Abstract
Background:
In both developing and developed countries, chronic pain remains a real issue and a true disease that affects up to 42% of the population in some areas. Opioids are widely used for the management of chronic pain with variations in prescribing practices, indications and observed efficacy.
Aim:
to analyze trends in opioids prescribing and patient response in chronic non-cancer pain conditions.
Methods:
Retrospective study of 1500 casenotes of patients suffering variable non-cancer chronic pain conditions. Detailed review of those cases who were managed using opioids. Statistical analysis using “SOFA” software set.
Results:
The prevalence of opioids prescribing in patients suffering this condition was thus around 35% (n=526). Women older than 50 years were more likely than men to have a chronic pain condition and to be given opioid therapy for 1 year or more. Opioid efficacy on neuropathic and mixed types of pain was found to be significant with relatively low rate of drop-out and limited side-effects that are not life threatening. Overall, patients stopped or changed their opioid medication due to inefficacy in only 12.7% of cases.
Conclusions:
The simple fact of having pain is itself a source of self-reported disability regardless of the actual physiological or pathological mechanism. Policy makers should be aware of the huge impact of chronic pain disease and of its serious effects on social and economical well-being. In developing countries, chronic pain could represent a real challenge for all parties. Multimodal management, including opioids, appears crucial for the approach of this disease.
Keywords: Age, chronic pain, gender, neuropathic, opioids
INTRODUCTION
Chronic non-cancer pain is a very common condition. Different etiological processes could lead to chronic pain, but the burden and effects on patient's life remain significant. The purpose of our present study is to understand the trends and variable characteristics of patients treated with opioids due to a chronic pain condition. Those include demographic, social, general health condition, type of the pain being treated and chronological data on the pain and the care being offered for these patients.
SETTING
The data were collated at the Pain Management Service (PMS) of a tertiary referral center in the UK. All patients were under the care of one Physician Consultant in Chronic Pain.
METHODS
A retrospective study. Each patient's casenote was reviewed to determine patients who were managed using opioids in which case further and more detailed review was performed. General demographic data, clinical data and phrmacological data were entered on a hard copy that guaranteed anonymous data collection- in line with local and national policy. Data were then fed into an electronic database and subsequently analyzed using the “SOFA” software package for statistical analysis.
RESULTS
A total number of 1500 case notes of patients who were seen at the PMS clinic between 1990 and 2006 were reviewed. Over one-third of patients (35%; n=526) were found to be treated using at least one opioid product. Further data collection was then performed on this group of patients allowing to provide the following information.
Demographic data
The majority of this group of patients were female (63%; n=332), and sex ratio f:m was 1.7:1. Patients overall average age was 57.67 years (range: 18 to 96) years. Female patients’ average age was significantly higher at 59.1 (range: 22-96 years) than males’ average age at 55.2 (range: 18-87 years) (ANOVA P=0.008 and F=7.11). This trend is also confirmed when above 50 year old are considered (P=0.043, F=4.146 an O’Brien P=0.01). Data was available about patients ethnicity in 242 patients of whom w white Caucasians represented 97.5% (n=236), the rest were Asians or Black patients (2.5%, n=6 patients).
Type of pain
Pain was described as Nociceptive type (Nc) in 54.3% of cases, Mixed nature (Mix) in 33.2%, and of Neuropathic type (Np) in 12.5% (n=286; 175; 65 patients, consecutively). In male patients, pain was Nc in 49%; Mix in 37%, and Np in 14% of cases (n=95; 71; 28 consecutively) [Table 1]. Females presented with Nc pain in 57%, Mix pain in 32% and Np pain in 11% (n=191; 104; 37 patients, consecutively). The T test shows no significant statistical difference between males and females in the probability to present with any one type of pain (P=0.39; t=0.945; df=4). In addition, as a whole, neither age (<50 vs >=50 year old) nor gender (male vs female) seems to affect the incidence of a specific type of pain [Tables 2 and 3] (t=1.0437; df=4; P=0.3555 for males and 1.2964; 4; 0.2645 for females), [Tables 1-3].
Table 1.
Type of pain and gender distribution
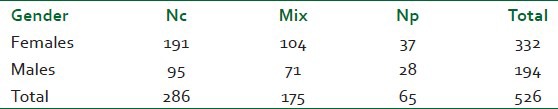
Table 2.
Type of pain and age, females

Table 3.
Type of pain and age, males

Duration of pain until referral to specialized care PMS
This duration was classified into 5 categories: Less than 6 months (a), 6 to 12 months (b), 1 to 5 years (c), 6 to 10 years (d) and more than 10 years (e). The great majority, 43% of patients, had no specialized input for a period up to 5 years (group ‘c’, n=227) followed by group ‘e’ (26%, n=135) and group ‘d’ (14.4%, n=76) [Table 4].
Table 4.
Duration of pain prior to first PMS visit
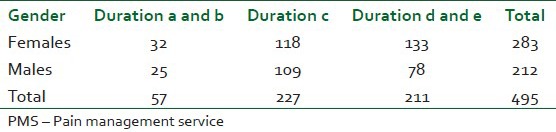
No statistical difference could be confirmed between males and females in regard to the duration of symptoms prior to referral to PMS within 5 years or more than 5 years (T test, t=1.4789, df=2 and P=0.2772).
Physical disability
Over a third of patients (35%; n=183) had some sort of physical disability limiting their professional and daily-life activities. Of these patients, 45% had a Nc pain, 42% had a Mix type pain, and 13% had Np pain (n=83; 76; 25 patients, consecutively). The type of pain did not have statistically significant effect on the prevalence physical disability (Chi sq.= 4.347; P=0.114; df=2), while there was a strong relation between the length of opioid therapy and the presence of physical disability (P=0.011; Pearson's Chi-Square statistic=11.064; df: 3). Physically limited patients were likely to have been treated with opioids for over 12 month periods.
Length of opioid therapy
Patients were included into four groups: ‘A’ if treatment by opioids lasted up to 3 months, ‘B’ if 3 to 6 months, ‘C’ if 6 to 12 months and ‘D’ if more than 1 year. The table below [Table 5] shows the relative numbers of these groups (excluding 40 cases of missing data).
Table 5.
Length of opioid therapy per gender
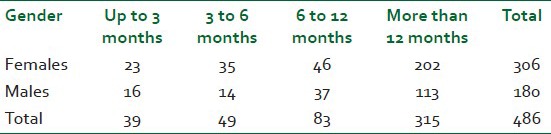
Female and male patients did not significantly differ as to the length of opioid therapy (χ2=3.979, df=3, P=0.264). However, the length of opioid therapy was significantly associated with the type of pain mechanism, with 87% of patients suffering Np or Mix symptoms staying on opioids for over 6 months versus 78% in the Nc group (χ2=16.547, df=6, P=0.011).
Age and the type of pain
In the group of above 50 year old, patients were significantly older in the Nc group when compared to the Np group (67 vs 63 year, T test: t=2.084, df=239, P=0,038). However, the average age did not differ in those younger than 50 year old for all types of pain (Nc, Np or Mix (P=0.758 and 0.58, consecutively).
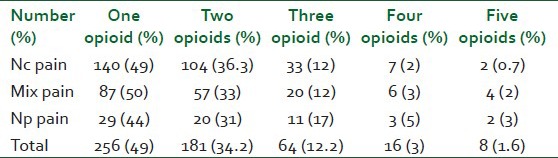
Opioids prescription
Number of compounds
Patients were prescribed up to 5 different products ranging from weak to strong opioids. Table 6 shows the number of compounds prescribed for patients, grouped by type of symptoms. The data does not necessarily reflect concomitant prescription but certainly “trials” of variable molecules in an effort to reach satisfactory pain control. No significant statistical difference was found between the different types of symptoms in respect to the number of opioids used/attempted in their treatment (T test, t=1.576, P=0.1536, df=8).
Table 6.
Number of opioids used per type of pain
Switching between and stopping compounds
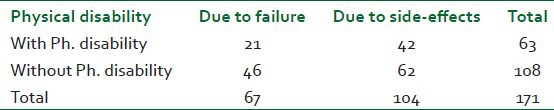
As it appears in Tables 7 and 8, overall, opioid therapy was stopped in 35.4% of cases (n=186). This was due to failure in 36% (n=67 equivalent to 12.7% of all patients). In the sample of those stopping/switching opioid compounds, side effects were a majority reason, in 56% (n=104; 19.7% of all patients.). When analyzed per pain type, failure reached 33% (n=31) in Nc, 36% (n=23) in Mix, and 48% (n=13) in Np patients. While the opioid was stopped due to SE in 59% (n=55 Nc), 58% (n=38 Mix) and in 41% (n=11 Np). The Np group seems to be more likely to suffer failure of opioid therapy (48%) when compared to other groups; however, no statistical significance was found (P=0.2629). Patients who had a physical disability had their opioids stopped/changed in 34.4% of cases (n=63, 21 cases due to failure and 42 due to side effects); this prevalence reached 31.5% in those without disability (n=108). Physical disability, per se, did not play a role in stopping or switching opioids (P=0.2304, t=1.7044).
Table 7.
Stopping/switching opioids
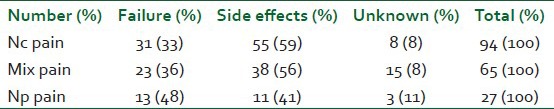
Table 8.
Stopping/switching opioids and disability
DISCUSSION
Prevalence and opioids use
Chronic pain affects a large number of patients worldwide. An estimated 37.3% of the population in developed countries and 41.1% in developing countries are thought to suffer of some form of chronic pain.[1] In Europe, an estimated 19% to 31.7% of the population is affected by chronic pain.[2,3] The social and economic consequences are not insignificant.[3,4,5] The calculated prevalence of chronic pain may depend on many factors among which are the types and mechanisms of the symptoms recorded, the geographical area, its economical level and its culture, the age and gender of patients. In our work above, we did not aim to study chronic pain prevalence within the general population, rather we studied various trends in chronic pain patients who were being managed with opioids. We therefore undertook the above study in an attempt to approach chronic pain issue from the opioid prescription angle and not the opposite. Case notes of 1500 patients at our university hospital Pain Management Service (PMS) were explored. Of those, we retained 526 case notes of patients who were on one or more opioid products for more detailed data collection and analysis. These patients accounted for 35% of chronic pain patients which is relatively high proportion of chronic pain population. Very similar prevalence was reported by Toth et al.[6] It is however important to note that the great majority of patients were on one opioid compound (n=256; 49%) followed by two compounds in 34.2% (n=181). Otherwise said, most patients did not require major changes in their therapeutic plans. In fact, a small percentage had received three compounds-at some point of their management – (12%) and even smaller group, 4.6% (n=24), received more than three. These figures lead us to believe that only a small group of patients were dropping out of their treatment suggesting that opioids played a major part in stabilizing their symptoms. Failure occurred only in 12.7% of all patients. Opioids seem to remain a good option even in those patients who were delayed from seeing a pain specialist. They also present as a relatively safe choice with no vital threat. The most common side-effects remain gastro-intestinal that are relatively easy to treat. Side-effects occurred in 19.7% cases and none was reported as life-threatening. However, and given the variable issues that encompass their prescription for prolonged periods, opioids remain a hot topic in chronic pain practice. The way opioids are prescribed is variable from one health system to another. The legal issues, fear of dependence, abuse, potential side effects, and general population misconceptions always played a role in shaping opioid therapy.[7,8]
Within this sample, the great majority of patients had nociceptive type of pain (Nc), were mostly females and aged more than 50 years. And as could be seen from the above results, patient's age followed a normal distribution spreading from young adults through to those aged more than 90 years. Indeed, chronic pain can be considered as very serious and common entity regardless of the initial triggering mechanism. Predominance of female patients, in general and in those older than 50 years, (P=0.008 and 0.043) is an important observation that was reported before our work in variable publications. This age and gender characteristic applied to chronic pain as a whole and to specific types such as neuropathic.[9,10,11] In addition, our results confirm that women were not only more likely than men to suffer a chronic pain condition, but also to be prescribed more opioids. This is in line with the work published by Damall et al. based on pharmacy claims data in the USA and finding that women were likely to be prescribed opioids more than men.[10] The great majority of our patients (63%) were indeed females. But when looked at the type of symptoms (Nc, Np, or Mix), there was no statistical evidence that the prevalence of females differed from males regardless of being older or younger than 50 years. Our work cannot thus confirm findings of the aforementioned authors that disparity between the two sexes tend to widen with progressing age.[10] Another gender disparity was reported by Campell et al. who identified higher prevalence and longer term of opioids use in women than in men.[11] Our data differed from that of the authors in finding similar time length of opioid therapy in both genders. The main factor that affected the length of opioid therapy was the type of pain (Nc, Np, or Mix) and not the patient's gender (P=0.011). In addition, 87% of patients who suffered a Mix or Np type of pain stayed on opioids for over 12 months. The requirement for opioids seems to last longer in case of Np pain. Opioid therapy, in this context, has common but not life-threatening side effects and the evidence is that it is effective in the management of Np pain.[12]
Patients were significantly older in the nociceptive group when compared to other types (neuropathic and Mixed; P=0.038). This finding is interesting and would support the concept of neuro-physiological changes due to aging. Age is associated with modification of the nociception processing mechanisms that leads to an increased pain threshold, a decreased pain tolerance and slower recovery of post-injury hyperalgesia phenomena.[13] Older patients could have a reduced functioning of striatal pain modulatory mechanisms with advancing age in contrast with an actual brain tissue atrophy that also affects these supra-spinal areas.[14] This may support the fact that post-injury chronic pain, for example, would be of higher prevalence in the older than 50 years for any type of pain although, in our study, we could support this theory only for the nociceptive type of chronic pain.
Patients of white origins represented over 97% of a sub-sample of our study (see above) which points out the disparity of access to specialized services of these patients and perhaps the type of management that being applied. Such disparity was also reported by the work of Green et al.[15]
Trend and burden of the chronic pain disease
A considerable number of patients were not seen by a specialized pain physician for up to 5 years duration of symptoms in 43% of cases. Furthermore, in 48% of cases, patients were delayed for over 5 years. But there was no statistical difference between females and males as in regard to the duration of chronic pain before first specialized input was sought. Such delays, we believe, could be due to reluctance of some patients to see the “chronic pain” service in the first place as this would mean “no curative management was available”. This delay could also be explained by the prolonged waiting lists in some cases or by lack of communications between GPs and Pain Services. It is very difficult to assert the actual reasons for such a trend.
Patients with chronic pain suffer variable degrees of disability. This could be in the form of full or partial dependence, partial or complete loss of job. Among our patients treated with opioids, a significant number (35%, n=183) had reported some degree of disability that hindered their normal daily life activities. This physical disability was not significantly associated with a particular type of pain nature. It appears as if the simple fact of having pain being itself a source of self-reported disability regardless of the actual physiological or pathological mechanism. Deterioration of patients quality of life is thought to be similar to that of those suffering arthritis, asthma, diabetes mellitus or depression.[16] This, in our view, justifies an additional emphasis on the management of the symptom pain with the same attention and effort of that of a potential curable or incurable long-term diseases. The economical burden is considerable for modern societies and starting early with adolescents to continue throughout life with an estimated 3840 million pounds (6064 million USD) annual cost for chronic pain in adolescent patients as was suggested in 2005.[17] Back pain alone could cost up to one fifth of health system budget and up to 1.5% of developed countries annual gross domestic product.[16]
CONCLUSIONS
Chronic pain is a major issue for public health. Its relatively high incidence and prevalence in developing and developed countries alike is consistent with a heavy impact on world's economy. For the chronic pain patient, the impact on social and personal life is major. Physical disability and depression are fertile ground for social and health instability.
While their prescription must remain “controlled”, opioids – weak and strong – must be made available for the management of chronic pain patients under specialized consultant practitioners in chronic pain. Opioids are very valuable in the management of chronic pain regardless of its type (Nc, Mix, or Np). Neuropathic pain (Np) is not an exception although opioids requirements could be more complex to predict and manage.
Older than 50 years female patients are more likely to suffer a chronic pain condition that could theoretically require opioid therapy. But there is no strong evidence that a widening gap is increasing with older age between the two sexes. In some studies, women older than 50 years are also found more prone to suffer a chronic neuropathic type of pain although our data do not support such conclusion. Nevertheless, patient's average age is likely to be older for the nociceptive pain group.
Chronic pain services are not always timely accessible for patients even in developed countries. Much effort must be invested in public information, physicians education, and training to reach a comprehensive and informed medical management of chronic pain.
ACKNOWLEDGMENT
Dr. N. Swaroop for aiding in the collection of data.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Tsang A, Von Korff M, Lee S, Alonso J, Karam E, Angermeyer MC, et al. Common chronic pain conditions in developed and developing countries: Gender and age differences and comorbidity with depression-anxiety disorders. J Pain. 2008;9:883–91. doi: 10.1016/j.jpain.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 2.Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: Prevalence, impact on daily life, and treatment. Eur J Pain. 2006;10:287. doi: 10.1016/j.ejpain.2005.06.009. [DOI] [PubMed] [Google Scholar]
- 3.Bouhassira D, Lantéri-Minet M, Attal N, Laurent B, Touboul C. Prevalence of chronic pain with neuropathic characteristics in the general population. Pain. 2008;136:380–7. doi: 10.1016/j.pain.2007.08.013. [DOI] [PubMed] [Google Scholar]
- 4.Gustavsson A, Bjorkman J, Ljungcrantz C, Rhodin A, Rivano-Fischer M, Sjolund KF. Socio-economic burden of patients with a diagnosis related to chronic pain – Register data of 840,000 Swedish patients. Eur J Pain. 2012;16:289–99. doi: 10.1016/j.ejpain.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 5.Raftery MN, Ryan P, Normand C, Murphy AW, de la Harpe D, McGuire BE. The Economic Cost of Chronic Noncancer Pain in Ireland: Results From the PRIME Study, Part 2. J Pain. 2012;13:139–45. doi: 10.1016/j.jpain.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 6.Toth C, Lander J, Wiebe S. The prevalence and impact of chronic pain with neuropathic pain symptoms in the general population. Pain Med. 2009;10:918–29. doi: 10.1111/j.1526-4637.2009.00655.x. [DOI] [PubMed] [Google Scholar]
- 7.Jamison RN, Ross EL, Michna E, Chen LQ, Holcomb C, Wasan AD. Substance Misuse Treatment for High Risk Chronic Pain Patients on Opioid Therapy: A Randomized Trial. Pain. 2010;150:390–400. doi: 10.1016/j.pain.2010.02.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Manchikanti L, Manchikanti KN, Pampati V, Cash KA. Observational study prevalence of side effects of prolonged low or moderate dose opioid therapy with concomitant benzodiazepine and/or antidepressant therapy in chronic non-cancer pain. Pain Physician. 2009;12:259–67. [PubMed] [Google Scholar]
- 9.Dieleman JP, Kerklaan J, Huygen FJ, Bouma PA, Sturkenboom MC. Incidence rates and treatment of neuropathic pain conditions in the general population. Pain. 2008;137:681–8. doi: 10.1016/j.pain.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 10.Darnall BD, Stacey BR. Sex differences in long-term opioid use cautionary notes for prescribing in Women. Arch Intern Med. 2012;172:431–2. doi: 10.1001/archinternmed.2011.1741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Campbell CI, Weisner C, Leresche L, Ray GT, Saunders K, Sullivan MD, et al. Age and gender trends in long-term opioid analgesic use for noncancer pain. Am J Public Health. 2010;10012:2541–7. doi: 10.2105/AJPH.2009.180646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eisenberg E, McNicol ED, Carr DB. Efficacy and safety of opioid agonists in the treatment of neuropathic pain of nonmalignant origin. JAMA. 2005;293:3043–52. doi: 10.1001/jama.293.24.3043. [DOI] [PubMed] [Google Scholar]
- 13.Gibson SJ, Farrell M. A review of age differences in the neurophysiology of nociception and the perceptual experience of pain. Clin J Pain. 2004;20:227–39. doi: 10.1097/00002508-200407000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Cole LJ, Farrell MJ, Gibson SJ, Egan GF. Age-related differences in pain sensitivity and regional brain activity evoked by noxious pressure. Neurobiol Aging. 2010;31:494–503. doi: 10.1016/j.neurobiolaging.2008.04.012. [DOI] [PubMed] [Google Scholar]
- 15.Green CR, Anderson KO, Baker TA, Campbell LC, Decker S, Fillingim RB, et al. The unequal Burden of pain, confronting racial and ethnic disparities in pain. Pain Med. 2003;4:277–94. doi: 10.1046/j.1526-4637.2003.03034.x. [DOI] [PubMed] [Google Scholar]
- 16.Phillips CJ. Economic burden of chronic pain. Expert Rev Pharmacoecon Outcomes Res. 2006;6:591–601. doi: 10.1586/14737167.6.5.591. [DOI] [PubMed] [Google Scholar]
- 17.Sleed M, Eccleston C, Beecham J, Knapp M, Jordan A. The economic impact of chronic pain in adolescence: Methodological considerations and a preliminary costs-of-illness study. Pain. 2005;119:183–90. doi: 10.1016/j.pain.2005.09.028. [DOI] [PubMed] [Google Scholar]


