Abstract
Background. Although periampullary diverticulum is usually asymptomatic and discovered incidentally in patients during endoscopic retrograde cholangiopancreatography (ERCP), it may lead to post-ERCP morbidity. We compared baseline characteristics and clinical data as well as ERCP results in patients with and without periampullary diverticulum. Methods. Clinical, laboratory, and ERCP data of 780 patients referred to the Taleghani Hospital, as a great referral endoscopy center, in Iran were prospectively analyzed. Results. The periampullary diverticulum was identified in 44 patients (5.6%). Cannulation of common bile duct was more failed in patients with diverticulum compared to others (35.5% versus 11.5, P < 0.001). Patients with diverticulum had eight times more often common bile duct stone compared to patients without diverticulum (54.5% versus 12.2%, P < 0.001). Post-ERCP complications were observed in 2.3% and 4.2% of patients with and without diverticulum, respectively, which did not significantly differ in both groups. Conclusion. Because of more failure cannulation in the presence of periampullary diverticulum, ERCP requires more skills in these patients. Prevalence of common bile duct stone was notably higher in patients with diverticulum; therefore, more assessment of bile stone and its complications in these patients is persistently recommended.
1. Introduction
Periampullary diverticulum is commonly situated on the second part of the duodenum and usually occurred in the elderly, with a slight female preponderance [1, 2]. It is usually caused by the progression of duodenal motility disorders. Furthermore, progressive weakening of intestinal smooth muscles and increased intraduodenal pressure have been known as main underlying etiologies for this defect [3]. The incidence of this finding widely varies from 1% to 32.8% based on different diagnostic approaches such as barium graphs, endoscopic retrograde cholangiopancreatography (ERCP) evaluation, and autopsy series [4–7]. Although periampullary diverticulum is usually asymptomatic and discovered incidentally in patients during ERCP, its association with various pathological conditions such as choledocholithiasis, perforation, pancreatitis, bleeding, CBD obstruction, and rarely carcinoma has been well recognized in various studies [8–12]. One of the most important problems to the endoscopists is the impact of these diverticula on the success of therapeutic or diagnostic ERCP procedures. In some reports, cannulation difficulty during ERCP was associated with the presence of periampullary diverticulum [3] and, in some others, it was related to higher risk of retained stones in the common bile duct [5]. However, some other studies could not find a relationship between the presence of diverticulum and any technical difficulties at ERCP. Moreover, successful cannulation was achieved in 88.8% to 97% of patients with diverticulum [2, 11, 12]. Therefore, more studies should be performed with the aim to determine the ERCP success rate and its related complications in patients with periampullary duodenal diverticulum.
We assessed and compared baseline characteristics and clinical data as well as ERCP results and complications in patients with and without periampullary diverticulum.
2. Materials and Methods
The study was approved by institutional review board of the Shahid Beheshti University of Medical Sciences. Patients between the ages of 15 and 99 with the diagnosis of hepatobiliary diseases and candidate for ERCP referred to Taleghani referral hospital between 2009 and 2012 were eligible and underwent diagnostic and therapeutic ERCP procedure. Patients with these criteria were ineligible: age below 15 years, acute illness such as hypotension, hypoxia, oxygen saturation less than 95% on supplemental oxygen, and hemodynamic instability. Patients with surgically altered anatomy (Billroth II or Roux-en-Yanastomosis) were also excluded as cannulation technique is then fundamentally different from that in normal anatomy.
Participants classified as one of the two groups: patients were diagnosed periampullary diverticulum following ERCP (as the case group) and those without this finding (as the reference group). Data describing patient characteristics such as demographic characteristics, medical history, and clinical presentations were collected from patients recorded files and by interviewing in the day of admission to hospital if required. Laboratory parameters were also measured in the day of admission that consisted of cell blood count and liver function tests. Eligible patients underwent ERCP for suspected and diagnosed pancreatobiliary disease on the basis of generally accepted diagnostic indications for ERCP [13]. Procedure was performed under conscious sedation with midazolam and meperidine and by a gastroenterologist. Cannulation was performed on the basis of techniques as previously described [14]. Successful cannulation was defined as free and deep instrumentation of the biliary tree and a cannulation attempt was defined as sustained contact with the cannulating device and the papilla for at least five seconds [15]. Difficult biliary cannulation was also related to the failure of biliary access despite ten minutes of attempted biliary cannulation, or more than five attempted unintentional pancreatic cannulations [16]. Post-ERCP complications include at least one of these post-ERCP pancreatitis, gastrointestinal perforation, and bleeding.
Comparisons of categorical variables across the groups were performed using an overall chi-square test or Fisher's exact test if required, while comparisons of continuous variables were performed using a t-test or Mann-Whitney test. The role of the presence of periampullary diverticulum for predicting common bile duct stone and also biliary cannulation failure was assessed by linear regression analysis adjusting for confounders. Model calibration was estimated using the Hosmer-Lemeshow (HL) goodness-of-fit statistic (higher P values imply that the model fits the observed data better). The data analyzer was anonymous, and data collection and processing were approved by the institutional review board of the university.
P values of 0.05 or less were considered statistically significant. All the statistical analyses were performed using SPSS version 15.0 (SPSS Inc., Chicago, IL, USA) and SAS version 9.1 for Windows (SAS Institute Inc., Cary, NC, USA).
3. Result
A total of 780 patients underwent ERCP that of these 44 patients had periampullary diverticulum. At baseline (Table 1), there was no difference in male-to-female ratio between the two study groups, and patients with diverticulum were older than the patients without this finding (66 versus 57-year old, P = 0.001). Regarding medical history, there were no significant differences in the overall incidence rates for hypertension, diabetes mellitus, current smoking, and family history of coronary artery disease between the patients with diverticulum and control group. Also, two groups were similar in terms of previous history of ERCP, cholecystectomy, and biliary stone. With regard to laboratory parameters (Table 2), levels of serum total and direct bilirubins as well as liver enzymes were lower in the group with diverticulum.
Table 1.
Baseline characteristics and medical history in the group with periampullary diverticulum and the control group.
| Characteristics | Diverticulum group (n = 44) | Control group (n = 736) | P value |
|---|---|---|---|
| Male/female | 18/26 | 375/361 | 0.193 |
| Age (years) | 65.9 ± 16.0 | 57.0 ± 17.1 | 0.001 |
| Medical history: | |||
| Diabetes mellitus | 8 (18.2) | 81 (11.0) | 0.146 |
| Hypertension | 8 (18.2) | 133 (18.1) | 0.985 |
| Coronary artery disease | 5 (11.4) | 58 (7.9) | 0.410 |
| Cigarette smoking | 4 (9.1) | 93 (12.6) | 0.489 |
| Cholecystectomy | 20 (45.5) | 263 (35.7) | 0.193 |
| Previous ERCP | 3 (6.8) | 67 (9.1) | 0.606 |
| Biliary stone | 4 (9.1) | 76 (10.3) | 0.999 |
Data are presented as mean ± SD or n (%).
Table 2.
Pre-ERCP laboratory parameters in the group with periampullary diverticulum and the control group.
| Laboratory parameters | Diverticulum group (n = 44) | Control group (n = 736) | P value |
|---|---|---|---|
| AST | 55.5 ± 46.0 | 87.5 ± 92.2 | 0.019 |
| ALT | 61.5 ± 55.9 | 112.7 ± 205.9 | 0.015 |
| ALP | 656.0 ± 753.5 | 832.3 ± 795.5 | 0.051 |
| Lactate dehydrogenase | 435.8 ± 229.7 | 465.4 ± 330.1 | 0.812 |
| Total bilirubin | 3.2 ± 6.6 | 6.6 ± 9.0 | 0.006 |
| Direct bilirubin | 2.0 ± 4.2 | 3.6 ± 5.2 | 0.025 |
| Serum amylase | 187.2 ± 211.7 | 167.7 ± 356.2 | 0.311 |
Data are presented as mean ± SD.
Successful biliary cannulation was achieved in 64.5% of the patients with periampullary diverticulum and in 88.5% of patients without this finding (P < 0.001) that in 19.3% and 12.0% of them was difficulty performed, respectively (Figure 1). Cannulation of common bile duct was also more failed in patients with diverticulum compared to others (35.5% versus 11.5, P < 0.001). Multivariable logistic regression analysis (Table 3) also confirmed that the presence of periampullary diverticulum could predict the failed biliary cannulation (OR = 6.287, 95% CI = 2.458–16.083, P < 0.001).
Figure 1.
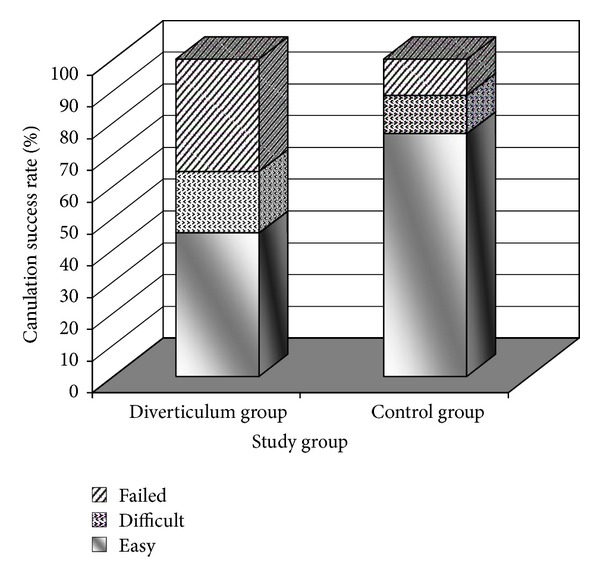
Success and failure rate of cannulation in the group with periampullary diverticulum and the control group.
Table 3.
Multivariable regression analysis of the predicting effect of periampullary diverticulum on failed biliary cannulation with the presence of confounders.
| Item | Multivariate P value | Odds ratio | 95% CI | |
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| Presence of diverticulum | <0.001 | 6.287 | 2.458 | 16.083 |
| Advanced age | 0.123 | 0.985 | 0.966 | 1.004 |
| Hypertension | 0.201 | 0.634 | 0.315 | 1.275 |
| Coronary artery disease | 0.192 | 0.576 | 0.251 | 1.318 |
| Cholecystectomy | 0.058 | 1.896 | 0.979 | 3.674 |
| Serum total bilirubin | 0.056 | 0.972 | 0.943 | 1.001 |
Hosmer-Lemeshow goodness of fit: χ 2 = 6.239, P = 0.621.
Those who had cannulation failure underwent needle knife precutting or fistulotomy regarding operators' preference. All of them had successful cannulation by these techniques.
In univariate analysis, patients with diverticulum had more common bile duct stone compared to patients without diverticulum (54.5% versus 12.2%, P < 0.001). Multivariable analysis (Table 4) also showed that the group with periampullary diverticulum had six times more often common bile duct stone in comparison with another group (OR = 6.450, 95% CI = 3.159–13.167, P < 0.001).
Table 4.
Multivariable regression analysis of the predicting effect of periampullary diverticulum on common bile duct stone with the presence of confounders.
| Item | Multivariate P value | Odds ratio | 95% CI | |
|---|---|---|---|---|
| Lower limit | Upper limit | |||
| Presence of diverticulum | <0.001 | 6.450 | 3.159 | 13.167 |
| Male gender | 0.832 | 1.049 | 0.673 | 1.634 |
| Advanced age | 0.018 | 0.983 | 0.970 | 0.997 |
| Serum total bilirubin | <0.001 | 1.081 | 1.035 | 1.129 |
Hosmer-Lemeshow goodness of fit: χ 2 = 4.240, P = 0.835.
There were no significant differences between the diverticulum and control groups in term of ERCP-related complications such as pancreatitis (2.3% versus 2.7%), bleeding (0.0% versus 0.3%), gastrointestinal perforation (0.0% versus 0.6%), and cholangitis (0.0% versus 0.5%) (Figure 2).
Figure 2.
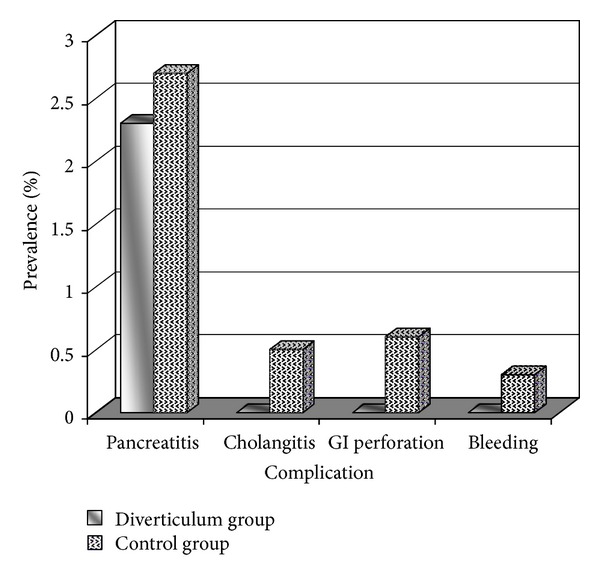
ERCP-related complications in the group with periampullary diverticulum and the control group.
4. Discussion
The current study first focused on the incidence of periampullary diverticulum among the patients who were candidate for ERCP. This phenomenon was found in 5.6% of our participants that was considerably lower than most previous studies. Some researches could confirm that high prevalence of diverticula was attributed to the higher age [2, 3, 11], and this relationship was reconfirmed in the present study since the mean age of patients was significantly higher in those with periampullary diverticulum than others (66 years versus 57 years, resp.). The discrepancy between the reported incidences of periampullary diverticulum can be also the result of differences in operator experience for detecting periampullary diverticulum. Furthermore, despite relationship of the incidence of diverticulum with female gender predominance [1, 17], this relation was not found in our study. It seems that the increased creation of periampullary diverticulum is mainly associated with advanced age, whereas its higher prevalence among women may not be reported in all studies among different population.
We showed that the presence of diverticulum significantly increased the difficulty and failure of biliary cannulation. Similarly, in a study by Lobo et al., diverticulum was a major cause of failed ERCP, especially in patients with intradiverticular papillae in comparison with juxtapapillary diverticula [3], whereas, in some other studies, the finding of a periampullary diverticulum during an ERCP was suggested as an indicator of an easier cannulation attempt [11, 12]. The various techniques for cannulation can be responsible for explaining higher cannulation failure rate. A low cannulation rate can be also attributed to the inability of the endoscopist to detect the papilla in a substantial percentage of cases with duodenal diverticula. Also, when the papilla is located deep inside the diverticulum, often lying at the bottom, the cannulation used to be difficult.
In the present study, the group with periampullary diverticulum had six times more often common bile duct stone in comparison with another group. It is similar other studies evaluated periampulary diverticula. Kennedy and Thompson indicated that patients with biliary stone were 2.6 times more likely to have a periampullary diverticulum than patients without this finding [18]. Rajnakova et al. also found that patients with diverticulum presented 1.8-times more often with retained stone in the common bile duct than patients without diverticulum [5]. Moreover, Tham and Kelly found bile duct stones in 64% of patients with diverticula compared with 33% of the controls, with an odds ratio of 3.6 [6]. Formation of biliary stone in the presence of periampullary diverticula can be related to several probable hypotheses. First, it has been proposed that the dysfunction in the sphincter of Oddi, which in turn causes reflux of pancreatic fluid and intestinal content that lead to biliary stone formation [7]. It has been also argued that diverticula cause spasm of the sphincter and increase biliary tract pressure. This phenomenon may produce jaundice and cholangitis as well as predispose for CBD lithiasis [19]. Also, it has been hypothesized that periampullary diverticula may cause functional biliary stasis possibly by compression of the distal part of the common bile duct that accounts for the increased incidence of pigment biliary stones [20, 21]. Although we were able to demonstrate an association between the presence of periampullary duodenal diverticulum and choledocholithiasis, pathological basis of this phenomenon is already undetermined and should be supported by further studies.
In summary, although the incidence of periampullary diverticulum in our study population is lower than most previous reports, its related female predominance as well as high cannulation failure is considerable. Because of more failure cannulation in the presence of periampullary diverticulum, ERCP requires more skills in these patients. Prevalence of common bile duct stone was notably higher in patients with diverticulum; therefore, more assessment of bile stone and its complications in these patients is persistently recommended.
References
- 1.Leivonen MK, Halttunen JAA, Kivilaakso EO. Duodenal diverticulum at endoscopic retrograde cholangiopancreatography, analysis of 123 patients. Hepato-Gastroenterology. 1996;43(10):961–966. [PubMed] [Google Scholar]
- 2.Boix J, Lorenzo-Zúñiga V, Añaños F, Domènech E, Morillas RM, Gassull MA. Impact of periampullary duodenal diverticula at endoscopic retrograde cholangiopancreatography: a proposed classification of periampullary duodenal diverticula. Surgical Laparoscopy, Endoscopy and Percutaneous Techniques. 2006;16(4):208–211. doi: 10.1097/00129689-200608000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Lobo DN, Balfour TW, Iftikhar SY. Periampullary diverticula: consequences of failed ERCP. Annals of the Royal College of Surgeons of England. 1998;80(5):326–331. [PMC free article] [PubMed] [Google Scholar]
- 4.Zoepf T, Zoepf D-S, Arnold JC, Benz C, Riemann JF. The relationship between juxtapapillary duodenal diverticula and disorders of the biliopancreatic system: analysis of 350 patients. Gastrointestinal Endoscopy. 2001;54(1):56–61. doi: 10.1067/mge.2001.115334. [DOI] [PubMed] [Google Scholar]
- 5.Rajnakova A, Goh PMY, Ngoi SS, Lim SG. ERCP in patients with periampullary diverticulum. Hepato-Gastroenterology. 2003;50(51):625–628. [PubMed] [Google Scholar]
- 6.Tham TCK, Kelly M. Association of periampullary duodenal diverticula with bile duct stones and with technical success of endoscopic retrograde cholangiopancreatography. Endoscopy. 2004;36(12):1050–1053. doi: 10.1055/s-2004-826043. [DOI] [PubMed] [Google Scholar]
- 7.Yildirgan MI, Başoğlu M, Yilmaz I, et al. Periampullary diverticula causing pancreaticobiliary disease. Digestive Diseases and Sciences. 2004;49(11-12):1943–1945. doi: 10.1007/s10620-004-9597-9. [DOI] [PubMed] [Google Scholar]
- 8.Dennison AR, Watkins RM, Sarr MJ, Lee ECG. Adenocarcinoma complicating a duodenal diverticulum. Journal of the Royal College of Surgeons of Edinburgh. 1987;32(1):44–46. [PubMed] [Google Scholar]
- 9.Oddo F, Chevallier P, Souci J, et al. Aspects radiologiques des complications des diverticules duodenaux. Journal of Radiology. 1999;80(2):134–140. [PubMed] [Google Scholar]
- 10.Yoneyama F, Miyata K, Ohta H, Takeuchi E, Yamada T, Kobayashi Y. Excision of a juxtapapillary duodenal diverticulum causing biliary obstruction: report of three cases. Journal of Hepato-Biliary-Pancreatic Surgery. 2004;11(1):69–72. doi: 10.1007/s00534-003-0854-7. [DOI] [PubMed] [Google Scholar]
- 11.Tyagi P, Sharma P, Sharma BC, Puri AS. Periampullary diverticula and technical success of endoscopic retrograde cholangiopancreatography. Surgical Endoscopy and Other Interventional Techniques. 2009;23(6):1342–1345. doi: 10.1007/s00464-008-0167-7. [DOI] [PubMed] [Google Scholar]
- 12.Panteris V, Vezakis A, Filippou G, Filippou D, Karamanolis D, Rizos S. Influence of juxtapapillary diverticula on the success or difficulty of cannulation and complication rate. Gastrointestinal Endoscopy. 2008;68(5):903–910. doi: 10.1016/j.gie.2008.03.1092. [DOI] [PubMed] [Google Scholar]
- 13.Silviera ML, Seamon MJ, Porshinsky B, et al. Complications related to endoscopic retrograde cholangiopancreatography: a comprehensive clinical review. Journal of Gastrointestinal and Liver Diseases. 2009;18(1):73–82. [PubMed] [Google Scholar]
- 14.Lee TH, Park DH, Park J-Y, et al. Can wire-guided cannulation prevent post-ERCP pancreatitis? A prospective randomized trial. Gastrointestinal Endoscopy. 2009;69(3):444–449. doi: 10.1016/j.gie.2008.04.064. [DOI] [PubMed] [Google Scholar]
- 15.Bailey AA, Bourke MJ, Williams SJ, et al. A prospective randomized trial of cannulation technique in ERCP: effects on technical success and post-ERCP pancreatitis. Endoscopy. 2008;40(4):296–301. doi: 10.1055/s-2007-995566. [DOI] [PubMed] [Google Scholar]
- 16.Kaffes AJ, Sriram PVJ, Rao GV, Santosh D, Reddy DN. Early institution of pre-cutting for difficult biliary cannulation: a prospective study comparing conventional versus a modified technique. Gastrointestinal Endoscopy. 2005;62(5):669–674. doi: 10.1016/j.gie.2005.05.022. [DOI] [PubMed] [Google Scholar]
- 17.Waugh JM, Johnston EV. Primary diverticula of the duodenum. Annals of Surgery. 1955;141(2):193–200. doi: 10.1097/00000658-195502000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kennedy RH, Thompson MH. Are duodenal diverticula associated with choledocholithiasis? Gut. 1988;29(7):1003–1006. doi: 10.1136/gut.29.7.1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hagege H, Berson A, Pelletier G, et al. Association of juxtapapillary diverticula with choledocholithiasis but not with cholecystolithiasis. Endoscopy. 1992;24(4):248–251. doi: 10.1055/s-2007-1010476. [DOI] [PubMed] [Google Scholar]
- 20.Miyazaki S, Sakamoto T, Miyata M, Yamasaki Y, Yamasaki H, Kuwata K. Function of the sphincter of Oddi in patients with juxtapapillary duodenal diverticula: evaluation by intraoperative biliary manometry under a duodenal pressure load. The World Journal of Surgery. 1995;19(2):307–312. doi: 10.1007/BF00308647. [DOI] [PubMed] [Google Scholar]
- 21.Shinagawa N, Fukui T, Mashita K, Kitano Y, Yura J. The relationship between juxtapapillary duodenal diverticula and the presence of bacteria in the bile. The Japanese Journal of Surgery. 1991;21(3):284–291. doi: 10.1007/BF02470948. [DOI] [PubMed] [Google Scholar]


