15 year period. Pre- and post-treatment photographs were compared and outcomes categorized as complete resolution (>90% reduction), considerable reduction (60-90% reduction), partial reduction (20-60% reduction) and no change (<20% reduction).
Results:
Complete resolution of the lesion was seen in 30% of the patients while 50% patients showed considerable reduction of the swelling. Complications occurred in 6.4% of patients.
Conclusion:
We conclude that sclerotherapy is an effective and safe treatment modality for these lesions and may be considered as the primary modality in the treatment of these challenging lesions.
KEY WORDS: Bleomycin, hemangioma, sclerotherapy, sodium tetradecyl sulfate, venous malformation
INTRODUCTION
Vascular malformations of the head and neck can cause cosmetic and functional disturbances. These may lead to enormous psychosocial problems for patients and their families. Various treatment options are available depending upon the vascular dynamics of the lesion. The vascular anomalies have been classified into haemangiomas (HM), high flow vascular malformations and low flow vascular malformations by Mulliken et al.,[1,2]
In this study, we dealt with the management of HM and low flow vascular malformations. Hence, discussion will involve these lesions. Treatment options include endovascular embolization and percutaneous/permucosal sclerotherapy. Surgical excision of venous malformations (VM) has limitations. There are chances of significant intraoperative bleeding as well as inadvertent injury to important head and neck structures. Furthermore, cosmetic disfigurement or recurrence may result from incomplete or inappropriate excision.[3,4] Similarly, surgery of lymphatic malformations (LM) is fraught with recurrence.[5] Sclerotherapy can be used either in isolation for smaller lesions or followed by the surgical resection for larger lesions. While there is no singular superior treatment modality for VM, for LM, sclerotherapy is the mainstay of treatment.[6]
This study represents single centre experience in the management of HM and low flow vascular malformations of the head and neck region. To the best of our knowledge and extensive literature search, this is the largest study to date on low flow vascular malformations from India.
MATERIALS AND METHODS
Patient demographics
This study was performed by analysing retrospectively the records of patients with HM and low flow maxillofacial vascular malformations who were treated in the interventional neuroradiology department of our institute from January 1995 to December 2009. The clinical features, examination findings and imaging features were studied in detail. The imaging data was mainly ultrasound with colour doppler, computed tomography scan or magnetic resonance imaging (MRI). Patients were classified into HM and low flow vascular malformations based on clinical and imaging findings. Low flow vascular malformations were further subdivided into VM, LM and veno-lymphatic malformations (VLM).
Pre-procedure angiogram was performed in all patients with HM. HM presenting in the proliferative phase were treated with trans-arterial embolization with polyvinyl alcohol (PVA) particles followed by the percutaneous injections of Bleomycin. HM presenting in the involuting phase which were affecting function, such as vision and hearing, were managed by multiple sessions of percutaneous sclerotherapy to augment involution. Bleomycin and sodium tetradecyl sulfate (STD) were used as sclerosants. STD was used for sclerotherapy when there was backflow of blood while Bleomycin was used when there was no backflow of blood on insertion of needle into the lesion. Percutaneous n-Butyl cyanoacrylate (nBCA) glue embolization was performed for preoperative embolization of lesions. The treatment sessions were performed under general anaesthesia for infants and small children while intravenous sedation was used for older children.
Vascular malformations
Pre-procedure angiogram was not performed for all patients with low-flow vascular malformations. It was carried out only for atypical cases and when the diagnosis was in doubt. However, percutaneous venogram was performed for all patients with vascular malformations prior to the treatment sessions. Low flow vascular malformations were primarily managed by percutaneous sclerotherapy. STD was the sclerosant of choice. STD was injected mixed with lipiodol under fluoroscopic guidance. The amount of STD used per session was dependent on the size of the vascular malformation and ranged from 2 cc for smaller malformations to 10 cc of for larger malformations. In case of LM aspiration of fluid from the lesion was performed as much as possible. Subsequently, Bleomycin was injected followed by strapping for few days. The amount of Bleomycin injected depended on the size of the malformation and ranged from 2 to 15 units per session. Strapping allows apposition of the walls thus facilitating induction of inflammatory adhesions by Bleomycin.
Multiple sessions of sclerotherapy were performed at an interval of 4 weeks. Treatment was stopped when >90% reduction of the swelling was achieved or if no change occurred over three treatment sessions. At the time of analysis, the pre-procedure data (clinical photographs and imaging) were compared with those at last follow-up. The clinical photographs were taken in two standardized views at each follow-up. The comparison was carried out in considerations with the norms of standardization. Comparison of imaging was also carried out for patients where imaging was available. Outcomes were graded as complete reduction (>90% reduction), considerable reduction (60-90% reduction), partial reduction (20-30% reduction) and no change (<20% reduction). Complete resolution and a considerable reduction was considered to be a successful treatment outcome.
RESULTS
A total of 437 patients with low flow vascular malformations and HM of the head and neck were treated in the interventional neuroradiology department of our institute from January 1996 to December 2010. Out of these, 66 patients were lost to follow-up prior to the completion of all treatment sessions. These patients were excluded from the study. Treatment was not completed in another five patients during the study period. These, too, were excluded. In addition, eight patients with HM were advised conservative management. As a result, a total of 358 patients were included in the study. A total of 68 patients had HM and 290 patients had low flow vascular malformations, of which 272 were VM, 10 were LM and 8 were VLM.
Clinical presentation
The most common presentation was swelling in the head and neck region. Bleeding from the vascular malformation was another presenting feature, mainly for haemagiomas. Other presenting features were visual loss, hearing loss and facial palsy due to large and trans-spatial malformations.
Treatment
Of the 68 patients with HM, 40 patients were treated with percutaneous sclerotherapy using Bleomycin while 11 patients underwent trans-arterial embolization alone [Figure 1]. Eight patients were managed by a combination of percutaneous and trans-arterial approach. Surgical resection was performed in nine patients following percutaneous sclerotherapy [Figure 2]. The various approaches used in the treatment of the vascular anomalies are illustrated in Table 1 and the therapeutic agents used for sclerotherapy and embolization are illustrated in Table 2. All patients with VM [Figures 3 and 4], LM [Figure 5] and VLM were treated with sclerotherapy via percutaneous and/or permucosal instillation of sclerosant into the malformation. Some of the patients required multiple sclerotherapy sessions with the number of sessions depending on the size of the malformation.
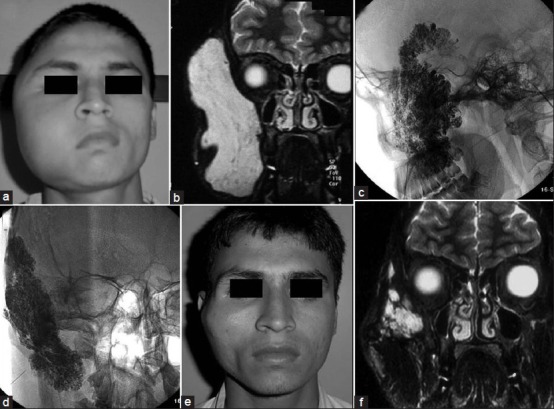
Figure 1.
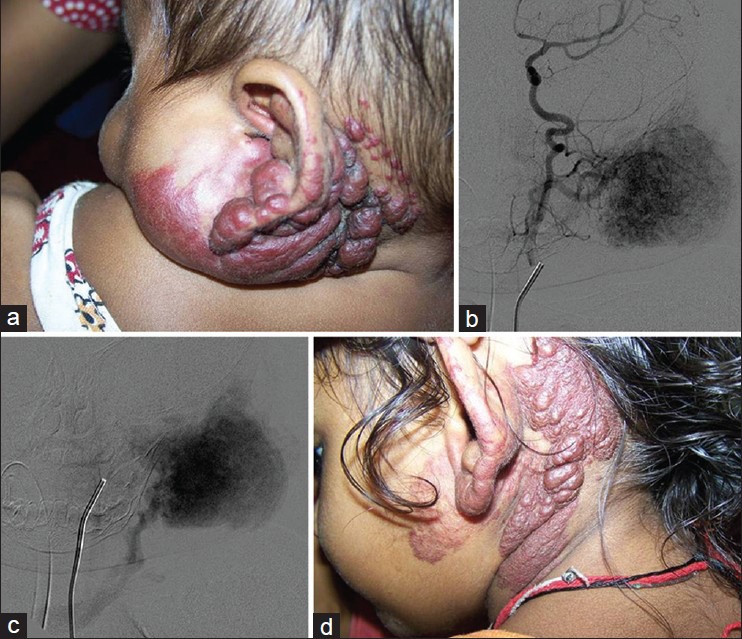
A 2-year-old female with left auricular and parotid region hemangioma treated with percutaneous intra-lesional Bleomycin; (a) Clinical photograph at presentation showing the hemangioma; (b) Left common carotid artery angiogram showing branches of the external carotid artery supplying the hemangioma; (c) Angiographic image showing persistent tissue staining characteristic of a hemangioma; (d) Clinical photograph after five treatment sessions showing reduction of the swelling. The therapeutic outcome was characterized as ‘complete resolution’
Figure 2.
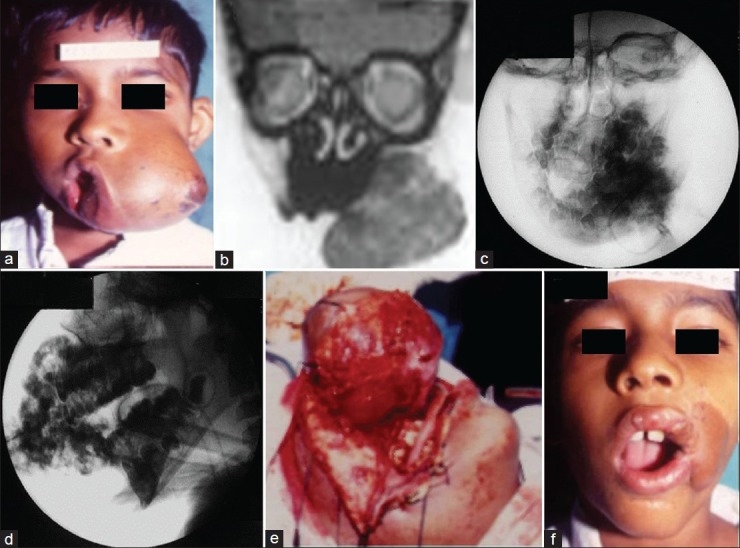
A 10-year-male with left cheek hemangioma treated with percutaneous glue embolization followed by surgical resection; (a) clinical photograph at presentation showing the large left cheek hemangioma; (b) preoperative coronal magnetic resonance imaging section showing the hemangioma; (c-d) plain radiographs during percutaneous glue embolization showing the glue cast in lateral and frontal views; (e) intraoperative photograph showing the hemangioma; (f) postoperative clinical photograph showing resolution of the left cheek swelling. The outcome was graded as ‘complete resolution’
Table 1.
Modalities used for the treatment of hemangiomas and venous malformations
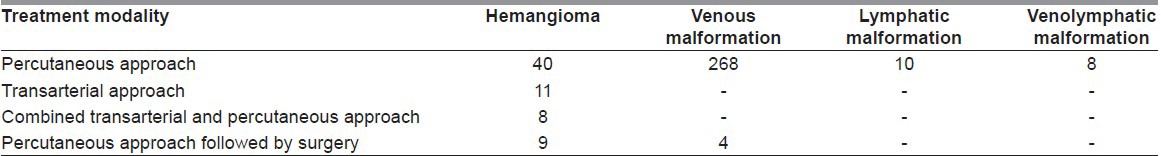
Table 2.
Therapeutic materials used for the treatment of hemangiomas and venous malformations
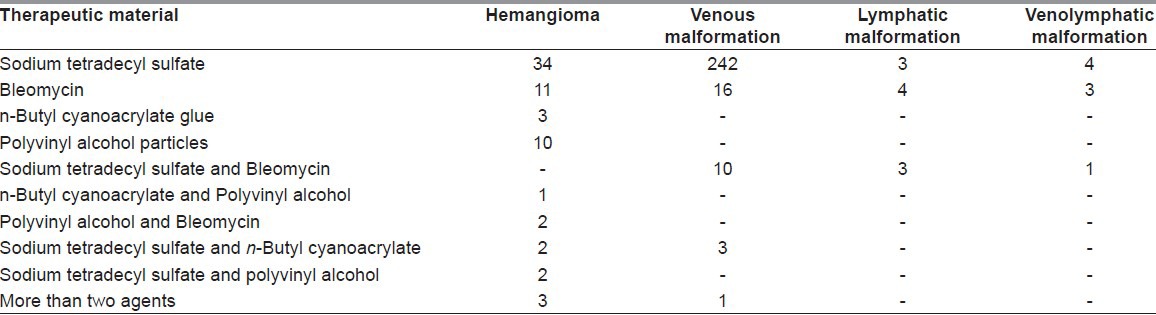
Figure 3.
A 22-year-male with right cheek venous malformation treated with sclerotherapy with Sodium Tetradecyl Sulfate; (a) Clinical photograph at presentation showing the right cheek swelling; (b) pre-operative T2 weighted coronal MRI section showing the T2 hyperintense malformation; (c-d) plain radiographs during sclerotherapy showing radiopaque contrast in the venous malformation; (e) clinical photograph 6 months after the last sclerotherapy session showing resolution of the swelling; (f) post-operative T2 weighted coronal MRI section showing resolution of the malformation
Figure 4.
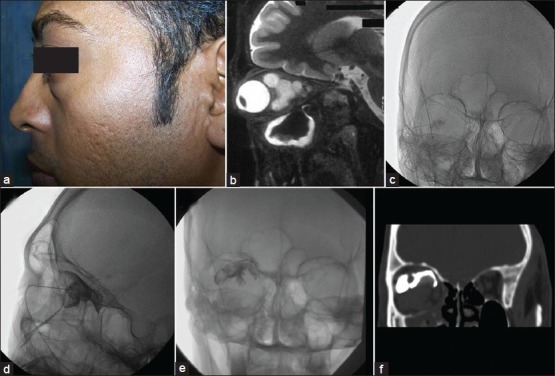
A 22-year-male with retro-ocular venous malformation treated with sclerotherapy with sodium tetradecyl sulfate mixed with lipiodol; (a) Clinical photograph at presentation showing right eye proptosis; (b) preoperative T2 weighted sagittal magnetic resonance imaging section showing the T2 hyperintense malformation; (c-d) Plain radiographs during sclerotherapy showing spinal puncture needle positioned in the malformation during injection of the sclerosing agent; (e) post-procedure plain radiograph showing the lipiodol cast; (f) post-procedure coronal computed tomography reconstruction image showing the lipiodol cast
Figure 5.
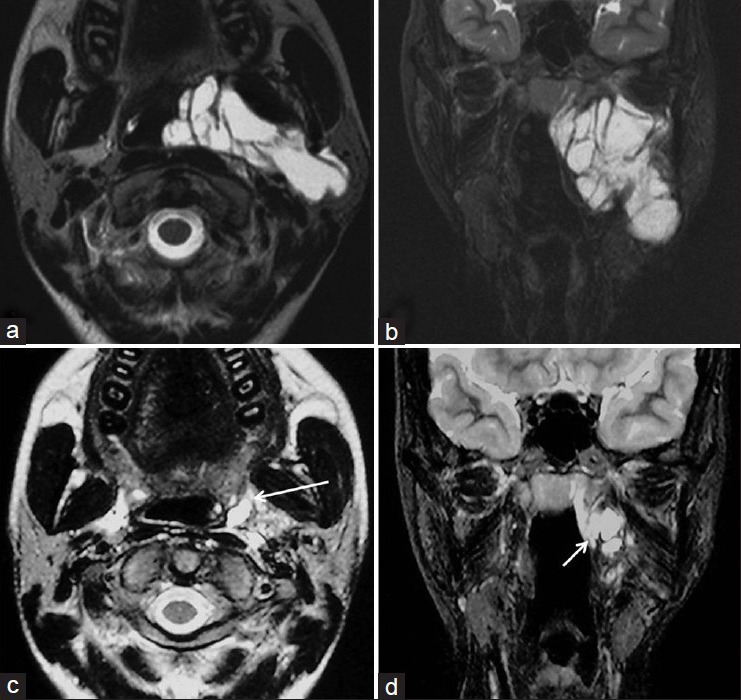
A 16-year-female with lymphatic malformation in the left parapharyngeal space treated with Bleomycin sclerotherapy; (a-b) Axial and coronal T2 weighted images showing the hyperintense lymphatic malformation; (c-d) Axial and coronal T2 weighted images after one session of percutaneous aspiration and Bleomycin sclerotherapy showing the residual lymphatic malformation (arrows)
Outcome
The follow-up duration in the study ranged from a minimum of 1.5 years to a maximum of 13 years, with the average follow-up duration being 4.7 years.
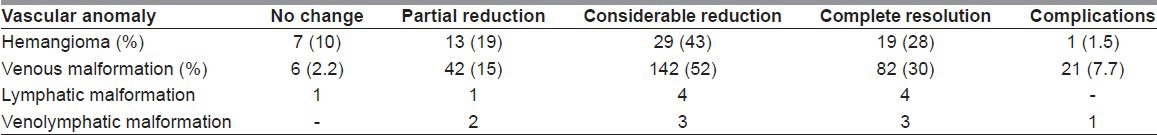
In the haemangioma group, various combinations of treatment modalities were used like transarterial PVA particle embolization followed by percutaneous or permucosal sclerotherapy. If surgery was planned, transarterial PVA particle embolization or percutaneous nBCA glue embolization was performed. Nine patients were treated like this and underwent surgery with good outcomes. Out of the 68 patients with HM, 48 patients (71%) had a more than 60% reduction of the swelling or complete cessation of bleeding, in patients where it was the presenting complaint. Cessation of bleeding was seen after the first session itself. Twenty patients (29%) had a less than 60% reduction of the swelling. In the low flow vascular malformation group, 82% patients had a good cosmetic outcome (>60% reduction in swelling), including large trans-spatial lesions. To summarize, a satisfactory outcome of treatment (>60% reduction in size) was seen in about 80% patients of HM and slow flow vascular malformations treated at our centre. The outcome of treatment of the different individual vascular anomalies is illustrated in Table 3.
Table 3.
Treatment outcome
Complications
Infection of the injection site was the commonest complication (2.8%, n = 10) followed by superficial skin necrosis (2.2%, n = 8) due to inadvertent extravascular injection of the sclerosing agent. Most of these were successfully managed with antibiotics except one patient who required reconstructive flap surgery. Other minor complications were skin blisters in a patient with VM of the cheek and radiating upper limb pain in a patient with VM of the neck. Both of these patients improved on conservative management.
Three major complications were observed in this study. One patient with cheek haemangioma, managed by trans-arterial particle embolization developed transient aphasia and hemiparesis which recovered over few hours. Another patient with extensive VM involving floor of the mouth developed uncontrolled bleeding from the permucosal puncture site. Cauterisation and surgical ligation of the bleeding malformation was performed with good outcome. Third patient with a large orbital VM, managed by direct puncture and sclerotherapy, developed increase in the swelling followed by raised intra-orbital pressure. The patient also developed glaucoma, vitreal and retinal haemorrhages. Emergency orbital decompression was performed. However, the patient developed corneal opacity and loss of vision in one eye.
DISCUSSION
Background
The management of vascular anomalies was plagued by confusion for many years. A lack of understanding of the pathophysiology had resulted in the evolution of confusing terminology to describe these lesions. This had affected the treatment of these lesions. Mulliken and Glowacki cleared the air in 1982 when they proposed a simplified classification system that divided the vascular anomalies into HM and the vascular malformations based on their endothelial cell characteristics and clinical behaviour.[1]
Majority of the HM involute spontaneously by 7 years of age.[2] Earlier, patients were advised watchful waiting in the hope of spontaneous involution. However, HM of the head and neck may cause problems that demand early intervention. Even otherwise, it is being increasingly realised that incomplete involution is not uncommon. Hence, the balance is shifting towards active treatment of HM.[6] Early intervention by trans-arterial embolization or sclerotherapy can be adjunctive or may even enhance the natural process of involution.
In our study, endovascular/percutaneous treatment of HM was successful in 71% of the patients. Complications were seen in 1.5% of patients. This demonstrates a good outcome and a low incidence of complications in a large sample size. Our results compare favourably with those of O’Donovan et al., who reported substantial improvement by sclerotherapy in about 83% of HM.[7] In another study, STD was injected intra-lesionally in 18 patients with HM, producing improvement in 16 patients.[8]
Vascular malformations
VMs, LMs and VLMs are slow flow malformations. These are effectively treated by percutaneous intra-lesional instillation of sclerosants.[9] Sclerotherapy has also been used in the treatment of HM. However, previous studies on sclerotherapy have been limited by small sample sizes.[10]
VMs were considered to be best managed by surgical excision.[6] However, surgery is associated with technical difficulties and complications. It may also leave behind scar marks.[3] Sclerotherapy is a good alternative for management of head and neck VMs. For smaller lesions, sclerotherapy alone can lead to cure or significant reduction in size while for larger lesions sclerotherapy may facilitate surgery by decreasing lesion size and blood loss.[6] Serious complications such as death and cardiovascular collapse that were earlier reported with the use of Ethanol have not been reported with the use of newer sclerosants like STD and Bleomycin.[7,8,11]
In the study by Yakes et al., Ethanol embolization of seven patients with VMs was done with a mean follow-up of 7 months. On serial colour doppler, persistent thrombosis of the vascular channels was seen in all patients. But, the cosmetic benefit to these patients has not been documented.[12] In another retrospective study by Lee et al., 87 patients with craniofacial VMs underwent Ethanol sclerotherapy. The results in this study were assessed on the basis of both clinical findings and change in the size of lesion on the baseline and follow-up MRI and whole body blood pool scintigram (WBBPS). Complete obliteration of the signs and symptoms with more than 75% uptake reduction on WBBPS or near complete resolution on MRI was observed in 32% patients.[13] Though, the assessment criteria for outcome are different than our study, this figure compares well with our study in which 30% of patients showed complete resolution (over 90% reduction in size) of their swelling. Any advantage that Ethanol might have over the newer sclerosing agents used in our study might have been offset by the additional MRI and WBBPS criteria used for the assessment of outcome in the former study.
In another study by Spence et al., 37 patients with facial VMs were treated by percutaneous sclerotherapy with Bleomycin. Subjective evaluation of outcome consisted of patient's as well as clinician's perception of response, categorized as worse, unchanged or better. Objective evaluation was carried out with post-treatment MRI as compared with pre-treatment MRI. Twenty-one patients showed a reduction in size on MRI. As per the subjective evaluation criteria, in 29 of 32 cases the patients and in 30 of 32 cases the clinicians thought that the lesions had improved. The authors considered Bleomycin sclerotherapy to be an effective treatment for VMs and concluded that MRI may not be required to demonstrate treatment benefits.[11] In our study, in about 98% cases of VMs, the clinicians thought that the lesions had improved.
Even large and trans-spatially extending head and neck VMs have been effectively treated by sclerotherapy. Wang et al., performed Ethanol sclerotherapy for large craniofacial VMs in 23 patients and documented over 75% reduction in swelling in 17 patients.[14] In the largest series published to date, outcome of sclerotherapy in 270 patients with craniofacial VMs was subjectively evaluated by patients themselves. An excellent or good outcome was seen in about 82% to 94% of patients depending on the sclerosing agent used.[15] A successful treatment outcome was seen in about 82% of patients with such VMs in our study.
Procedural complications were noted in 7.7% of patients with VM in our series. Spence et al., reported complications in four out of 32 patients in his study of patients with VM.[11] Wang et al., reported complications in four out of 23 of their patients with ethanol sclerotherapy.[15] In another retrospective review, blistering was the most common complication of Ethanol sclerotherapy and was seen in about 50% of patients.[16]
Lymphatic and veno-lymphatic malformations
Sclerotherapy remains the mainstay of treating LM in many centres.[6] In our study, sclerotherapy was successful in eight of the ten patients with LM and six of the eight patients with VLM. Peters et al., retrospectively reviewed 12 patients of LM treated with sclerotherapy using OK-432. In this study, six patients showed either an excellent or a good response. All of these patients had macrocystic LMs while all of the poor responders had microcystic malformations.[5] In another prospective study, all patients treated with doxycycline sclerotherapy had a favourable clinical response. However, this study had a small sample size of five patients, and only one of these had involvement of the head and neck region.[17]
CONCLUSION
Sclerotherapy for HM, VM and LM involving the head and neck is an effective treatment modality. The newer sclerosing agents like STD and Bleomycin used in this study have not shown any life threatening adverse effects. Though, complications are not uncommon, the procedure is reasonably safe. With our experience in such a large cohort group of patients, we suggest that percutaneous sclerotherapy with STD and Bleomycin be considered as the most effective and safe treatment modality for low flow vascular malformations involving the head and neck, including large trans-spatial lesions.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: A classification based on endothelial characteristics. Plast Reconstr Surg. 1982;69:412–22. doi: 10.1097/00006534-198203000-00002. [DOI] [PubMed] [Google Scholar]
- 2.Jackson IT, Carreño R, Potparic Z, Hussain K. Hemangiomas, vascular malformations, and lymphovenous malformations: Classification and methods of treatment. Plast Reconstr Surg. 1993;91:1216–30. doi: 10.1097/00006534-199306000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Jackson IT, Keskin M, Yavuzer R, Kelly CP. Compartmentalization of massive vascular malformations. Plast Reconstr Surg. 2005;115:10–21. [PubMed] [Google Scholar]
- 4.Chen WL, Yang ZH, Bai ZB, Wang YY, Huang ZQ, Wang YJ. A pilot study on combination compartmentalisation and sclerotherapy for the treatment of massive venous malformations of the face and neck. J Plast Reconstr Aesthet Surg. 2008;61:1486–92. doi: 10.1016/j.bjps.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Peters DA, Courtemanche DJ, Heran MK, Ludemann JP, Prendiville JS. Treatment of cystic lymphatic vascular malformations with OK-432 sclerotherapy. Plast Reconstr Surg. 2006;118:1441–6. doi: 10.1097/01.prs.0000239503.10964.11. [DOI] [PubMed] [Google Scholar]
- 6.Buckmiller LM, Richter GT, Suen JY. Diagnosis and management of hemangiomas and vascular malformations of the head and neck. Oral Dis. 2010;16:405–18. doi: 10.1111/j.1601-0825.2010.01661.x. [DOI] [PubMed] [Google Scholar]
- 7.O’Donovan JC, Donaldson JS, Morello FP, Pensler JM, Vogelzang RL, Bauer B. Symptomatic hemangiomas and venous malformations in infants, children, and young adults: Treatment with percutaneous injection of sodium tetradecyl sulfate. AJR Am J Roentgenol. 1997;169:723–9. doi: 10.2214/ajr.169.3.9275886. [DOI] [PubMed] [Google Scholar]
- 8.Woods JE. Extended use of sodium tetradecyl sulfate in treatment of hemangiomas and other related conditions. Plast Reconstr Surg. 1987;79:542–9. doi: 10.1097/00006534-198704000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Burrows PE, Mason KP. Percutaneous treatment of low flow vascular malformations. J Vasc Interv Radiol. 2004;15:431–45. doi: 10.1097/01.rvi.0000124949.24134.cf. [DOI] [PubMed] [Google Scholar]
- 10.Lee CH, Chen SG. Direct percutaneous ethanol instillation for treatment of venous malformation in the face and neck. Br J Plast Surg. 2005;58:1073–8. doi: 10.1016/j.bjps.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 11.Spence J, Krings T, terBrugge KG, da Costa LB, Agid R. Percutaneous sclerotherapy for facial venous malformations: Subjective clinical and objective MR imaging follow-up results. AJNR Am J Neuroradiol. 2010;31:955–60. doi: 10.3174/ajnr.A1940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yakes WF, Luethke JM, Parker SH, Stavros AT, Rak KM, Hopper KD, et al. Ethanol embolization of vascular malformations. Radiographics. 1990;10:787–96. doi: 10.1148/radiographics.10.5.2217971. [DOI] [PubMed] [Google Scholar]
- 13.Lee IH, Kim KH, Jeon P, Byun HS, Kim HJ, Kim ST, et al. Ethanol sclerotherapy for the management of craniofacial venous malformations: The interim results. Korean J Radiol. 2009;10:269–76. doi: 10.3348/kjr.2009.10.3.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang YA, Zheng JW, Zhu HG, Ye WM, He Y, Zhang ZY. Sclerotherapy of voluminous venous malformation in head and neck with absolute ethanol under digital subtraction angiography guidance. Phlebology. 2010;25:138–44. doi: 10.1258/phleb.2009.009019. [DOI] [PubMed] [Google Scholar]
- 15.Zhao JH, Zhang WF, Zhao YF. Sclerotherapy of oral and facial venous malformations with use of pingyangmycin and/or sodium morrhuate. Int J Oral Maxillofac Surg. 2004;33:463–6. doi: 10.1016/j.ijom.2003.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Berenguer B, Burrows PE, Zurakowski D, Mulliken JB. Sclerotherapy of craniofacial venous malformations: Complications and results. Plast Reconstr Surg. 1999;104:1–11. [PubMed] [Google Scholar]
- 17.Molitch HI, Unger EC, Witte CL, van Sonnenberg E. Percutaneous sclerotherapy of lymphangiomas. Radiology. 1995;194:343–7. doi: 10.1148/radiology.194.2.7529933. [DOI] [PubMed] [Google Scholar]


