Abstract
Adults with acquired language impairments secondary to stroke, traumatic brain injury, and neurodegenerative diseases are candidates for communication supports outside of the traditional restoration-based approaches to intervention. Recent research proves repeatedly that augmentative and alternative communication (AAC) provides a means for participation, engagement, conversation, and message transfer when individuals can no longer expect full return of pre-morbid communication skills and that inclusion of communication supports should begin early. We discuss current research and future directions for integrated systems of technical supports that include low-technology, high tech, and partner-dependent strategies for adults with severe and chronic aphasia, cognitive-communication problems resulting from traumatic brain injuries, and primary progressive aphasia.
Keywords: acquired disabilities, aphasia, augmentative and alternative communication (AAC), cognition, dementia, primary progressive aphasia, traumatic brain injury
A recent emphasis has emerged on the social participation approach to intervention for adults with acquired communication impairments, with meaningful life outcomes being a desired result (Simmons-Mackie, 2001). Participation in conversation and daily functional tasks is an agreed-upon goal for which many families, clinicians, and patients strive (LPAA Project Group, 2001). Regardless of whether adults have experienced stroke, traumatic brain injury, or neurodegenerative disease, they still carry expectations of communication competence as they enter a conversational interchange. Fox and Sohlberg (2000) remind us that individuals with severe acquired communication disorders must make choices every day regarding when, how, and with whom to engage in social interactions. They must expend considerable energy to communicate, since they are experiencing new social and environmental demands with every encounter. They have new social roles as family members, peers, employees, and employers that must be addressed by all members of communication interactions. Often, their social networks for communication are significantly reduced as a result of the communication impairment. They must learn to use new or familiar communication tools in different ways and accept different outcomes from daily exchanges.
As augmentative and alternative communication (AAC) researchers, our role is to understand the different tools that comprise the communication continuum and develop a knowledge base that strives to design the best strategies, techniques, and equipment to maximize performance and success in communication exchanges. This challenge becomes even greater when we consider the present health care delivery system for the AAC decision-making process (Yorkston & Beukelman, 2000). We must base our recommendations on knowledge about staging interventions using a small evidence base. We must integrate evidence from aphasiology, neuroscience, and rehabilitation technology as we enhance the research agenda within the field of AAC and cognitive-communication disorders for adults. We must frame assessment and intervention in a participation model that encompasses meaningful outcomes for individuals and families that are common to both AAC and general rehabilitation.
Currently, the AAC researcher addresses compensatory strategies and tools for adults with cognitive-communication impairments in an attempt to maximize communication function for social interaction. For example, a woman with an expressive naming problem might use a speech generating device with visual scenes to point to people in her daughter’s wedding party instead of struggling to rely on natural language to retrieve names. Another approach to communication treatment relies on restorative techniques. Within traditional aphasiology, researchers in acquired communication disorders for adults have examined ways to restore speech and language, trying to help the individual recover skills that were impaired due to brain damage. Intervention studies examine different techniques that can stimulate language recovery. For example, increasing rehearsal on high-frequency, personally relevant words might be recommended for naming treatment. Or, training individuals to think of semantic features of target nouns (i.e., location, use, item category, location, use, action) might improve naming abilities. Often, little overlap occurs between the research conducted using the AAC compensatory strategy approach and a restorative treatment paradigm. As we look for commonalities between the restorative community and the AAC compensatory support community, we should consider the World Health Organization’s International Classification of Functioning, Disability and Health (ICF) (World Health Organization, 2001). The ICF provides a framework that bridges rehabilitation technology, aphasiology, and AAC intervention. Within assistive technology, DeRuyter (1995) discussed using the ICF to assess outcomes; within aphasiology, the Living with Aphasia: Framework for Outcome Measurement (A-FROM) has been proposed as an instrument to measure meaningful outcomes (Kagan et al., 2008; Simmons-Mackie & Kagan, 2007), and within AAC, the ICF is being adapted as a theoretical and practical organization scheme for communication measurement (Raghavendra, Bornman, Granlund, & Bjorck-Akesson, 2007; Rowland et al., 2012). We should acknowledge that the ICF is a worldwide document that has been accepted as a way to examine the impact of complex communication needs on participation and environment.
We will discuss current and future research agendas for AAC, addressing three populations of adults with acquired disabilities: chronic, severe aphasia; traumatic brain injury; and primary progressive aphasia. Issues relating to participation within the natural environment will be raised, as well as the integration of communication supports within a restorative treatment paradigm for cognitive, language, and motor impairments and the emergence of future technologies for communication supports.
CHRONIC, SEVERE APHASIA AND AAC
Aphasia is an acquired communication disorder in which a person struggles to process language symbols despite having normal intellectual functioning (National Aphasia Association, 2009; McNeil & Pratt, 2001). People with aphasia routinely have difficulty retrieving words, combining words into phrases and sentences, and understanding the verbalizations of others; most experience concomitant and comparable challenges with reading and writing.
More than 100,000 people in the United States acquire aphasia each year, with stroke (i.e., cerebrovas-cular accident or CVA being the most common cause (National Aphasia Association, 2009). Many people with sudden-onset aphasia retain or regain sufficient skills to manage a majority of their communication needs through natural speech. However, a substantial portion of adults with sudden-onset aphasia experience persistent and complex communication challenges that either remain unmet or require support using compensatory strategies or alternatives to natural speech (LaPointe, 2005; Laska, Hellblom, Murray, Kahan, & Von Arbin, 2001).
Current AAC Acceptance and Use by People with Sudden-onset Aphasia
The use of AAC support strategies by people with unmet communication needs due to aphasia has progressed slowly through the years. Several factors have contributed to the relatively limited development, implementation, acceptance, and use of compensatory communication supports with this population. First, the primary focus of most intervention procedures has been on the restoration of natural speech production and comprehension, simply because people with aphasia and their families desire a return to functioning comparable to that experienced prior to stroke. Second, intervention funding encourages restoration-based services in that, when people plateau in recovering natural speech functions, funding—and therefore intervention services—often terminates. Third, the tendency to focus on natural speech restoration has meant that clinicians often omit attention to communication supports while delivering intervention. People with aphasia and their families often must seek out AAC services on their own. Unfortunately, many personnel who provide intervention in restoration-focused rehabilitation programs state that they “do not do AAC” when individuals and family members request such services. Fourth, AAC specialists have been slow to develop strategies to address the needs of people with limited language capabilities despite essentially intact intelligence, world knowledge, and life experiences. Only during the past decade have AAC professionals systematically focused on developing and implementing communication supports for people with severe, chronic aphasia.
The use of low-technology strategies to supplement the residual speech of people with aphasia currently exceeds the use of high-technology strategies. Despite the many factors limiting the development and acceptance of AAC supports for people with severe, chronic aphasia, low-technology interventions focused on using multimodal supports, topic setters, and written choice conversation as well as interventions designed to improve writing, drawing, pointing, and referencing photographic images and line-drawings have increased in recent years (Fox, Sohlberg, & Fried-Oken, 2001; Garrett & Beukelman, 1995; Garrett & Lasker, 2005; Ho, Weiss, Garrett, & Lloyd, 2005; Lasker, Garrett, & Fox, 2007; Lasker, Hux, Garrett, Moncrief, & Eischeid, 1997; Lyon, 1995a, 1995b). All of these intervention techniques are similar regarding their simplicity and minimal demands for specialized materials. For example, topic setters can take the form of tangible remnants or souvenirs (e.g., ticket stubs, sporting event programs, menus, photographs, maps, etc.) or single communication book pages that incorporate pictures and/or key phrases relating to a specific event (Beukelman, Yorkston, & Dowden, 1985; Garrett & Huth, 2002; Ho et al., 2005); written choice conversations require a communication partner to write down key words relating to an established topic and from which a person with aphasia can select his/her desired response (Garrett & Beukelman, 1995; Lasker et al., 1997); multimodal supports incorporate numerous techniques simultaneously or in sequence to resolve communication breakdowns as they occur (Hux, Weissling, & Wallace, 2008). The selection and implementation of these types of low-technology supports vary substantially across individuals depending on the extent of their residual language and cognitive capabilities.
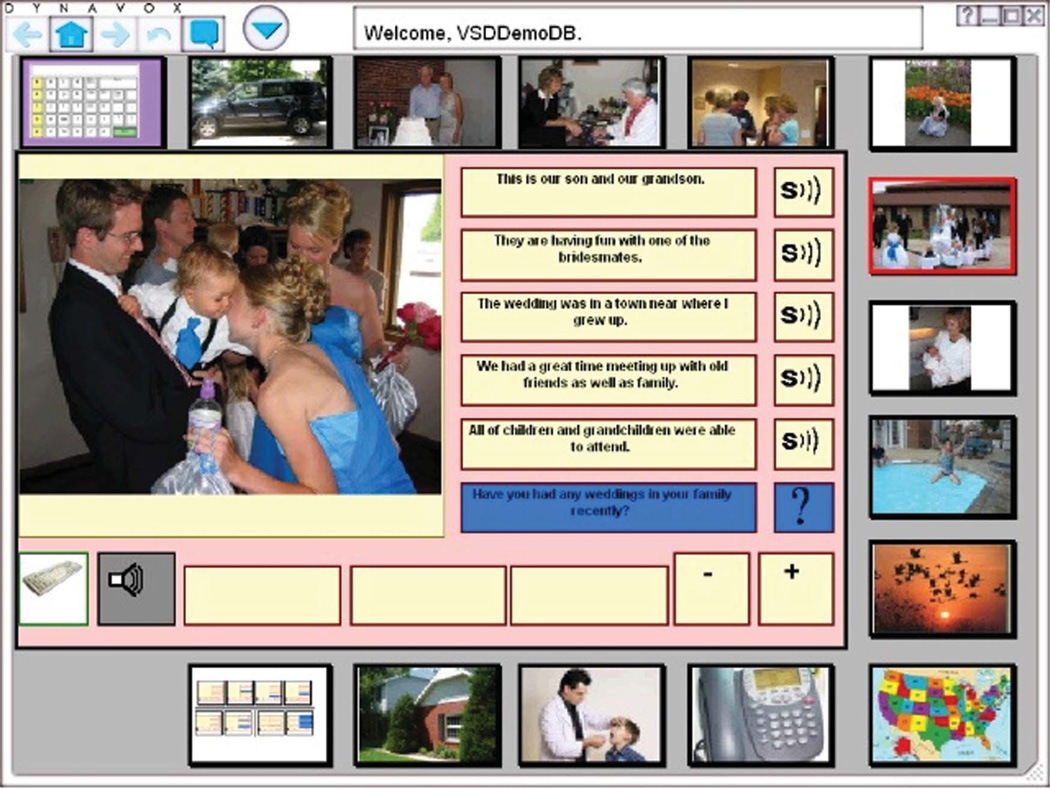
High-technology interventions have traditionally been relatively rare in clinical practice, but on-going research and technological developments make the implementation of such supports increasingly feasible. Initially, people with aphasia used AAC devices only to meet specific communication needs such as answering the phone, delivering prepared speeches, or ordering in restaurants. AAC devices for people with aphasia typically contained a limited number of messages or message types and were intended for use only in situations in which speech output was essential. With advances in technology, however, a wider range of options is now available for people with aphasia. In particular, recent technological developments supporting the use of personally-relevant and contextually-rich digital images to convey content on dynamic screens available via AAC equipment, tablet computers, and mobile devices have emerged. Figure 1 provides an example of what a high-technology AAC screen using personally-relevant, contextually-rich images accompanied by written phrases might look like. These technological developments open the possibility for AAC to provide supports to people with aphasia in a variety of communication environments and situations and across a range of interaction partners.
FIGURE 1.
Visual scene for aphasia (color figure available online).
Review of Research Related to Communication Supports
Several researchers have documented the use of low- and high-technology communication supports by individual people with sudden-onset aphasia (Fried-Oken, 1995; Garrett & Beukelman, 1995; Garrett, Beukelman, & Low-Morrow, 1989; Garrett & Huth, 2002; King & Hux, 1995; Lasker, LaPointe, & Kodras, 2005). Typically, these case reports and single case studies have documented the frequency and effectiveness with which individuals have used AAC systems designed specifically to meet their unique communication needs. Many of these studies also report the preferences and satisfaction of people with aphasia regarding their AAC systems. In some case studies, researchers have reported about comprehensive communication supports that include several components and are of assistance to a person with aphasia in multiple communication settings and across a range of communication partners. For example, Garrett, Beukelman, and Low-Morrow (1989) described a multimodal, low-technology system incorporating natural speech, gestures, writing, drawing, a first-letter spelling alphabet card, a thematic word dictionary, a suggestion list for resolving breakdowns, and a list of conversational control phrases. For other cases, researchers have described systems targeting specific communication needs or situations. For example, Lasker, LaPointe, and Kodras (2005) developed and evaluated a system designed specifically to assist a university professor in delivering class lectures; King and Hux (1995) taught an adult with aphasia to use talking word processing software to edit his written work.
Additional research exists regarding specific characteristics of AAC support materials and the effect of these characteristics on the communicative performance of people with aphasia. For example, McKelvey, Hux, Dietz, and Beukelman (2010) studied the effect of personal relevance and image contextualization on the preferences and word-picture matching accuracy of people with severe aphasia. By pairing visual stimuli with three types of target words—labels of people or objects, actions, and socially relevant events— researchers found that participants preferred personally relevant, contextualized photographs over non-contextualized iconic drawings or non-personally relevant, contextualized photographs. Participants performed more accurately when matching spoken words to pictures given personally relevant, contextualized photographs rather than non-contextualized iconic drawings or non-personally relevant, contextualized photographs.
Hux, Buechter, Wallace, and Weissling (2010) examined how the creation of a shared communication space using a low-technology AAC support system affected the content and quality of interactions between a person with aphasia and unfamiliar communication partners. The AAC system combined contextually-rich photographs and written messages to create visual scene displays about a topic of interest to the person with aphasia. Participants engaged in conversations about the selected topic in one of three conditions: (a) a shared condition in which both the person with aphasia and his communication partner had access to the AAC system, (b) a non-shared condition in which only the person with aphasia had access to the AAC system, and (c) a no-AAC condition in which neither participant had access to the system. Comparisons across conditions revealed the shared condition prompted the greatest number of conversational turns, the highest level of conceptual complexity in the utterances generated by communication partners, the greatest number of content units generated by the person with aphasia, and the best perception by the person with aphasia regarding information transfer, ease of conversational interaction, and partner understanding. The authors concluded that using visual scene displays as an AAC support to create a shared communication space positively affected the manner and extent to which both a person with aphasia and communication partners contributed to conversational interactions involving information transfer.
Dietz, McKelvey, Hux, and Beukelman (2009) examined the effect of various visuographic supports on the reading comprehension of people with chronic, nonfluent aphasia. Participants silently read ten-sentence passages accompanied either by high-context photographs, low-context photographs, or no photographs and then responded to multiple choice comprehension questions presented using the written choice conversation strategy. Across participants, response accuracy was significantly better given the high-context photograph condition. In addition, the participants consistently indicated through Likert ratings that they perceived the high-context photographs as being helpful to their reading comprehension; they were less consistent in this perception given the low-context photographs.
Future Directions
A need exists for additional research and development in many areas related to the population of people with sudden-onset aphasia. A major challenge facing clinicians is the integration of communication supports into all aspects of aphasia intervention rather than the continued segregation of restoration and compensatory interventions, as has traditionally occurred. In each recovery setting, whether acute medical, inpatient rehabilitation, outpatient rehabilitation, or long-term care, people with sudden-onset aphasia need to participate effectively in decision-making activities while also working to reduce their communication impairments. In accordance, our role is to provide research evidence to professionals that will enable them to introduce novel intervention strategies, materials, and AAC technologies in an effective manner while simultaneously performing on-going evaluations of the communicative competence of people with aphasia with respect both to language restoration and compensation.
The development and evaluation of new technologies supporting communication for people with severe, chronic aphasia are important future priorities. The ongoing release of innovative mobile technologies that are lightweight and that provide dynamic screen capability, speech output, web (cloud) access, and built-in cameras to allow immediate capture of personally-relevant images is particularly important for this population. Given their world knowledge, extensive personal experience, and preserved visuospatial and intellectual functioning, research and development about ways people with aphasia can meet their communication needs by storing and accessing information via maps, photographs, and videos is a priority. In addition, many people with severe aphasia collaborate with communication partners to co-construct meaning during communication exchanges and establish mutually-shared communication spaces. As of yet, the AAC field has spent little time developing and implementing high-technology strategies to support such message co-construction.
Another area of needed research relates to ways in which people with aphasia manage various types of AAC designs. Differences in layouts and organizational frameworks underlying AAC devices can have a substantial effect on system transparency and, hence, the ease with which people with aphasia can gain technological and navigational competence. Researchers have yet to investigate the interplay among cognitive and linguistic strengths and challenges displayed by individuals with aphasia and various intervention strategies aimed at teaching them to use AAC devices to support communication. In particular, further research is needed regarding the speed, accuracy, and overall efficiency with which people with aphasia learn to implement various AAC strategies and generalize those techniques to everyday situations involving a variety of communication settings and partners.
TRAUMATIC BRAIN INJURY AND AAC
Traumatic brain injury (TBI) refers to open and closed injuries to the head resulting in diffuse and/or focal neurological damage. The extent, severity, location, and type of damage vary extensively from person to person and depend on a complex interplay of multiple instantaneous and delayed injury mechanisms. The recent prevalence of military-related blast injuries has influenced the injury profile of the TBI population. Because of wide variations in sustained damage, people with TBI can experience a range of communication disabilities including motor speech disorders, aphasia, and/or cognitive-communication deficits (Fager, Doyle, & Karantounis, 2007). We will focus on communication disorders of sufficient severity to necessitate AAC supports.
Motor speech disorders associated with TBI often result from a combination of spasticity due to upper motor neuron damage and flaccidity due to lower motor neuron damage (Duffy, 2005). Typically, motor speech disorders of sufficient severity to require AAC supports stem from damage to the brainstem (Fager et al., 2007). This damage can be the direct result of an initial trauma or a secondary consequence to brain swelling that interrupts blood flow to the base of the brain and brainstem. Recent advances in medical treatments serving to limit brain swelling or the negative consequences associated with brain swelling may reduce the frequency and extent of motor speech disorders observed in this population; researchers have yet to confirm this hypothesis, however.
Aphasia can appear as a form of specific language impairment following TBI. Sometimes aphasia appears in isolation, but, more commonly, it appears in combination with cognitive-communication deficits or motor speech disorders (Hux, 2011). Further complicating the diagnosis of aphasia is the phenomenon that, during early recovery, many survivors struggle to answer questions and express basic ideas, and professionals may mistakenly label the disorder as aphasia. In actuality, these communication challenges are often transitory and reflect generalized confusion and impaired consciousness rather than traditional aphasia (Hux, 2011). Over time, survivors of TBI may display none of the linguistically-based impairments typical of people with aphasia. When this is the case, long-term AAC supports may be unnecessary; however, survivors of TBI who display traditional and chronic aphasia may find AAC supports beneficial.
Cognitive-communication deficits are the most common communication impairment to result from TBI. By definition, cognitive-communication deficits refer to decreased performance of language-based activities secondary to impairment in one or more aspects of cognition (e.g., attention, perception, memory, executive function, etc.) supporting communication (American Speech-Language-Hearing Association, 2005; Coelho, 2007). Almost without exception, these deficits interfere with the communication, social, educational, and vocational effectiveness of people with TBI. Many people who have cognitive-communication deficits without concomitant aphasia or motor speech disorders do not need AAC supports to express basic intents; however, they may rely extensively on assistive technologies to compensate for their cognitive challenges. Individuals who have cognitive-communication deficits in combination with aphasia or motor speech disorders of sufficient severity to warrant use of AAC face the challenge of having to master new communication strategies, techniques, and/or devices in the presence of cognitive limitations severely hampering learning.
AAC Acceptance and Use
Numerous case reports and single-case descriptions exist documenting the early use of AAC by people with TBI (e.g., Beukelman, Yorkston, & Dowden, 1985; DeRuyter & Donoghue, 1989; Light, Beesley, & Collier, 1988). In terms of documenting AAC intervention strategies effective with survivors displaying different types of communication challenges, Fager, Doyle, and Karantounis (2007) and Fager and Karantounis (2011) provide summaries across various stages of recovery. Additional researchers have documented AAC use by relatively large groups of survivors (DeRuyter & Lafontaine, 1987; Keenan & Barnhardt, 1993).
A recent study about AAC use following TBI reported on 25 adults with on-going communication support needs that spanned multiple years post-injury (Fager, Hux, Karantounis, & Beukelman, 2006). Eight study participants received low-technology AAC interventions only, and 17 received high-technology options or a combination of high- and low-technology options at various times post-injury. The initial acceptance rate of low-technology options was 100% among study participants. The initial acceptance rate of high-technology AAC devices was 94%, with only one individual rejecting this type of system. This rejection was because the individual wished to pursue natural speech only as a means of communicating despite the fact that familiar listeners judged his attempts to be ineffective. Two other individuals discontinued long-term use of high-technology AAC devices because of inadequate AAC support when they transferred from one living facility to another; one was unsuccessful in obtaining a device because of funding issues.
Review of Research Related to Communication Supports
Most people with TBI who rely on AAC formulate messages by spelling individual words (Doyle, Kennedy, Jausalaitis, & Phillips, 2000; Fager et al., 2006; Fried-Oken & Doyle, 1992). Exceptions to this primarily involve individuals who sustain injuries as children who have not yet learned to spell. A few survivors use word or message prediction strategies to speed the letter-by-letter spelling process, but cognitive deficits often interfere with use of this type of message-retrieval strategy (Burke, Wassink, Martin, & Seikel, 2008; Doyle et al., 2000; Fager et al., 2006; Fried-Oken & Doyle, 1992). No other reported studies document the message representation capabilities of people with TBI.
The accuracy and speed with which people with severe TBI can navigate dynamic screen AAC devices is an issue of concern regarding communicative efficiency. In an investigation of this subject, Wallace, Hux, and Beukelman (2010) found that participants who demonstrated sufficient cognitive flexibility to pass the Symbols Trails subtest of the Cognitive Linguistic Quick Test (Helm-Estabrooks, 2001) performed system navigation significantly more accurately than those who did not pass the subtest. Regarding another aspect of device use, Wallace and her colleagues found that all participants navigated more accurately when provided with contextually-rich images rather than isolated people, animals, or objects appearing on plain backgrounds.
Future Directions
Many people who experience both cognitive and communication limitations secondary to TBI could benefit from having an integrated system of technological supports for communication, memory, personal organization (schedules), reading, and recreation. Such systems are likely to become increasingly available as advances in technology continue, but little, if any, research exists documenting the effectiveness with which survivors can master integrated devices. Because of the extensive cognitive limitations manifested by people with TBI who cannot meet their communication needs solely through natural speech, an ongoing need exists to perform research and development activities that identify and evaluate strategies to reduce the cognitive load associated with mastering AAC devices.
People with TBI who rely on communication supports often need AAC facilitators to maintain their equipment, instruct new communication partners, and provide instruction as needed. Fager and her colleagues (2006) documented that some people with TBI discontinue use of high-technology AAC devices because of a lack of facilitator support. Research focusing on AAC facilitator instruction, especially through distance learning options, remains an important future goal.
Finally, many people with TBI have some residual speech, although it may not be adequate to meet daily communication demands. The development of speech recognition technology that can translate disordered speech into text is a possible means of compensating for such a problem. More information about research in this area appears in the speech recognition section of the Fager, Beukelman, Fried-Oken, Jakobs, and Baker article (2012) published in this issue.
PRIMARY PROGRESSIVE APHASIA AND AAC
Primary progressive aphasia (PPA) is a relatively new diagnosis that was first described by Mesulam (1982, 2001) based on linguistic and cognitive symptoms (Hodges & Patterson, 1996; Neary et al., 1998; Gorno-Tempini et al., 2004). Three variants of PPA are described: non-fluent, semantic, and logopenic PPA. Wilson and colleagues (2010) recently published the most comprehensive clinical research study on the language characteristics of these three subgroups. Individuals with nonfluent progressive aphasia (NFPA) are, by definition, non-fluent and present with an apraxia of speech that may become so severe that it results in mutism. Adults with NFPA demonstrate agrammatism, speech distortions, reduction in speech rate, paraphasias, and reduced fluency during connected speech. Individuals with the semantic variant of PPA are anomic, producing reduced speech rate because of problems with word finding rather than motor speech impairment. Preserved motor speech and syntax skills suggest that the semantic variant can be described by a disorder in lexical content. The final group with logopenic PPA presents with a non-fluency resulting from phonological rather than motor speech impairments during connected speech, with some syntax disturbance, word finding pauses, or rephrasings that appear to be more related to phonemic errors than to lexical or motor speech errors.
Adults with PPA are appearing more and more in AAC clinics. Language intervention for adults with progressive nonfluent aphasia has been reported during the past 15 years (Cress & King, 1999; Fried-Oken, 2008; Murray, 1998; Rogers & Alarcon, 1998; Rogers, King, & Alarcon, 2000). Rogers and Alarcon present a management scheme based on the clinical picture of NFPA that is representative of most intervention reports. It includes three stages: (1) anticipatory implementation of communication strategies, since communication independence declines as the disease progresses; (2) disability-based intervention focused on early utilization of AAC; and (3) dyad-oriented intervention. In the early stage, intervention is based on the need to convey specific information in specific situations, such as telling your spouse what to buy at the store. In this stage, strategies for pacing, syllable segregation, word retrieval, and identification of topic and key words are recommended. Mid-stage treatment recommendations include reliance on printed materials, idiosyncratic gestures, communication boards or cards, speech generating devices with language options, and partner/family training to provide multi-modal input to support comprehension for the person with PPA. Late stage treatment includes prompting, errorless training for pointing to referents, and teaching partners to provide basic choices for expression. These late stage strategies, although intuitively appropriate, are not yet supported by scientific evidence. As is evident, the goals for intervention change as the person with PPA moves from unassisted to assisted communication.
Clinical intervention for adults with PPA can be set within a communication supports framework with two primary goals: to provide patients with visual lexical supports so that they can participate in daily activities as their language skills decline and to engineer the environment to support successful communication. Operationally, these two challenges are expressed as three treatment objectives: (1) to compensate for progressive language loss (not to stimulate the language system to regain skills); (2) to start early so that the person with PPA can learn to use communication strategies and tools as soon as possible; and (3) to include communication partners in all aspects of training, with outreach to multiple partners. The neurodegenerative goals resemble treatment for individuals with motor neuron disease, while the content resembles goals used for aphasia intervention.
Future Directions
While evidence clearly demonstrates the value of low-technology AAC for individuals with PPA, little empirical data exist on the use of high-tech speech generating devices for this population. As with the severe, chronic aphasia population, new questions arise for this clinical group as the general population is presented with new technologies, new storage methods, and novel presentation strategies. Mobile computing and devices such as the tablet and smart phone must be examined for individuals who are familiar with communication competence and bring technological savvy to the task of interaction.
The field of AAC has staged interventions for individuals with neurodegenerative motor speech disorders, especially ALS (Trautman et al., 2002). Fried-Oken, Rowland, and Gibbons (2010) proposed PPA staged interventions that clearly combine a restorative rehabilitation approach with a communication support approach for this progressive disorder. Research efforts must be directed to the issues surrounding language learning and use that are required for communication supports during a degenerative disease. For example, additional knowledge is needed to understand if adults with mild PPA should learn to use personally relevant, contextualized photographs even though they can still spell and use a computer keyboard adequately. Issues about how to organize the visual language for adults with PPA during different stages of their disease should be addressed. For example, does one system work when individuals are still literate, and then does another, picture-based system maximize performance when they can no longer rely on orthography? Or, should they be competent users of picture-based language systems before they are needed? We still do not understand the range of cognitive skills that people with PPA bring to the task of learning to use communication supports, or how the progressive disorder affects cognitive strategies for language use. Additional questions persist about the complex multi-modal nature of communication systems. Often, individuals diagnosed with PPA are still multi-tasking, relying on smart phones, daily calendars, e-mail, and social networking software on laptops while writing text and interacting verbally. Research should examine multi-modal communication options for the person with PPA, considering their projectile for mutism and language loss. Intervention studies should be designed to address whether a predictable set of supports should fade away or be reinforced during the disease progression. Communication supports for people with PPA is now becoming evidence-based practice. Clearly, research in the future will address many issues as we learn more about the disease and the features of the three variants of PPA, as we expand the features of communication technology, and as we come to understand the role of communication supports within this progressive language degeneration process.
CONCLUSION
Common themes exist for research agendas across the three populations discussed. This is a time of change within rehabilitation technology. With the advent of mobile technology, the definition of communication and the means to socially interact are changing drastically (Shane, Blackstone, Vanderheiden, Williams, & DeRuyter, 2012). These changes will be felt strongly by the future group of adults with acquired neurological conditions who developed verbal communication, technology, and media use skills as typical speakers and writers. Future adults with chronic aphasia, traumatic brain injuries, and progressive aphasia may have used widely-available communication technologies for e-mailing, telephoning, and social networking in their previous employment, education, and recreation. We should expect a seamless transition from everyman’s technology to assistive technology for communication supports.
The future research agenda for AAC and adults with acquired cognitive-communication impairments must be based on the acquisition of knowledge to maximize performance and social interaction through the design of optimal communication supports and intervention paradigms within a technology-savvy world. We must reduce the cognitive load for learning communication devices while simultaneously developing the technology that supports cognitive-communication tasks. Within general technology today, machine learning of language is exploding, and we must incorporate that work within AAC technology (Higginbotham, Lesher, Moulton, & Roark, 2012). AAC technologies should learn the cognitive and language demands of each individual user and adapt or adjust over time as the adult with acquired neurological impairment learns his/her device. We must develop novel systems with new technologies that integrate residual use of speech, language, cognitive, and motor abilities with creative and novel ways to visually represent and store language for meaningful participation by users. We must place communication within an environment where message co-construction is optimized and knowledge of the physical world is automatic.
The value of using a functional framework to understand the integration of communication devices with restorative treatment strategies must be understood for adults, regardless of the neurological basis of their impairments. In addition to learning more about the communication and cognitive skills that adults bring to the task of AAC, we must examine best ways to represent language concepts, best ways to present language in low-tech and high-tech media, and best ways to integrate the strategies into the natural environments for conversation. In 2007, RERC partners addressed AAC and acquired neurological conditions (Beukelman, Fager, Ball, & Dietz, 2007). We have progressed significantly in our understanding of communication supports since their research challenge. We have entered a decade where a current technological explosion drives our proposed agenda, and the social values of engagement and participation are shaped by the integration of language restoration and compensation philosophies.
ACKNOWLEDGMENT
The preparation of this manuscript was supported in part by The Rehabilitation Engineering Research Center on Communication Enhancement (AAC-RERC) funded under grant #H133E080011 from the National Institute on Disability and Rehabilitation Research (NIDRR) in the U.S. Department of Education’s Office of Special Education and Rehabilitative Services (OSERS).
REFERENCES
- American Speech-Language-Hearing Association. Roles of Speech-Language Pathologists in the Identification, Diagnosis, and Treatment of Individuals with Cognitive-Communication Disorders: Position Statement [Position Statement] 2005 Available from www.asha.org/policy.
- Beukelman D, Yorkston K, Dowden P. Communication augmentation: A casebook of clinical management. San Diego, CA: College Hill Press; 1985. [Google Scholar]
- Beukelman DR, Fager S, Ball L, Dietz A. AAC for adults with acquired neurological conditions: A review. Augmentative and Alternative Communication. 2007;23:230–242. doi: 10.1080/07434610701553668. [DOI] [PubMed] [Google Scholar]
- Burke R, Wassink K, Martin T, Seikel A. Message retrieval for survivors of traumatic brain injury. Augmentative and Alternative Communication. 2008;23:56–63. doi: 10.1080/07434610701421015. [DOI] [PubMed] [Google Scholar]
- Coelho CA. Management of discourse deficits following traumatic brain injury: Progress, caveats, and needs. Seminars in Speech and Language. 2007;28:122–135. doi: 10.1055/s-2007-970570. [DOI] [PubMed] [Google Scholar]
- Cress C, King J. AAC Strategies for people with primary progressive aphasia without dementia. Augmentative and Alternative Communication. 1999;15:248–259. [Google Scholar]
- DeRuyter F, Donoghue K. Communication and traumatic brain injury: A case study. Augmentative and Alternative Communication. 1989;5:49–54. [Google Scholar]
- DeRuyter F. Evaluating outcomes in assistive technology: Do we understand the commitment? Assistive Technology. 1995;7(1):3–8. doi: 10.1080/10400435.1995.10132246. [DOI] [PubMed] [Google Scholar]
- DeRuyter F, Lafontaine L. The nonspeaking brain injured: A clinical demographic database report. Augmentative and Alternative Communication. 1987;3:18–25. [Google Scholar]
- Dietz A, McKelvey M, Hux K, Beukelman DR. Reading comprehension by people with chronic aphasia: A comparison of three levels of visuographic contextual support. Aphasiology. 2009;23:1053–1064. [Google Scholar]
- Doyle M, Kennedy M, Jausalaitis G, Phillips B. AAC and traumatic brain injury. In: Beukelman DR, Yorkston KM, Reichle J, editors. Augmentative and alternative communication for adults with acquire neurological disorders. Baltimore, MD: Brookes Publishing Co.; 2000. pp. 271–304. [Google Scholar]
- Duffy J. Motor speech disorders: Substrates, differential diagnosis, and management. St. Louis: Mosby; 2005. [Google Scholar]
- Fager S, Beukelman D, Fried-Oken M, Jakobs T, Baker J. Access interface strategies. Assistive Technology. 2012;24:25–33. doi: 10.1080/10400435.2011.648712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fager S, Doyle M, Karantouis R. Traumatic brain injury. In: Beukelman D, Garrett K, Yorkston K, editors. Augmentative communication strategies for adults with acute or chronic medical conditions. Baltimore, MD: Paul H. Brookes Publishing Co.; 2007. pp. 59–90. [Google Scholar]
- Fager S, Hux K, Karantounis R, Beukelman D. Augmentative and alternative communication use and acceptance by adults with traumatic brain injury. Augmentative and Alternative Communication. 2006;22:37–47. doi: 10.1080/07434610500243990. [DOI] [PubMed] [Google Scholar]
- Fager S, Karantounis R. AAC assessment and intervention. In: Hux K, editor. Assisting survivors of traumatic brain injury: The role of speech-language pathologists. 2nd ed. Austin, TX: Pro-ed; 2011. pp. 227–254. [Google Scholar]
- Fox L, Sohlberg MM. Meaningful Roles. In: Beukelman D, Yorkston KM, Reichle J, editors. Augmentative and Alternative Communication for Adults with Acquired Neurological Disorders. Baltimore, MD: Paul H. Brookes Publishing Co.; 2000. pp. 3–24. [Google Scholar]
- Fox L, Sohlberg MM, Fried-Oken M. Effects of conversational topic choice on outcomes of an augmentative communication intervention for adults with aphasia. Aphasiology. 2001;15:171–200. [Google Scholar]
- Fried-Oken M, Doyle M. Language representation for the augmentative and alternative communication of adults with traumatic brain injury. Journal of Head Trauma Rehabilitation. 1992;9:59–69. [Google Scholar]
- Fried-Oken M. Story telling as an augmentative communication approach for a man with severe apraxia of speech and expressive aphasia. ASHA AAC Special Interest Division Newsletter. 1995;4:3–4. [Google Scholar]
- Fried-Oken M. Augmentative and alternative communication treatment for persons with primary progressive aphasia. Perspectives on Augmentative and Alternative Communication. 2008;17:99–104. [Google Scholar]
- Fried-Oken M, Rowland C, Gibbons C. Providing augmentative and alternative communication treatment to persons with progressive nonfluent aphasia. Perspectives on Neurophysiology and Neurogenic Speech and Language Disorders. 2010;20:21–25. [Google Scholar]
- Garrett K, Beukelman D. Changes in the interaction patterns of an individual with severe aphasia given three types of partner support. Clinical Aphasiology. 1995;23:237–251. [Google Scholar]
- Garrett K, Huth C. The impact of graphic contextual information and instruction on the conversational behaviors of an individual with severe aphasia. Aphasiology. 2002;16:523–536. [Google Scholar]
- Garrett K, Lasker J. AAC for adults with severe aphasia. In: Beukelman DR, Mirenda P, editors. Augmentative & alternative communication: Supporting children & adults with complex communication needs. 3rd ed. Baltimore, MD: Paul H. Brookes Publishing Company; 2005. pp. 467–504. [Google Scholar]
- Garrett K, Beukelman D, Low-Morrow D. A comprehensive augmentative communication system for an adult with Broca’s aphasia. Augmentative and Alternative Communication. 1989;5:55–61. [Google Scholar]
- Gorno-Tempini ML, Dronkers NF, Rankin KP, Ogar JM, Phenegrasamy L, Rosen HJ, Miller BL. Cognition and anatomy in three variants of primary progressive aphasia. Annals of Neurology. 2004;55(3):335–346. doi: 10.1002/ana.10825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helm-Estabrooks N. CLQT: Cognitive Linguistic Quick Test. San Antonio, TX: The Psychological Corporation; 2001. [Google Scholar]
- Higginbotham J, Lesher G, Moulton B, Roark B. The application of natural language processing to augmentative and alternative communication. Assistive Technology. 2012;24:14–24. doi: 10.1080/10400435.2011.648714. [DOI] [PubMed] [Google Scholar]
- Ho KM, Weiss SJ, Garrett KL, Lloyd LL. The effect of remnant and pictographic books on the communicative interaction of individuals with global aphasia. Augmentative and Alternative Communication. 2005;21:218–232. [Google Scholar]
- Hodges JR, Patterson K. Nonfluent progressive aphasia and semantic dementia: A comparative neuropsychological study. Journal of the International Neuropsychological Society. 1996;2:511–524. doi: 10.1017/s1355617700001685. [DOI] [PubMed] [Google Scholar]
- Hux K, Buechter M, Wallace S, Weissling K. Using visual scene displays to create a shared communication space for a person with aphasia. Aphasiology. 2010;24:643–660. [Google Scholar]
- Hux K. Cognitive-communication deficits. In: Hux K, editor. Assisting survivors of traumatic brain injury: The role of speech-language pathologists. 2nd ed. Austin, TX: Pro-ed; 2011. pp. 121–184. [Google Scholar]
- Hux K, Weissling K, Wallace S. Communication-based interventions: AAC for people with aphasia. In: Chapey R, editor. Language intervention strategies in aphasia and related neuorgenic communication disorders. 5th ed. Baltimore, MD: Lippincott Williams & Wilkins; 2008. pp. 814–836. [Google Scholar]
- Johnson RK, Strauss Hough M, King KA, Vos P, Jeffs T. Functional communication in individuals with chronic severe aphasia using augmentative communication. Augmentative and Alternative Communication. 2008;24:269–280. doi: 10.1080/07434610802463957. [DOI] [PubMed] [Google Scholar]
- Kagan A, Simmons-Mackie N, Rowland A, Huijbregts M, Shumway E, McEwen S, Sharp S. Counting what counts: A framework for capturing real-life outcomes of aphasia intervention. Aphasiology. 2008;23:258–280. [Google Scholar]
- Keenan N, Barnhardt K. Development of yes/no systems in individuals with severe traumatic brain injuries. Augmentative and Alternative Communication. 1993;9:184–190. [Google Scholar]
- King J, Hux K. Intervention using talking word processing software: An aphasia case study. Augmentative and Alternative Communication. 1995;11:187–192. [Google Scholar]
- LaPointe L. Foundations: Adaptation, accommodation, aristos. In: LaPointe L, editor. Aphasia and related neurogenic language disorders. 3rd ed. New York: Thieme; 2005. pp. 1–18. [Google Scholar]
- Laska AC, Hellblom A, Murray V, Kahan T, Von Arbin M. Aphasia in acute stroke and relation to outcome. Journal of Internal Medicine. 2001;249:413–422. doi: 10.1046/j.1365-2796.2001.00812.x. [DOI] [PubMed] [Google Scholar]
- Lasker J, Garrett K, Fox L. Severe aphasia. In: Beukelman DR, Garrett K, Yorkston K, editors. Augmentative Communication for Adults with Acute or Chronic Medical Conditions. Baltimore, MD: Paul H. Brookes Publishing Company; 2007. pp. 163–206. [Google Scholar]
- Lasker JP, LaPointe LL, Kodras J. Helping a professor with aphasia resume teaching through multimodal approaches. Aphasiology. 2005;19:399–410. [Google Scholar]
- Lasker J, Hux K, Garrett K, Moncrief E, Eischeid T. Variations on the Written Choice Communication strategy for individuals with severe aphasia. Augmentative and Alternative Communication. 1997;13:108–116. [Google Scholar]
- Light JC, Beesley M, Collier B. Transition through multiple augmentative and alternative communication systems: A three-year case study of a head injured adolescent. Augmentative and Alternative Communication. 1988;4:2–14. [Google Scholar]
- Chapey R, Duchan J, Elman R, Garcia L, Kagan A, Lyon J, Simmons-Mackie N. LPAA Project Group. Life participation approach to aphasia: A statement of values. In: Chapey R, editor. Language intervention strategies in adult aphasia. Baltimore, MD: Williams & Wilkins; 2001. pp. 246–268. [Google Scholar]
- Lyon JG. Communicative drawing: An augmentative mode of interaction. Aphasiology. 1995a;9:84–94. [Google Scholar]
- Lyon JG. Drawing: Its value as a communication aid for adults with aphasia. Aphasiology. 1995b;9:33–50. [Google Scholar]
- McKelvey M, Hux K, Dietz A, Beukelman DR. Impact of personal relevance and contextualization on word-picture matching by people with aphasia. American Journal of Speech-Language Pathology. 2010;19:22–33. doi: 10.1044/1058-0360(2009/08-0021). [DOI] [PubMed] [Google Scholar]
- McNeil MR, Pratt SR. Defining aphasia: Some theoretical and clinical implications of operating from a formal definition. Aphasiology. 2001;15:901–911. [Google Scholar]
- Mesulam M-M. Slowly progressive aphasia without generalized dementia. Annals of Neurology. 1982;11:592–598. doi: 10.1002/ana.410110607. [DOI] [PubMed] [Google Scholar]
- Mesulam MM. Primary progressive aphasia. Annals of Neurology. 2001;49:425–432. [PubMed] [Google Scholar]
- Murray L. Longitudinal treatment of primary progressive aphasia: A case study. Aphasiology. 1998;12(7/8):651–672. [Google Scholar]
- National Aphasia Association. Aphasia Frequently Asked Questions. 2009 Retrieved July 22, 2011, http://aphasia.org/Aphasia_Facts/aphasia_faq.html.
- Neary D, Snowden J, Gustafson L, Passant U, Stuss D, Black S, Benson DF. Frontotemporal lobar degeneration: A consensus on clinical diagnostic criteria. Neurology. 1998;51:1546–1554. doi: 10.1212/wnl.51.6.1546. [DOI] [PubMed] [Google Scholar]
- Raghavendra P, Bornman J, Granlund M, Bjorck-Akesson E. The World Health Organization’s international classification of functioning, disability and health: Implications for clinical and research practice in the field of augmentative and alternative communication. Augmentative and Alternative Communication. 2007;23:349–361. doi: 10.1080/07434610701535905. [DOI] [PubMed] [Google Scholar]
- Rogers MA, Alarcon NB. Dissolution of spoken language in primary progressive aphasia. Aphasiology. 1998;12:635–650. [Google Scholar]
- Rogers MA, King J, Alarcon N. Proactive management of primary progressive aphasia. In: Beukelman D, Yorkston KM, Reichle J, editors. AAC for adults with acquired neurological disorders. Baltimore: Paul H Brookes; 2000. pp. 305–337. [Google Scholar]
- Rowland C, Fried-Oken M, Steiner SAM, Lollar D, Phelps R, Simeonsson R, Granlund M. Developing the ICYCY for AAC Profile and code set for children who rely on AAC. Augmentative & Alternative Communication. 2012;28:21–32. doi: 10.3109/07434618.2012.654510. [DOI] [PubMed] [Google Scholar]
- Shane H, Blackstone S, Vanderheiden G, Williams M, DeRuyter F. Using AAC technology to access the world. Assistive Technology. 2012;24:3–13. doi: 10.1080/10400435.2011.648716. [DOI] [PubMed] [Google Scholar]
- Simmons-Mackie N. Social approaches to aphasia intervention. In: Chapey R, editor. Language intervention strategies in adult aphasia. Baltimore, MD: Williams & Wilkins; 2001. pp. 246–268. [Google Scholar]
- Simmons-Mackie N, Kagan A. Application of the ICF in aphasia. Seminars in Speech and Language. 2007;28:244–253. doi: 10.1055/s-2007-986521. [DOI] [PubMed] [Google Scholar]
- Trautman J, Ourand P, Bardach L, Vess T, Caves K, DeRuyter F. Patient’s clinical pathway for communication changes with ALS. Retrieved July 28. 2002;2011 http://aac-rerc.psu.edu/index.php/files/list/type/1. [Google Scholar]
- Wallace S, Hux K, Beukelman DR. Navigation of a dynamic screen AAC interface by survivors of severe traumatic brain injury. Augmentative and Alternative Communication. 2010;26:242–254. doi: 10.3109/07434618.2010.521895. [DOI] [PubMed] [Google Scholar]
- Wilson SM, Henry ML, Besbris M, Ogar JM, Dronkers NF, Jarrold W, Gorno-Tempini ML. Connected speech production in three variants of primary progressive aphasia. Brain. 2010;133:2069–2088. doi: 10.1093/brain/awq129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (WHO) International classification of functioning, disability and health (ICF) Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- Yorkston KM, Beukelman DR. Decision making in AAC intervention. In: Beukelman D, Yorkston KM, Reichle J, editors. Augmentative and Alternative Communication for Adults with Acquired Neurological Disorders. Baltimore, MD: Paul H. Brookes Publishing Co.; 2000. pp. 55–82. [Google Scholar]