Abstract
Loss of Achilles tendon combined with overlying soft tissue loss is a challenging problem. Multiple techniques like tendon graft with coverage by soft tissue flap or composite flaps have been used. All these options are technically demanding. Reports do exist whereby muscle flaps bridging the defect used as cover in course of time could transmit the tendon force across the defect. We are presenting a case where a free gracilis muscle flap used to cover the soft tissue defect at the Achilles tendon at 2 years follow up provided stable cover and produced active function of the Achilles tendon allowing the patient to stand tip toe. Mechanism of its action has been analysed by MRI and M-mode ultrasound. While in primary Achilles tendon injury reconstruction is still the recommended option, in complex situations mere filling of the gap with the flap without formal reconstruction of the tendon could give good functional outcome. This technique can be used in demanding situations.
KEY WORDS: Achilles tendon, gracilis, muscle flap, reconstruction
INTRODUCTION
Achilles tendon being the strongest tendon in the body plays a significant role in normal gait and its loss leads to a poor push off.[1] Combined segmental defects of Achilles tendon and overlying soft-tissues is frequently seen in road traffic accidents and secondary to infection occurring in the Achilles tendon region.
Various complex secondary reconstructive procedures for Achilles tendon and soft-tissue defects have been propagated by many authors and all claim equally good results.[1,2,3,4,5,6,7,8,9,10,11,12,13] Saunders, et al.,[14] have even suggested that if adequate wound healing is ensured by appropriate soft-tissue cover, good plantar flexion and even push off can be achieved, but no further investigations have been carried out to substantiate this.
We are reporting a case wherein free gracilis muscle flap was used to bridge the combined defect of Achilles tendon and overlying soft-tissue and the outcome was evaluated clinically and also by using dynamic B mode ultrasound and magnetic resonance imaging (MRI) scan.
CASE REPORT
Our patient was a 50-year-old manual labourer who sustained open injury to the Achilles tendon while at work and presented to us a week following the injury with severely infected wound. Thorough debridement of the wound resulted in a 20 cm long × 10 cm wide defect (200 cm2) and the defect was covered with a free gracilis muscle flap [Figure 1]. The muscle was placed longitudinally and was anchored to the surrounding skin. Vascular anastomosis was carried out to posterior tibial vessels. As it was an infected wound no formal attempt was made to reconstruct the tendon. At 2 years follow-up, we noted that patient was having a good active plantar flexion, was able to stand tip toe on both legs without any support, and had good push off and a near normal gait [Figure 2]. The movement of the ankle and Achilles tendon region was evaluated by using dynamic B-mode ultrasound, which was carried out with patient prone and the probe was kept over the region of reconstruction and the result showed that there is increased echogenic soft-tissue shadow in the deeper aspect of the muscle flap, which is filling the tendon defect suggestive of fatty change and the muscle was found to be merging with the Gastro-soleus myotendinous region proximally and to the residual tendon and to the calcaneum distally, and on active plantar flexion against resistance the muscle graft filling the defect was found to be shortening and transmitting the force of muscle action to the calcaneum [Figure 3]. MRI scan was also performed and the T2-weighted image showed that there is a tendon defect, which is being filled by the muscle graft and the deeper part of the muscle graft shows fatty change. The cleavage of the graft with the proximal myotendinous region and distal Achilles tendon is not visualised – suggestive of complete incorporation of the graft [Figure 4].
Figure 1.

The picture showing the soft tissue and Achilles tendon defect of the right leg after debridement and harvested gracilis muscle
Figure 2.

Follow-up at 2 years showing well settled flap and tip toe standing without any support on both legs
Figure 3.
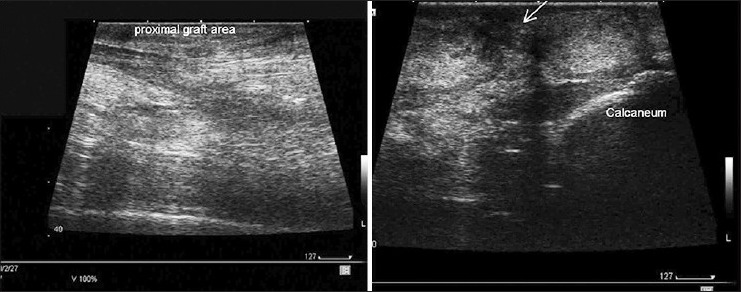
Ultrasound picture showing the tendon and graft interface proximally and distally
Figure 4.
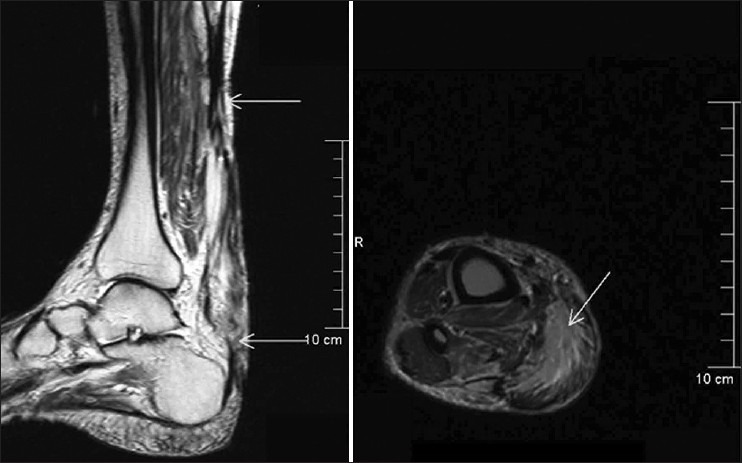
Magnetic resonance imaging T2-image showing the tendon defect, which is filled by the muscle graft and the deeper part of the muscle graft is in continuity with the proximal myotendinous region and distal Achilles tendon – suggestive of complete graft incorporation
DISCUSSION
Complex defects in the posterior ankle region with segmental defects of the Achilles tendon pose a reconstructive challenge.[2] Two modalities of treatment have been described. The classical method is to do tendon reconstruction using various tendon grafts along with soft-tissue cover using a local or free flap.[2,3,4,5,6,7,8,9] The second method is to use a composite graft of tendon and soft tissue together.[10,11,12,13,15] Infection further compounds the problem. Though ample options are available for the reconstruction, there have been complications when there is infection, which could be directly attributed to the tendon reconstruction component. Sporadic reports are available where sufficient results could be achieved without reconstruction.[14] If an adequate push off and a normal gait can be achieved by just providing a soft-tissue cover alone it can greatly reduce the morbidity and the operative time and a protocol could have been devised not to reconstruct Achilles tendon in infected complex defects. Our study shows that muscles, which are used to bridge the tendons, can align and function like a tendon. Similar results were reported by Jepegnanam, et al.,[16] when they used medial Gastrocnemius flap to bridge the gap in patella tendon and showed good knee extension. The outcome in our case could provide another option for surgeons to manage Achilles tendon defect in post infective conditions. In primary acute injuries still the standard options of reconstruction could be followed. The limitation of the report is that it is a single case report, but the outcome has been analysed well by MRI and M-mode ultrasound, which can provide enough confidence for anyone to try this solution in a demanding situation.
ACKNOWLEDGMENT
We thank Dr. Anupama NV, Dr. Kiruthika C, Department of Radiology, Ganga Hospital for helping with the imaging studies of the patient.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Fredrick MA. Traumatic disorders. In: Canale ST, Beaty JH, editors. Campbell's Operative Orthopaedics. 11th ed. Philadelphia: Mosby Elsevier; 2008. pp. 2753–8. [Google Scholar]
- 2.Jepegnanam TS, Nithyananth M, Boopalan PR, Cherian VM, Titus VT. Reconstruction of open contaminated Achilles tendon injuries with soft tissue loss. J Trauma. 2009;66:774–9. doi: 10.1097/TA.0b013e31817c96c7. [DOI] [PubMed] [Google Scholar]
- 3.Gopalakrishna A, Pavan Kumar TV. Twenty years’ follow-up of a de-epithelialised turnover flap. Indian J Plast Surg. 2008;41:211–3. doi: 10.4103/0970-0358.44944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bullocks JM, Hickey RM, Basu CB, Hollier LH, Kim JY. Single-stage reconstruction of Achilles tendon injuries and distal lower extremity soft tissue defects with the reverse sural fasciocutaneous flap. J Plast Reconstr Aesthet Surg. 2008;61:566–72. doi: 10.1016/j.bjps.2006.01.017. [DOI] [PubMed] [Google Scholar]
- 5.Fong EP, Papini RP, Mckiernan MV, Rao GS. Reconstruction of an Achilles tendon skin defect using a local fascial flap. Eur J Plast Surg. 1997;20:266–9. [Google Scholar]
- 6.Mohanty A, Jain P. Reconstructing and resurfacing open neglected Achilles tendon injury by distal posterior tibial artery based adipofascial flap. Eur J Plast Surg. 2004;27:196–9. [Google Scholar]
- 7.Lu TC, Lin CH, Lin CH, Lin YT, Chen RF, Wei FC. Versatility of the pedicled peroneal artery perforator flaps for soft-tissue coverage of the lower leg and foot defects. J Plast Reconstr Aesthet Surg. 2011;64:386–93. doi: 10.1016/j.bjps.2010.05.004. [DOI] [PubMed] [Google Scholar]
- 8.Huemer GM, Larcher L, Schoeller T, Bauer T. The free gracilis muscle flap in Achilles tendon coverage and reconstruction. Plast Reconstr Surg. 2012;129:910–9. doi: 10.1097/PRS.0b013e31824422da. [DOI] [PubMed] [Google Scholar]
- 9.Daniel NR. Managment of complications. In: Maffulli N, Almekinders LC, editors. The Achilles tendon. London: Spinger-Verlag Ltd; 2007. p. 210. [Google Scholar]
- 10.Deiler S, Pfadenhauer A, Widmann J, Stützle H, Kanz KG, Stock W. Tensor fasciae latae perforator flap for reconstruction of composite Achilles tendon defects with skin and vascularized fascia. Plast Reconstr Surg. 2000;106:342–9. doi: 10.1097/00006534-200008000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Dabernig J, Shilov B, Schumacher O, Lenz C, Dabernig W, Schaff J. Functional reconstruction of Achilles tendon defects combined with overlaying skin defects using a free tensor fasciae latae flap. J Plast Reconstr Aesthet Surg. 2006;59:142–7. doi: 10.1016/j.bjps.2005.07.011. [DOI] [PubMed] [Google Scholar]
- 12.Babu V, Chittaranjan S, Abraham G, Korula RJ. Single-stage reconstruction of soft-tissue defects including the Achilles tendon using the dorsalis pedis arterialized flap along with the extensor digitorum brevis as bridge graft. Plast Reconstr Surg. 1994;93:1090–4. doi: 10.1097/00006534-199404001-00033. [DOI] [PubMed] [Google Scholar]
- 13.Lee JW, Yu JC, Shieh SJ, Liu C, Pai JJ. Reconstruction of the Achilles tendon and overlying soft tissue using antero-lateral thigh free flap. Br J Plast Surg. 2000;53:574–7. doi: 10.1054/bjps.2000.3407. [DOI] [PubMed] [Google Scholar]
- 14.Saunders DE, Hochberg J, Wittenborn W. Treatment of total loss of the Achilles tendon by skin flap cover without tendon repair. Plast Reconstr Surg. 1978;62:708–12. doi: 10.1097/00006534-197811000-00008. [DOI] [PubMed] [Google Scholar]
- 15.Ronel DN, Newman MI, Gayle LB, Hoffman LA. Recent advances in the reconstruction of complex Achilles tendon defects. Microsurgery. 2004;24:18–23. doi: 10.1002/micr.10191. [DOI] [PubMed] [Google Scholar]
- 16.Jepegnanam TS, Boopalan PR, Nithyananth M, Titus VT. Reconstruction of complete knee extensor mechanism loss with gastrocnemius flaps. Clin Orthop Relat Res. 2009;467:2662–7. doi: 10.1007/s11999-009-0735-8. [DOI] [PMC free article] [PubMed] [Google Scholar]


