Abstract
Craniosynostosis is a premature pathologic fusion of one or more cranial vault sutures that leads to abnormal shape of the skull. The fused sutures lead to restricted growth in some areas and compensatory bossing in other areas. The head may assume different shapes depending upon the site and timing of the abnormally fused suture. The exact cause of this suture pathology is still unknown, but the local dura, cranial base and the fibroblast growth factors seem to influence this. The diagnosis rests on clinical examination and confirmation is generally on the computed tomography scan. The need for surgery is both for cosmetic and functional reasons. Many cases may be associated with raised intracranial pressure with its attendant deleterious effects on vision and brain. The aim of treatment is to increase the cranial volume and reshape the skull. The surgery can be safely undertaken around 9-12 months in most of the cases. The conventional management is through an open surgical approach; although, some centres have claimed impressive results with limited endoscopic techniques in selected cases. The review article deals with the aetiopathogenesis, clinical presentations and management of the common varieties of craniosynostoses seen in the Indian scenario.
KEY WORDS: Abnormal skull shapes, cosmetic and functional issues, cranioplasty, fronto-orbital advancement, premature suture fusion
INTRODUCTION
Craniosynostosis is premature fusion of one or more cranial sutures leading to abnormal shape of the skull. In a newborn, the brain develops at a rapid rate in the initial periods: Its size doubles during the first 6 months and quadruples by the 1st year of life. The brain acquires 80% of its adult size by 2nd year of life. This rapid brain growth is allowed by the patent cranial sutures in the growing child. The growing brain itself provides a stimulus for keeping the sutures patent. It has been found that a minimal pressure of approximately 5 mm Hg from the growing brain is required to stimulate new bone deposition at the suture margins.[1]
Some people feel it is better to label craniosynostosis as ‘absence of cranial sutures’ rather than ‘premature fusion’ as most of the ‘fusion’ occurs during the intrauterine period.[1]
The abnormal shape of the skull has been known since antiquity. Hippocrates was aware of the abnormal shape of the skull[2] and Sommerring,[3] observed that bone growth in the skull occurred primarily at suture lines and abnormal skull shape develop if the suture was replaced by bone.
In 1851, Virchow hypothesised about the pattern of growth across a fused suture.[3] Observations of Crouzon[4] and Apert and Bigot,[5] from 1910 to 1920 established that in many cases, the facial deformities and abnormal skull shape are associated with a myriad of other features. These clinical entities are now named after them.
DEVELOPMENT OF SKULL
The normal skull development begins around 23-26 day of gestation.[6] The bone is formed by intramembranous ossification in the cranial vault and endochondrial ossification at the cranial base. This process involves mesenchymal cell proliferation and subsequent differentiation into osteoblasts at the bone margins. The ‘suture’ is the ‘meeting point’ of the osteogenic fronts of two adjacent bones. The maintenance of a suture relies on sufficient new bone cells being recruited into the bone fronts as well as undifferentiated cells within the suture.[7,8]
The calvarial sutures play an important role in allowing mouldability of the head during the parturition to allow normal delivery. In the postnatal period, these sutures allow the much needed growth of the infant brain that almost doubles in volume in the first 6 months. The sutures serve as growth sites where new bone is deposited in response to the continuing separation of the osteogenic fronts between the opposing bones.[9] Premature closure of these sutures leads to restriction of growth along the sutures and can lead to morphological changes that can result in various skull deformities.[10,11,12]
The cause of premature closure of sutures is still controversial. Virchow believed,[13] this is due to abnormality in the suture itself, whereas Moss blamed the abnormal development of the cranial base, which affects the suture through the dural attachment.[14] However, the sequence of events leading to premature ossification of sutures is unknown. Biomechanical forces and genetically determined local expression of growth factors have been implicated in the aetiology of craniosynostosis.[12,15] Delashaw et al., further describes compensatory growth, listing four fundamental factors that explain compensatory growth patterns.[16]
Cranial vault bones that are prematurely fused act as a single bone plate with decreased growth potential
Abnormal asymmetric bone deposition occurs at perimeter sutures with increased bone deposition directed away from the bone plate
Perimeter sutures adjacent to the prematurely fused suture compensate in growth more than perimeter sutures distant to the sutural stenosis
A non-perimeter suture that is contiguous to the prematurely fused suture undergoes enhanced symmetric bone deposition along both edges.
These events lead to the development of abnormal shapes of the skull depending upon the timing, location and multiplicity of the sutures involved. The orbital shape and volume may be affected leading to exophthalmoses or corneal exposure and ocular muscle imbalance. It has been found that intracranial pressure (ICP) may be raised (more than 17 mm Hg on lumber puncture) in about 14% of single suture involvement. This may be increased to about 40% in multiple suture involvement.[17] The raised ICP is attributed to the decreased cranial capacity and disproportion between cerebrospinal fluid production and egress.[18] Sleep apnoea resulting from mid-facial retrusion can induce episodic nocturnal elevations in ICP secondary to the dilating effects of hypercapnia on the cerebral vasculature. Another potential cause is venous hypertension resulting from stenosis or complete closure of the sigmoid/jugular sinus complex.[19]
The appearance of the normal sutures in a newborn infant is shown in Figure 1. Three of the five major cranial sutures are paired, i.e., coronal, lambdoid and squamosal. The other two sutures sagittal and metopic are single. There are some minor facial region sutures, the frontonasal, frontoethmoid and frontosphenoidal sutures, which are also commonly affected in craniosynostosis. The metopic suture fuses between 9 months and 2 years of age. The lambdoid, sagittal and coronal sutures fuse around 40 years of age. Sutures normally fuse from back to front and lateral to medial except the metopic, which fuses from front to back.[20]
Figure 1.
The sutures in a normal infant
Physical examination is very important in the diagnosis of craniosynostosis. The normal head has an egg shape, being widest in the parietal area posterior to the ears with a narrower, gently rounded forehead. The shape of the skull is altered depending upon the suture (s) that get prematurely fused. The skull will assume a shape that is characteristic of the suture involved (vide infra). Head circumference and cephalic index (CI) are adjunctive measurements that may support the diagnosis. CI is based on maximal cranial length and maximal cranial width:
CI = Wd/L×100
Where Wd is the maximal cranial width and L is the maximal cranial length.[21]
The normal ratio is 76:81. Anything less than 76 is labelled as dolichocephalic and above 81 is labelled as brachycephaly.
PATHOLOGY
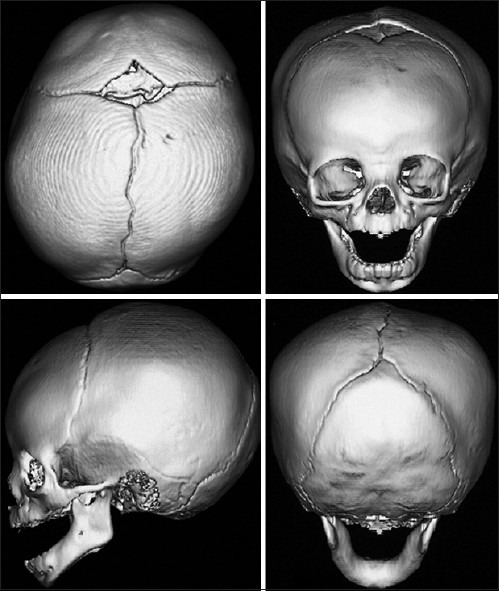
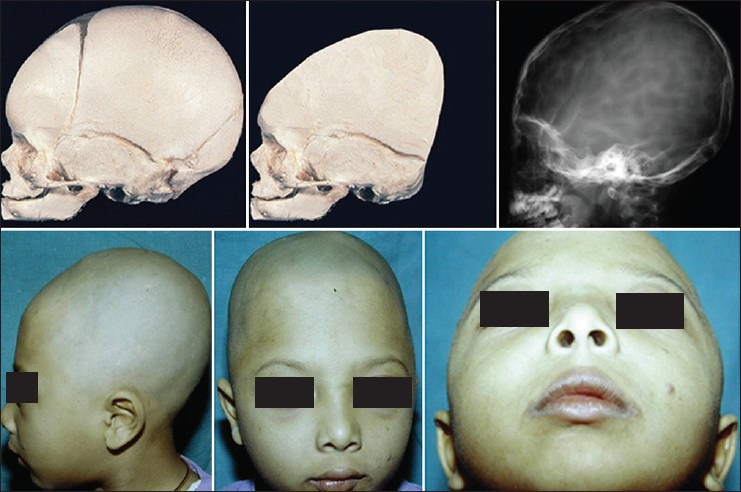
The unilateral coronal suture fusion leads to flattening of the fronto-parietal region on the affected side and is clinically known as plagiocephaly. The ipsilateral eyebrow is raised and there is widening of the palpebral fissure on the affected side. The nasal root gets deviated to the ipsilateral side and the chin is displaced to the contra lateral side. The contra lateral forehead and ipsilateral temporal region bossing is seen. The orbit on the affected side shows vertical orientation and the so called harlequin sign is positive. The computed tomography (CT) scan would confirm all these findings [Figure 2].
Figure 2.
Schematic pathogenesis of frontal plagiocephaly. The upper row shows abnormal fusion of unilateral coronal suture. The middle row shows the appearance of fused suture in the computed tomography scan. Lower row shows clinical appearance in a 1-year-old child
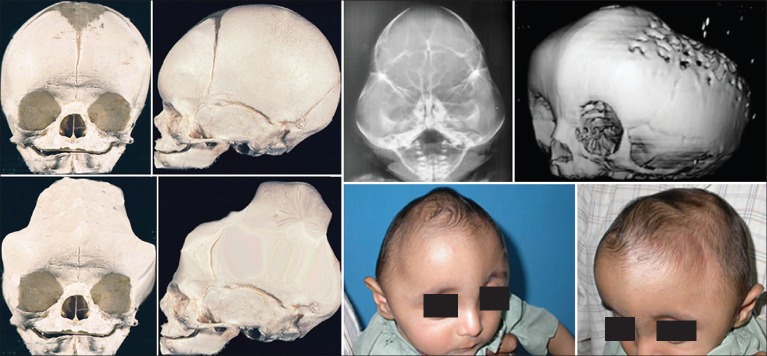
It is important to differentiate the frontal synostotic plagiocephaly from the positional plagiocephaly that may happen because of deformation of the skull either during the birth or because of the child lying in one particular position for a very long time. In addition, infants have limited ability to move their head in the first few months of life because of their weak neck muscles. The presence of torticollis may further pre-dispose to positional plagiocephaly [Figure 3]. The skull outline in deformational plagiocephaly is of a parallelogram, whereas it is trapezoidal in synostotic plagiocephaly. There are many distinguishing features between these two conditions [Table 1].
Figure 3.

A case of positional plagiocephaly showing (upper row) and unilateral frontal synostotic plagiocephaly (lower row)
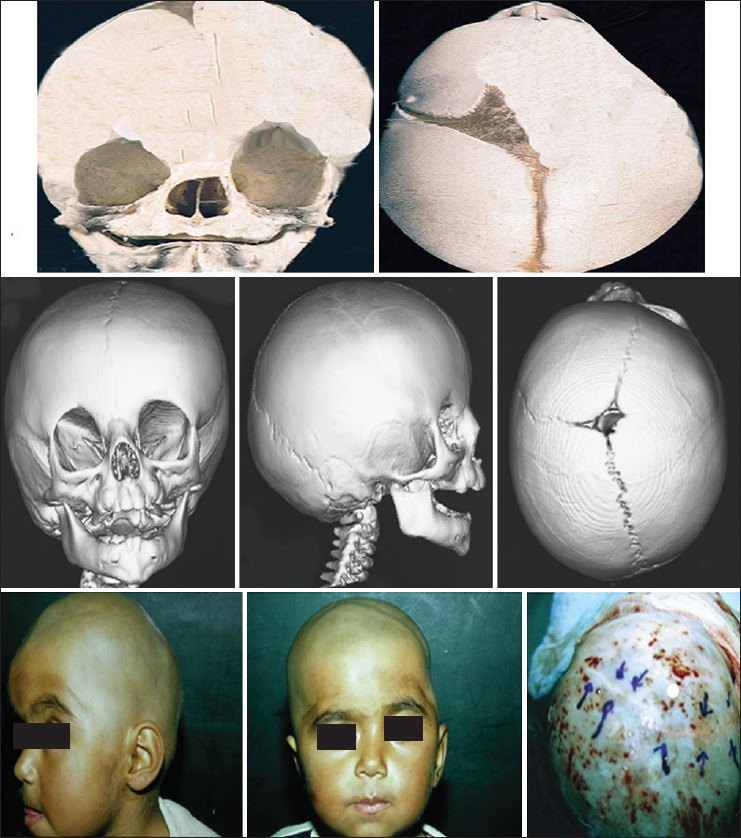
Table 1.
Differences between deformational and synostotic frontal plagiocephaly
Bilateral closure of the coronal suture produces a diminished growth vector in the ventral-dorsal direction and compensatory growth takes place in the medial-lateral direction. This results in brachycephaly. There is bilateral recession of the fronto-orbital bar leading to prominent eyes. In severe cases, even exorbitism can result. Bilateral frontal bossing is present in most of the cases. CT scan reveals fused bilateral coronal sutures and the short skull in the anteroposterior dimensions [Figure 4]. Sometimes the skull may grow in the vertical direction in response to growth along the parieto-temporal suture to give the appearance of a tower and is then known as turricephaly [Figure 5].
Figure 4.
Schematic pathogenesis of bilateral coronal suture fusion and the appearance on plain X-ray skull (upper row). Lower row shows showing appearance in a 9 months old child. The computed tomography scan shows bilateral fused coronal suture
Figure 5.
Schematic pathogenesis of turricephaly deformity (upper row). The X-ray skull shows thumb printing indicative of raised intracranial pressure. The clinical appearance in a 3-years-old child (lower row)
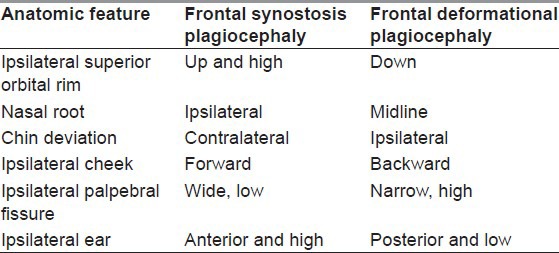
A premature closure of the sagittal suture results in the continuing growth of the calvarium in the antero posterior direction and diminished growth in the transverse direction, causing the skull to appear like a boat and is known as scaphocephaly. The CT scan would show fused sagittal suture. The skull is both narrow and long [Figure 6].
Figure 6.
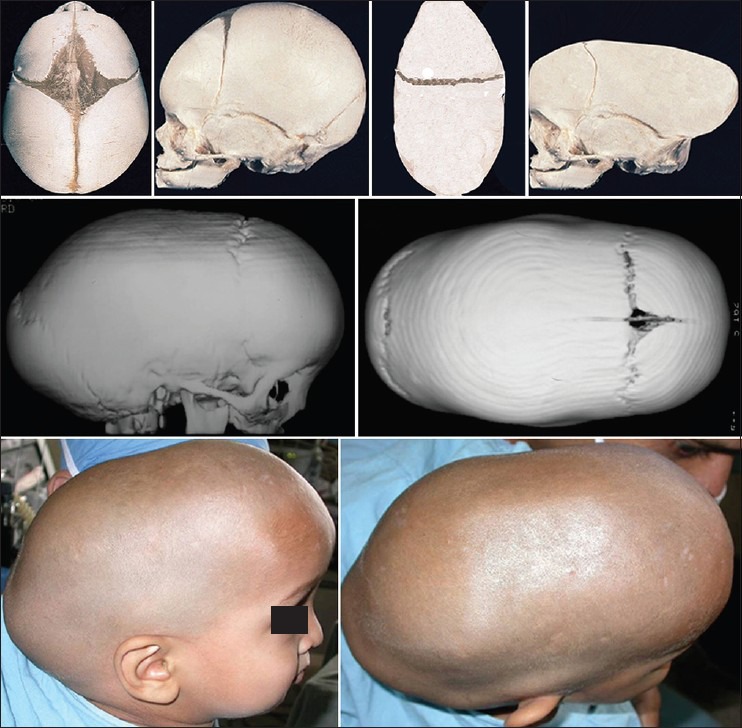
(Upper row) Schematic pathogenesis of scaphocephaly; (middle row) computed tomography scan showing long and narrow skull. Lower row: Clinical appearance in a patient
A pathologically closed metopic suture results in the absence of the transverse growth of both the frontal bones, leading to a narrow forehead. This anterior narrowing appears as a triangle and is known as trigonocephaly. There is decreased growth in the intercanthal region and resulting in hypotelorism [Figure 7].
Figure 7.
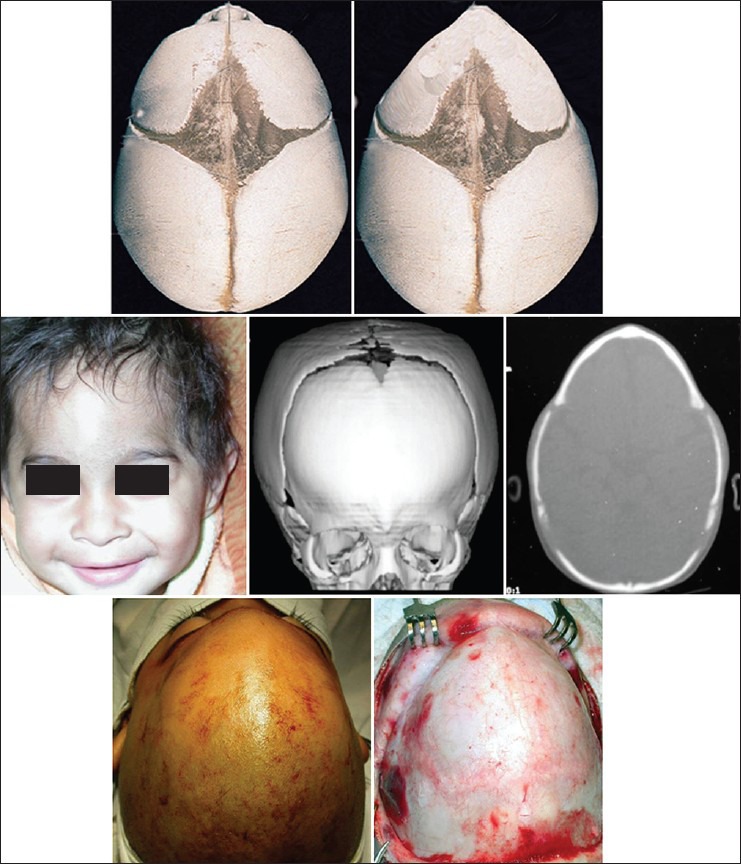
Schematic pathogenesis of metopic suture synostosis (upper row). Narrow forehead seen in a child with computed tomography scan showing triangualar forehead (middle row). Lower row showing pointed forehead on operation
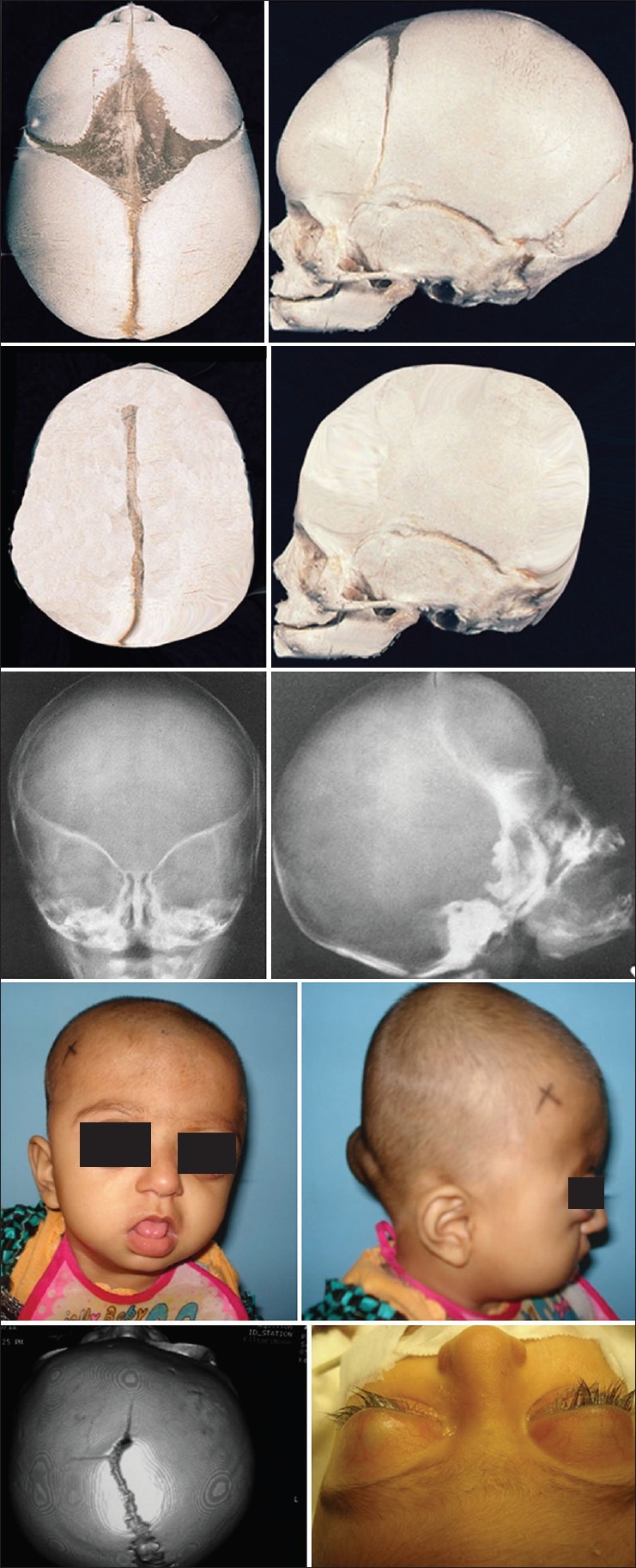
In clover leaf deformity, there is multiple suture involvement and the skull assumes the shape of a trifoliate clover leaf [Figure 8].
Figure 8.
Schematic pathogenesis of clover leaf deformity (upper row). Plain X-ray skull and 3D computed tomography (CT) showing the deformity the CT also shows thinning of the calvarium because of raised intracranial pressure (middle row). The lower row shows clover leaf deformity in a 9 months old child
Premature closure of the lambdoid suture leads to occipital plagiocephaly with ipsilateral flattening of the occipital region and contralateral bulging.
SYNDROMIC VERSUS NON-SYNDROMIC CRANIOSYNOSTOSIS
The craniosynostosis can occur as an isolated sporadic event or may appear as an associated event with syndromes such as Apert, Crouzon, Carpenter, Pfifer, etc., Multiple sutures are involved in syndromic cases. These patients also have mid-face hypoplasia and limb and trunkal deformities.
Sometimes the sutures can be prematurely closed because of poor development of the brain (microcephaly); this can be diagnosed on the basis of a magnetic resonance imaging showing poor sulci and gyri. These patients will also have delayed milestones. It is important to distinguish cases of microcephaly from primary craniosynostosis as surgical intervention is not indicated in such the former.
INDICATIONS FOR SURGERY
The need for surgery is both for cosmetic and functional reasons. The misshaped skull can lead to body image problems later in life. In some cases, there can be raised ICP. This is likely to happen in about 40% cases when multiple sutures are involved as in syndromic cases. The aim of treatment is to restore normal appearance of the skull and increase the cranial volume so that the growing brain can be accommodated without any pressure effects on vital structures. Moreover, an uncorrected continued calvarial deformity can lead to abnormalities in the cranial base. The consensus is to operate around 9-12 months of age. The surgical risk is much less as the child is in a better position to withstand surgery at this age as compared with in the first few months after birth. The infant skull bones are still quite pliable at this age and can be moulded into the appropriate shape rather easily. The small bony defects that invariably result from various cranioplasties and advancements get ossified easily at this age.
SURGICAL MANAGEMENT
The principles of management are to increase the cranial volume, reshape the cranial vault and to perform fronto-orbital advancement to correct any recessed supraorbtal rims. The skull bones can be divided into many parts and these parts may be rearranged to give natural appearing shape. Some areas may need to have onlay bone grafting by using split cranial bone grafts. Any accompanying abnormalities such as orbital shape and size or orbital dystopias can also be addressed at the same time.
The surgical correction is undertaken through a combined intracranial and extracranial approach. A bi-frontal craniotomy is performed. The fronto-orbital consisting of supraorbital band and part of orbital roof and lateral orbital wall is also removed. The abnormal shape of the calvarium is corrected; the fronto-orbital segment can also be manipulated to correct the deformities on the side table (“bench surgery”). The corrected calvarium and frontorbital segment is then repositioned in an advanced position. The small defects that may result from advancement are left as such as these ossify rapidly in these children.
The need for re-operation in craniosynostosis patients can always arise and this is more so in case of syndromal cases. These syndromal cases would also require advancement at le fort 1 and le fort 3 levels for correction of mid-face deformities. Previously these cases required extensive surgical procedures, but with the recent availability of sophisticated distraction techniques, the surgery has become less extensive and produces better soft-tissue and bony correction. Many patients of syndromic craniosynostosis such as Aperts and Carpenter syndromes have syndactyly of the hands and feets and the concomitant correction needs to be started around 1 year of age.
PLAGIOCEPHALY
The aim of treatment here is a correction of recessed forehead and the supraorbital margins. The affected orbit also needs to be expanded horizontally and the vertical height may also be a need to be reduced. It has been found that a bilateral frontal craniotomy accords the best opportunity to correct this deformity. Figure 9 shows the pre-operative appearance in a child and post-operative result after 5 years.
Figure 9.

A plagiocephaly patient (upper row) showing clinical features. The middle row shows fused coronal suture on one side. The fronto-orbital segment shows recessed segment on affected side. The post-operative appearance at 6 years later (lower row)
In cases of accompanying orbital dystopia and deviation of the root of the nose, the orbital and nasal osteotomies may be needed for correction [Figure 10].
Figure 10.

Plagiocephaly patient with orbital dystopia and laterally deviated nasal skeleton (upper row) Intraoperative pictures showing expansion of the recessed frontal bar and expanded orbital socket and corrected nasal skeleton (middle row) post-operative pictures showing corrected deformities (lower row)
Brachycephaly
The skull is short in anteroposterior diameter and there is frontal bossing along with supraorbital recession. Bilateral fronto-orbital advancement is carried out and bone grafts are added to increase the length of the calvarium [Figure 11].
Figure 11.

A case of brachycephaly (upper row); increase in length of calvarium achieved by using bone grafts (middle row). The post-operative pictures show improved cranial length (lower row)
In some cases of brachycephaly, the skull may grow vertically to assume tower shaped appearance and is still short in anteropsterior dimension. This can be corrected by dividing the calvarial portion into many segments and rotating them appropriately as shown achieve good results. Figure 12 shows the method of correction and post-operative result at 15 years.
Figure 12.

A case of turricephaly (upper row) corrected by re-arranging the calvarial segments (middle row). The post-operative appearance 15 years later (lower row)
METOPIC SYNOSTOSIS
There is supra orbital recession and the forehead is wedge shaped. There is some degree of hypotelorism present in these cases. The forehead needs to be expanded by adding bone; the contour is corrected by scoring the frontal segment. The hypotelorism is corrected by placing a wedge of bone in the intercanthal region [Figure 13].
Figure 13.
A case of metopic synostosis (upper row) showing corrected frontal bone segments (middle row). 1 year post-operative pictures at 1 year period
SCAPHOCEPHALY
The aim of treatment is expansion of the calvarium in the transverse dimension; this is carried out by performing zigzag osteotomies in such a way that the calvarial width can be increased by moving the segments laterally on either side [Figure 14]. The resultant bony defect is grafted by using bone from the calvarium itself. Barrel staving is performed in the temporal regions to match the expanded calvarium.
Figure 14.

A case of scaphocephaly (upper row) managed by expanding the calvarium by zigzag osteotomies (middle row). The appearance at 3 years post-operative period (lower row)
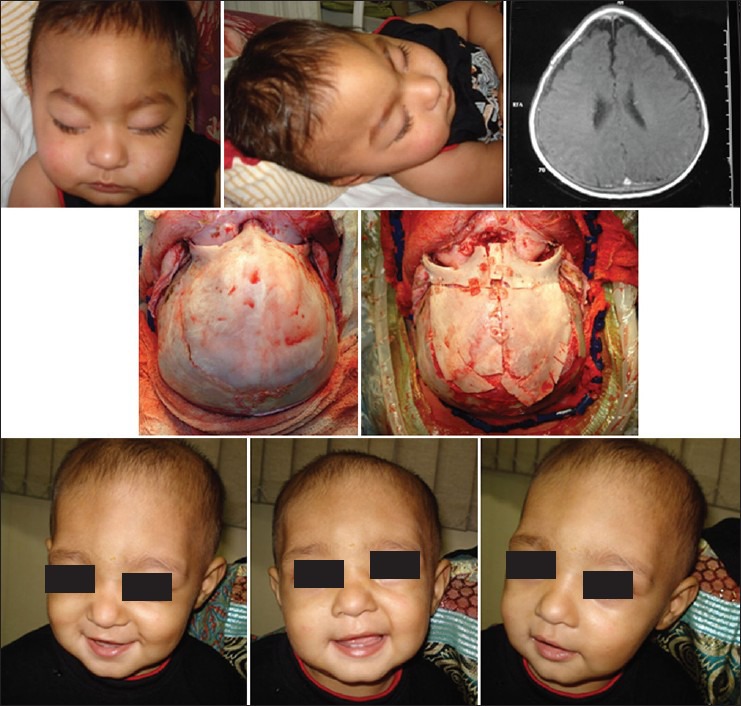
In clover leaf deformity, multiple sutures are involved and all of these need to be addressed. The calvarium can be divided into many segments and these are rearranged to give a more acceptable shape. Figure 15 shows the pre-operative appearance at age of 9 months and late post-operative results at the age of 10 years.
Figure 15.

A case of clover leaf deformity showing intraoperative correction of the bony calvarial segments (upper and middle row). Post-operative appearance at 9 years post-operative period (lower row)
The mid-face hypoplasia is very common in syndromic cases such as Crouzon's and Aperts and these patients would require correction by advancements at the le fort levels. Figure 16 shows a case of Crouzon's syndrome who underwent distraction at the level of both le fort 1 and le fort 3 level.
Figure 16.
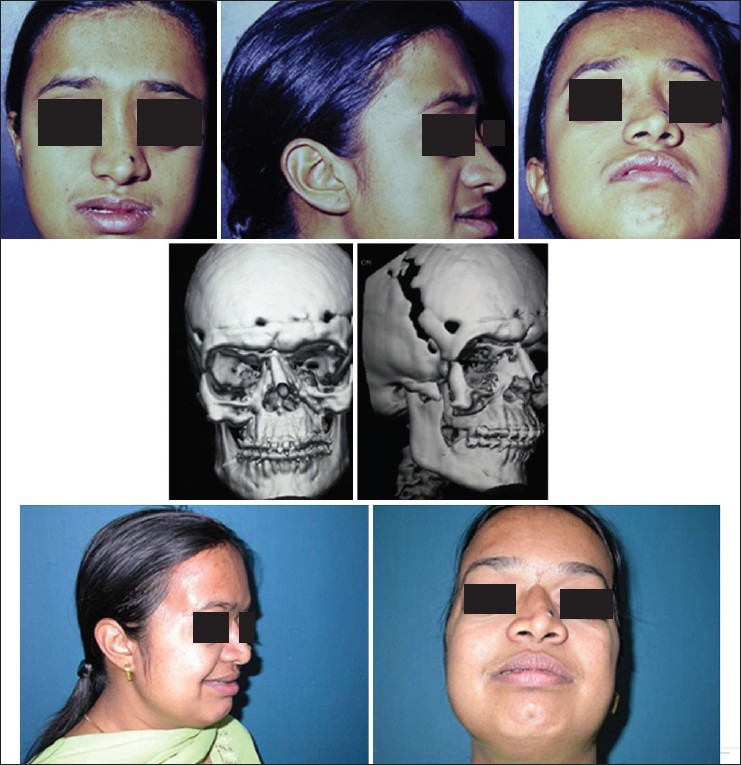
A case of Crouzon's syndrome operated for fronto-orbital advancement earlier (upper row) underwent mid-face advancement at le fort 1 and 3 levels (middle row). Lower row shows 2 years post-operative appearance
Newer techniques of management
A relatively new adjunct used in the treatment of single suture synostosis entails slow active bone movement aided by springs. It has been most commonly reported for management of sagittal synostosis.[22]
Distraction osteogenesis is another technique to reposition cranial vault bones gradually while encouraging intervening bone fill between segments.[23] These techniques are still not very popular and are used in selected centres in select cases only.
Post-operative complications
These patients can have moderate amount of blood loss during the surgery and this needs to be replaced quickly as these children have very little reserve. The airway may be difficult especially in syndromic patients and these children need to be kept in the paediatric intensive care units for at least first 24 h. The extradural dead space created because of the advancements generally gets filled up by the expanding brain in a few weeks’ time.
The incidence of infection has been reported to be around 3-6%.[24]
The mortality has been reported to be around 2.2-0.1% and these fall with experience.[25] In our centre, the mortality has been about 2% in 84 cases.
Prognosis and outcomes
Non-syndromic craniosynostosis patients if operated early have very good post-operative outcome and the need for the second surgery is minimal. However, in syndromic cases the re operation rates are quite high, to the tune of about 2-13%.[26]
There are no long-term assessments of cognitive function; however, some studies suggest a correlation between early surgery and higher IQ scores (although, these retrospective study cannot show causation).[27]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Pattisapu JV, Gegg CA, Olavarria G, Johnson KK, Ruiz RL, Costello BJ. Craniosynostosis: Diagnosis and surgical management. Atlas Oral Maxillofac Surg Clin North Am. 2010;18:77–91. doi: 10.1016/j.cxom.2010.08.002. [DOI] [PubMed] [Google Scholar]
- 2.Dimopoulos VG, Kapsalakis IZ, Fountas KN. Skull morphology and its neurosurgical implications in the Hippocratic era. Neurosurg Focus. 2007;23:E10. doi: 10.3171/foc.2007.23.1.10. [DOI] [PubMed] [Google Scholar]
- 3.Alden TD, Lin KY, Jane JA. Mechanisms of premature closure of cranial sutures. Childs Nerv Syst. 1999;15:670–5. doi: 10.1007/s003810050456. (Quoted Sömmerring ST. Vom Baue des menschlichen Körpers, 2nd edn. Leipzig: Voss; 1839.) and Virchow R. Ueber den Cretinismus, namentlich in Franken, und ueber pathologische) [DOI] [PubMed] [Google Scholar]
- 4.Crouzon O. Dysostose cranio-faciale héréditaire. Bull Mem Soc Med Hop Paris 7. 1921;33:545–55. [Google Scholar]
- 5.Apert E, Bigot A. Dysostose cranio-faciale hereditaire (type Crouzon) (presentation de malades) Bull Mem Soc Med Hop Paris. 1921;45:1717–9. [Google Scholar]
- 6.Ursitti F, Fadda T, Papetti L, Pagnoni M, Nicita F, Iannetti G, et al. Evaluation and management of nonsyndromic craniosynostosis. Acta Paediatr. 2011;100:1185–94. doi: 10.1111/j.1651-2227.2011.02299.x. [DOI] [PubMed] [Google Scholar]
- 7.Albright AL, Byrd RP. Suture pathology in craniosynostosis. J Neurosurg. 1981;54:384–7. doi: 10.3171/jns.1981.54.3.0384. [DOI] [PubMed] [Google Scholar]
- 8.Coussens AK, Wilkinson CR, Hughes IP, Morris CP, van Daal A, Anderson PJ, et al. Unravelling the molecular control of calvarial suture fusion in children with craniosynostosis. BMC Genomics. 2007;8:458. doi: 10.1186/1471-2164-8-458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baer MJ. Patterns of growth of the skull as revealed by vital staining. Hum Biol. 1954;26:80–126. [PubMed] [Google Scholar]
- 10.Enlow DH. Normal craniofacial growth. In: Cohen MM Jr, editor. Craniosynostosis: Diagnosis, Evaluation and Management. New York: Raven; 1986. pp. 131–56. [Google Scholar]
- 11.Enlow DH. Normal craniofacial growth. In: Cohen MM Jr, MacLean RE, editors. Craniosynostosis: Diagnosis, Evaluation and Management. 2nd ed. New York: Oxford University Press; 2000. pp. 35–50. [Google Scholar]
- 12.Cohen MM. Sutural pathology. In: Cohen MM Jr, MacLean RE, editors. Craniosynostosis: Diagnosis, Evaluation and Management. 2nd ed. New York: Oxford University Press; 2000. [Google Scholar]
- 13.Persing JA, Jane JA, Shaffrey M. Virchow and the pathogenesis of craniosynostosis: A translation of his original work. Plast Reconstr Surg. 1989;83:738–42. doi: 10.1097/00006534-198904000-00025. [DOI] [PubMed] [Google Scholar]
- 14.Moss ML. Functional anatomy of cranial synostosis. Childs Brain. 1975;1:22–33. doi: 10.1159/000119554. [DOI] [PubMed] [Google Scholar]
- 15.Mulliken JB, Warman ML. Molecular genetics and craniofacial surgery. Plast Reconstr Surg. 1996;97:666–75. doi: 10.1097/00006534-199603000-00030. [DOI] [PubMed] [Google Scholar]
- 16.Delashaw JB, Persing JA, Broaddus WC, Jane JA. Cranial vault growth in craniosynostosis. J Neurosurg. 1989;70:159–65. doi: 10.3171/jns.1989.70.2.0159. [DOI] [PubMed] [Google Scholar]
- 17.Renier D, Sainte-Rose C, Marchac D, Hirsch JF. Intracranial pressure in craniostenosis. J Neurosurg. 1982;57:370–7. doi: 10.3171/jns.1982.57.3.0370. [DOI] [PubMed] [Google Scholar]
- 18.Inagaki T, Kyutoku S, Seno T, Kawaguchi T, Yamahara T, Oshige H, et al. The intracranial pressure of the patients with mild form of craniosynostosis. Childs Nerv Syst. 2007;23:1455–9. doi: 10.1007/s00381-007-0436-0. [DOI] [PubMed] [Google Scholar]
- 19.Warren SM, Proctor MR, Bartlett SP, Blount JP, Buchman SR, Burnett W, et al. Parameters of care for craniosynostosis: Craniofacial and neurologic surgery perspectives. Plast Reconstr Surg. 2012;129:731–7. doi: 10.1097/PRS.0b013e3182412a50. [DOI] [PubMed] [Google Scholar]
- 20.Fernbach SK, Naidich TP. Radiological evaluation of craniosynostosis. In: Cohen MM, editor. Craniosynostosis: Diagnosis, Evaluation and Management. New York: Raven Press; 1986. [Google Scholar]
- 21.Bennaceur S, Petavy-Blanc AS, Chauve J, et al. Human cephalic morphology. In: Laffont A, Durieuz F, editors. Anthropometry. Elsevier: Encyclopédie Médicochirurgicale; 2005. pp. 85–103. [Google Scholar]
- 22.Lauritzen C, Sugawara Y, Kocabalkan O, Olsson R. Spring mediated dynamic craniofacial reshaping. Case report. Scand J Plast Reconstr Surg Hand Surg. 1998;32:331–8. doi: 10.1080/02844319850158697. [DOI] [PubMed] [Google Scholar]
- 23.Hirabayashi S, Sugawara Y, Sakurai A, Harii K, Park S. Frontoorbital advancement by gradual distraction. Technical note. J Neurosurg. 1998;89:1058–61. doi: 10.3171/jns.1998.89.6.1058. [DOI] [PubMed] [Google Scholar]
- 24.Fearon JA, Yu J, Bartlett SP, Munro IR, Chir B, Whitaker L. Infections in craniofacial surgery: A combined report of 567 procedures from two centers. Plast Reconstr Surg. 1997;100:862–8. doi: 10.1097/00006534-199709001-00006. [DOI] [PubMed] [Google Scholar]
- 25.Czerwinski M, Hopper RA, Gruss J, Fearon JA. Major morbidity and mortality rates in craniofacial surgery: An analysis of 8101 major procedures. Plast Reconstr Surg. 2010;126:181–6. doi: 10.1097/PRS.0b013e3181da87df. [DOI] [PubMed] [Google Scholar]
- 26.McCarthy JG, Glasberg SB, Cutting CB, Epstein FJ, Grayson BH, Ruff G, et al. Twenty-year experience with early surgery for craniosynostosis: I. Isolated craniofacial synostosis: Results and unsolved problems. Plast Reconstr Surg. 1995;96:272–83. doi: 10.1097/00006534-199508000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Arnaud E, Meneses P, Lajeunie E, Thorne JA, Marchac D, Renier D. Postoperative mental and morphological outcome for nonsyndromic brachycephaly. Plast Reconstr Surg. 2002;110:6–12. doi: 10.1097/00006534-200207000-00002. [DOI] [PubMed] [Google Scholar]


