Abstract
Multiple myeloma involving the thyroid cartilage is a very uncommon disease entity. Only 10 cases have been reported in the international literature to date and as such it constitutes a rare and challenging diagnosis to make. We report the case of a 63-year-old man with a background of malignant melanoma and multiple myeloma both of which were in remission at the time of presentation. The patient presented with hoarseness and a large neck mass that turned out to be an extramedullary deposit of his previously treated multiple myeloma indicating disease relapse. The differential diagnosis of a mass in the thyroid cartilage is discussed. Despite its rarity, this diagnosis should be considered even in patients with no history of multiple myeloma, as it can arise de-novo in the thyroid cartilage (extramedullary plasmacytoma). The importance of the multidisciplinary team (MDT) approach as well as recent advances in treatment are also discussed.
Background
Multiple myeloma involving the thyroid cartilage is a very uncommon disease entity. Only 10 cases have been reported in the international literature to date and as such it constitutes a rare and challenging diagnosis.1–10 We present a case of extramedullary relapse of multiple myeloma involving the thyroid cartilage, discuss the differential diagnosis of such a neck mass and illustrate modern therapeutic approaches.
Case presentation
A 63-year-old man was referred to the otorhinolaryngology—head and neck surgery clinic with a 1-month history of hoarseness and an expanding midline neck mass. He had a medical history of multiple myeloma diagnosed 3 years previously which was currently in remission. Moreover, he had a superficial spreading malignant melanoma excised from his back 7 years ago and there had been no sign of recurrence. He had no other significant medical or family history. The patient also had a history of heavy smoking, though had quit smoking 2 years prior to his presentation.
On clinical examination, there was a 5 cm hard mass fixed to the left hemilarynx. There was no associated cervical lymphadenopathy and the thyroid gland felt normal on palpation. Fibreoptic laryngoscopy performed in the ear, nose and throat (ENT) clinic revealed a bulging left false vocal fold with an obliterated ipsilateral laryngeal ventricle. The overlying mucosa appeared normal.
Investigations
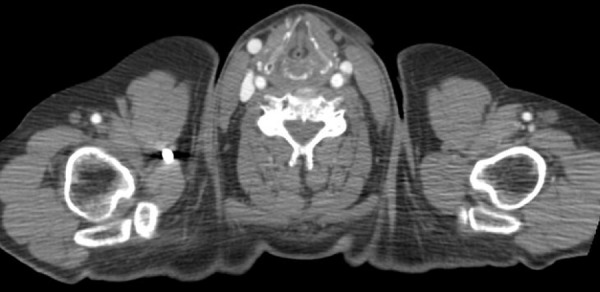
A CT confirmed the presence of a 28×15×45 mm mass consisting of enhancing abnormal tissue with central necrosis. The mass had caused complete destruction of the ipsilateral thyroid lamina which had been totally replaced by the tumour (figure 1). The tissue bulged into the paraglottic space displacing the left true vocal fold and narrowing the rimma glottidis. There was no pathological lymphadenopathy and the rest of the cervical region (including the thyroid gland) and thorax appeared normal.
Figure 1 .
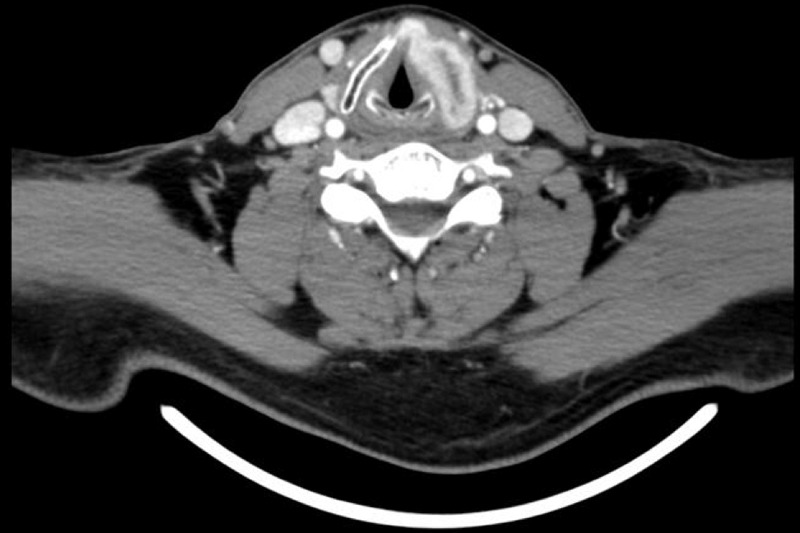
CT of the neck showing the left thyroid lamina completely replaced with avidly enhancing abnormal tissue with central necrosis.
On direct laryngoscopy under general anaesthesia, deep biopsies were obtained from the bulging supraglottic area and left false vocal fold. The overlying mucosa appeared normal (figure 2). In addition, a transcutaneous trucut biopsy of the laryngeal mass was performed to ensure adequate and representative tissue would be available for histopathological examination.
Figure 2 .
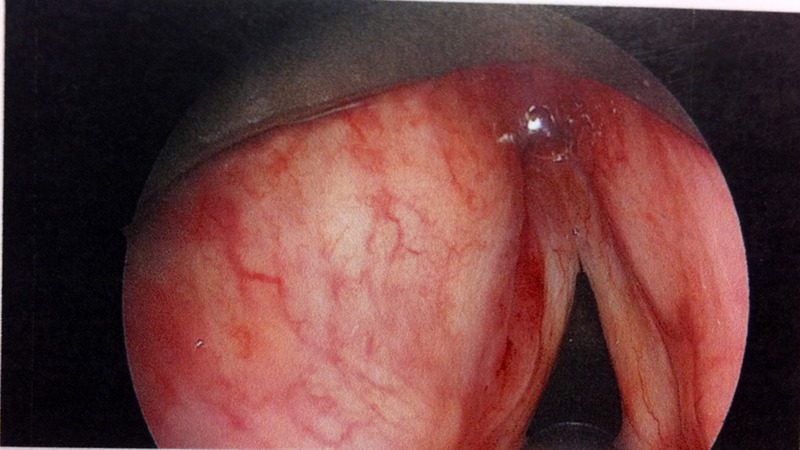
Direct laryngoscopy showing a bulging left false vocal fold with an obliterated ipsilateral laryngeal ventricle. The overlying mucosa appears normal.
Hisptopathological examination of the specimens revealed a heavy diffuse infiltrate of cytologically atypical plasma cells. The latter expressed the plasma cell markers CD138 and CD79a as well as CD56, with κ light chain restriction on immunohistochemistry (figures 3 and 4). These were consistent with laryngeal involvement from the patient's previously diagnosed multiple myeloma.
Figure 3 .
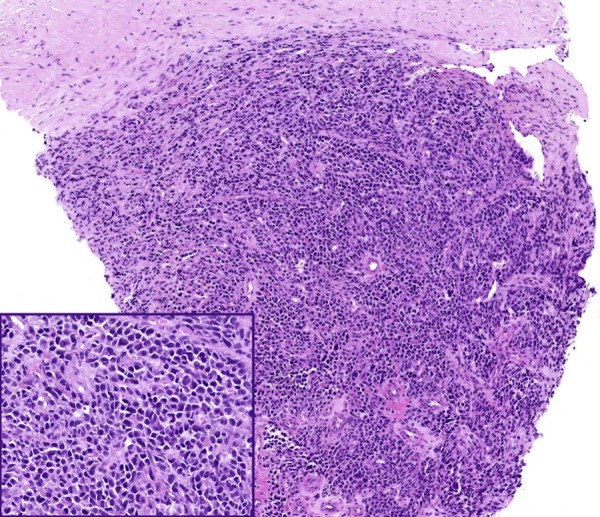
Laryngeal biopsy showing a diffuse infiltrate of atypical plasma cells. Inset shows high power view of atypical plasma cells.
Figure 4 .
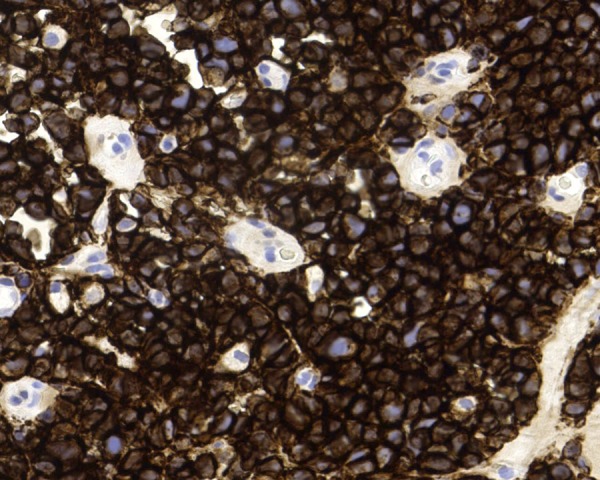
CD138 immunostain showing strong diffuse expression by atypical plasma cells.
Differential diagnosis
In view of the radiological appearance of the mass, a metastatic deposit from his previous malignant melanoma or multiple myeloma deposit were suspected as the most likely diagnoses. A primary tumour of the thyroid cartilage such as a chondroma or chondrosarcoma was also considered as the mucosa appeared to be spared endoscopically. In view of the site of the lesion and the patient's age and long history of heavy smoking, a squamous cell carcinoma of the larynx also had to be considered although in view of the mucosal sparring and absence of cervical lymphadenopathy this diagnosis was less likely. Another possibility was an anaplastic thyroid carcinoma infiltrating the thyroid cartilage but this was also unlikely as the thyroid gland was normal on both clinical examination and CT imaging of the neck.
Treatment
Following discussion in the Head & Neck Oncology Multidisciplinary Team Meeting, the patient was referred back to the haematology team and was jointly treated by the haematology and oncology teams. The patient was started on chemotherapy with Revlimid (lenalidomide) in conjunction with external beam radiotherapy to the larynx.
Outcome and follow-up
The patient responded well to the treatment and the mass rapidly regressed. Indeed, on his follow-up CT scan there was complete resolution of the previously heavily enhancing mass in the left thyroid lamina (figure 5). He is currently in remission and under close follow-up by both the haematology and oncology teams.
Figure 5 .
CT of the neck post-treatment showing complete resolution of the previously heavily enhancing mass in the left thyroid lamina.
Discussion
A mass in the thyroid cartilage involves a long list of differential diagnoses. In the older patient and where a significant smoking history is present, it should be assumed to be malignant until proven otherwise.
Both primary and secondary malignancies can present as a laryngeal mass. Squamous cell carcinoma is the commonest primary malignancy of the larynx, and thus the most likely diagnosis. Indeed, direct invasion of the thyroid cartilage from a glottic or supraglottic squamous cell carcinoma (SCC) is a common phenomenon.11 Direct invasion from a thyroid gland neoplasm is also likely and must always be considered. Anaplastic thyroid cancer is a particularly aggressive tumour, with local invasion present in 90% of patients at the time of diagnosis. It is therefore likely to invade directly the thyroid cartilage and present as a mass in that region.12 Alternative diagnoses include primary neoplasms of the thyroid cartilage such as a chondroma13 or more rarely chondrosarcoma.14
On the other hand, a mass in the thyroid cartilage could represent a metastatic deposit. Metastases in the thyroid cartilage have been described to originate from a number of primary sites including the bronchus15 and prostate.16 Metastasis from malignant melanoma is another important differential to be considered, especially in this case where there was relevant medical history.17
Multiple myeloma accounts for 80% of plasma cell malignancies.18 It is characterised by the deposit of neoplastic plasma cells in the bone marrow as well as extramedullary sites (plasmacytoma). However, the latter is uncommon and present in only 4.6% of patients with multiple myeloma with the commonest extramedullary sites being the lungs, liver and upper respiratory tract.19
Multiple myeloma affecting the larynx is an uncommon entity. It has been reported in the literature, but the sites involved appear to mainly include the glottis and supraglottis.20 There has been one documented case of an extramedullary plasmacytoma (EMP) of the thyroid cartilage.21 There are two cases reporting multiple myeloma initially presenting as a solitary EMP of the thyroid cartilage4 8 and eight additional cases reporting multiple myeloma involving the thyroid cartilage.1–3 5–7 9 10 These invariably present with a neck mass causing compressive symptoms including stridor, hoarseness and dysphagia.7 9 10
Typical radiological features of EMP of the thyroid cartilage on CT include calcification and areas of low density within the thyroid cartilage.8 9
When biopsying such a lesion it is paramount to take a deep biopsy as 80% of EMPs will be submucosal.18
The diagnosis of multiple myeloma depends on neoplastic plasma cell bone marrow infiltration, medullary or extramedullary plasma cell masses and characteristic paraproteins. Monoclonal antibodies for κ and λ chains can be used enabling the tumour to be subclassified. Bone lesions can be screened for by performing a skeletal survey with MRI or bone scintigram. Also typically in multiple myeloma, the characteristic Bence-Jones paraproteins are found in the urine.22
Once the diagnosis has been made, the course of treatment should be decided in a MDT setting. The approach to treatment in this case can be regarded as systemic treatment for the multiple myeloma and local treatment for the extramedullary lesion in the thyroid cartilage.
With regard to systemic treatment, the patient was treated with Revlimid (lenalidomide) which is an immunomodulatory, thalidomide-related drug, newly licensed for multiple myeloma and shown to improve survival rates.23
In relation to local treatment, there are two possible options—surgical excision and external beam radiotherapy. Often complete surgical excision is not possible, due to the close proximity of other important structures which can leave the patient with considerable postoperative morbidity (eg, dysphonia, swallowing and/or aspiration problems). External beam radiotherapy has been shown to be effective in the management of plasmacytomas in the head and neck and a combination of these modalities gives the best prognosis.21
Learning points.
Multiple myeloma involving the thyroid cartilage is a rare diagnosis but should be considered in the differential diagnosis of a midline neck mass.
When biopsying such a lesion deep biopsies must be taken as the disease may be submucosal.
Recent advances in treatment mean patients with multiple myeloma have a better prognosis than previously expected.
Acknowledgments
The authors would like to thank Dr Marium Khan, Consultant Histopathologist for her help with the immunohistochemistry photomicrographs.
Footnotes
Contributors: HKM and GG: Conception of idea, reviewed literature and co-wrote the manuscript. NM and JM: Reviewed and corrected the manuscript.
Competing interests: None.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Kumar N, Pandey AN, Kashyap R, et al. Extramedullary relapse in a case of multiple myeloma involving the thyroid cartilage: case report and review of literature. Indian J Surg Oncol 2011;2013:313–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kalina P, Rykken JB. Multiple myeloma of the thyroid cartilage. Case Rep Hematol 2012;2013:194797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saad R, Raab S, Liu Y, et al. Plasmacytoma of the larynx diagnosed by fine-needle aspiration cytology: a case report. Diagn Cytopathol 2001;2013:408–11 [DOI] [PubMed] [Google Scholar]
- 4.Aslan I, Yenice H, Baserer N. An indolent course of multiple myeloma mimicking a solitary thyroid cartilage plasmacytoma. Eur Arch Otorhinolaryngol 2002;2013:84–6 [DOI] [PubMed] [Google Scholar]
- 5.Brandmaier P, Kahn T, Stumpp P. [Extraosseous myeloma manifestation of the thyroid cartilage]. Rofo 2011;2013:477–8 [DOI] [PubMed] [Google Scholar]
- 6.Dispenza F, Sciandra D, Saraniti C. Thyroid cartilage involvement in patient affected by IgA multiple myeloma: case report. Auris Nasus Larynx 2008;2013:288–90 [DOI] [PubMed] [Google Scholar]
- 7.Gross M, Eliashar R, Petrova P, et al. Neck mass as primary manifestation of multiple myeloma originating in the thyroid cartilage. Otolaryngol Head Neck Surg 2002;2013:326–8 [DOI] [PubMed] [Google Scholar]
- 8.Shimada T, Matsui M, Ikebuchi K,et al. Multiple myeloma involving the thyroid cartilage. Auris Nasus Larynx 2007;2013:277–9 [DOI] [PubMed] [Google Scholar]
- 9.Sosna J, Slasky BS, Paltiel O, et al. Multiple myeloma involving the thyroid cartilage: case report. AJNR Am J Neuroradiol 2002;2013:316–18 [PMC free article] [PubMed] [Google Scholar]
- 10.Van Dyke CW, Masaryk TJ, Lavertu P. Multiple myeloma involving the thyroid cartilage. AJNR Am J Neuroradiol 1996;2013:570–2 [PMC free article] [PubMed] [Google Scholar]
- 11.Chen SA, Muller S, Chen AY,et al. Patterns of extralaryngeal spread of laryngeal cancer: thyroid cartilage penetration occurs in a minority of patients with extralaryngeal spread of laryngeal squamous cell cancers. Cancer 2011;2013:5047–51 [DOI] [PubMed] [Google Scholar]
- 12.Cornett WR, Sharma AK, Day TA,et al. Anaplastic thyroid carcinoma: an overview. Curr Oncol Rep 2007;2013:152–8 [DOI] [PubMed] [Google Scholar]
- 13.Schittek A, James AG. Chondroma of the larynx. J Surg Oncol 1982;2013:176–8 [DOI] [PubMed] [Google Scholar]
- 14.Jones DA, Dillard SC, Bradford CR, et al. Cartilaginous tumours of the larynx. J Otolaryngol 2003;2013:332–7 [DOI] [PubMed] [Google Scholar]
- 15.Lee JK, Yoon TM, Kim HD,et al. Thyroid cartilage metastasis from the lung. J Otolaryngol Head Neck Surg 2008;2013:E183–7 [PubMed] [Google Scholar]
- 16.Escudero RM, Amo FH, Martinez MC,et al. Metastatic prostate cancer on the thyroid cartilage: unusual symptoms of prostatic adenocarcinoma. Case report . Arch Esp Urol 2011;2013:132–5 [PubMed] [Google Scholar]
- 17.Nicolai P, Puxeddu R, Cappiello J,et al. Metastatic neoplasms to the larynx: report of three cases. Laryngoscope 1996;2013:851–5 [DOI] [PubMed] [Google Scholar]
- 18.Garas G, Choudhury N, Prasad N, et al. Extramedullary plasmacytoma of the tongue base. JRSM Short Rep 2010;2013:60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Damaj G, Mohty M, Vey N,et al. Features of extramedullary and extraosseous multiple myeloma: a report of 19 patients from a single center. Eur J Haematol 2004;2013:402–6 [DOI] [PubMed] [Google Scholar]
- 20.Rolins H, Levin M, Goldberg S, et al. Solitary extramedullary plasmacytoma of the epiglottis: a case report and review of the literature. Otolaryngol Head Neck Surg 1995;2013:754–7 [DOI] [PubMed] [Google Scholar]
- 21.Sasaki R, Yasuda K, Abe E, et al. Multi-institutional analysis of solitary extramedullary plasmacytoma of the head and neck treated with curative radiotherapy. Int J Radiat Oncol Biol Phys 2012;2013:626–34 [DOI] [PubMed] [Google Scholar]
- 22.Raab MS, Podar K, Breitkreutz I, et al. Multiple myeloma. Lancet 2009;2013:324–39 [DOI] [PubMed] [Google Scholar]
- 23.Morgan GJ, Krishnan B, Jenner M, et al. Advances in oral therapy for multiple myeloma. Lancet Oncol 2006;2013:316–25 [DOI] [PubMed] [Google Scholar]


