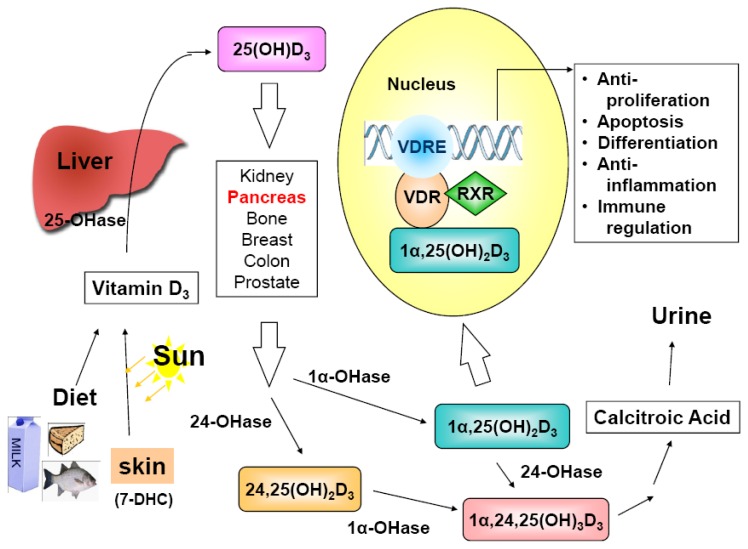
Figure 1.
Vitamin D sources, metabolism, mechanism of action and biological activities. Vitamin D3 (cholecalciferol) is either derived from the diet, including supplements, or synthesized in the skin via sunlight exposure (290-315 nm) from the precursor 7-dehydrocholesterol (7-DHC). Vitamin D3 is initially hydroxylated in the liver by vitamin D-25-hydroxylase (25-OHase) to generate the circulating prohormone 25-hydroxyvitamin D3 [25(OH)D3]. The subsequent conversion of 25(OH)D3 to the active form, 1α,25-dihydroxyvitamin D3 [1α,25(OH)2D3], occurs in the kidneys catalyzed by a tightly regulated enzyme 25(OH)D-1α-hydroxylase (1α-OHase or CYP27B1). However, the activation may take place in many extra-renal tissues, including pancreas, bone, breast, colon, prostate, etc. The extra-renal synthesis of 1α,25(OH)2D may be one reason why serum 25(OH)D level, instead of the circulating level of the active form, 1α,25(OH)2D, is the index of vitamin D nutritional status. The resulting 1α,25(OH)2D3 elicits its transcriptional effects by binding to the vitamin D receptor (VDR)/retinoid X receptor (RXR) complex on vitamin D response element (VDRE) in the promoter region of vitamin D responsive genes. The cellular effects include anti-proliferation, pro-differentiation, pro-apoptosis, anti-inflammation, immune response regulation, etc. In addition to 25-OHase and 1α-OHase, 24-OHase (CYP24A1) also plays an important role in the vitamin D metabolic cascade, and thereby, in the regulation of vitamin D actions. The primary role of 24-OHase is to hydroxylate 1α,25(OH)2D3 and 25(OH)D3 to their corresponding 24-hydroxylated metabolites, the first step of vitamin D catabolic pathway to inactivate VDR ligands.